The Female Reproductive System
advertisement
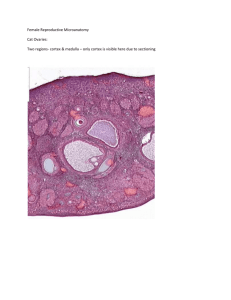
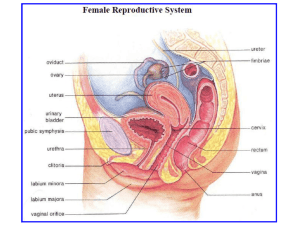
The Female Reproductive System The female reproductive system consists of the two ovaries, two oviducts, uterus, vagina and external genetalia. Although the mammary glands don't belong to the genital system(is amodified sweat gland located within subcutaneous tissue) are included in this classification because they undergo changes directly connected to the functional state of the reproductive system. The Ovary : The ovaries are classified as a double glands since they produce both exocrine (cytogenic ) and endocrine secretions . Ovaries are almond-shaped bodies approximately 4cm long ,2cm wide and 1cm thick . One lies on each side of the uterus on the lateral wall of the pelvic cavity. Each is attached to the broad ligament of the uterus at its margin the hilum by a fold of peritoneum called the mesovarium. At the hilum, the vascular con.t of mesovarium continuous with the ovarian stroma. The free surface of the ovary is covered by alayer of cuboidal cells the germinal epithelium. Beneath the epi there is apoorly delineated layer of dense con.t the tunica albuginea which increase in density with advancing age. In sections of the ovary , two zones may be distinguished , an outer layer the cortex , and an inner portion the medulla which merges with the vascular con.t of the mesovarium at the hilum. There is no distinct line of demarcation between the two zones. The medulla consists of loose fibroblastic con.t containing numerous large blood vessels , lynmphatics and nerves. The stroma contains scattered strands of smooth muscle fibers. The cortex consists of a compact, cellular stroma that contains the ovarian follicles. The follicles may be seen in all stages of development, and the appearance of the cortex depends upon the age of the individual and the stage of the ovarian cycle. Before puberty only primordial follicles are seen. Sexual maturity is characterized by the presence of growing follicles and their end products (corpus luteum , atretic follicles). After menopause, follicles disappear and the cortex become a narrow zone of fibrous con.t . Follicular Growth and Development : Primordial follicles : Consists of an immature ovum surrounded by a single flattened layer of epithelial (follicular) cells . A thin basal lamina separates the follicle from ovarian stroma. The immature ovum,the primary oocyte is aspheroidal cell with a large vesicular nucleus and a prominent nucleolus. The cytoplasm is finely granular. In the newborn infant , the number of follicles a bout 400,000, but most of them will disappear during the reproductive years. Growing Follicles : The progressive development of follicles that occur after puberty is characterized by growth and differentiation of the ovum, proliferation of follicular cells and development of a con t from surrounding stroma. The immature ovum increase in size, the nucleus enlarge. Mitochondria increase in number, the endoplasmic reticulum hypertrophies and the Golgi complexes migrate to just beneath the cell surface. The zona pellucida , are a refractile, deeply staining membrane is formed around the oocyte, it contains glycoproteins and appear homogenous in fresh condition. The flattened follicular cells become first cuboidal and then columnar in shape and the follicle is called aunilaminar primary follicle. Follicular cell proliferate by mitosis and form a stratified follicular epi or granulose layer. The follicle is called a multilaminar primary follicle. The proliferation occur more rapidly on one side of the ovum , so that the follicle become ovoid in shape and the ovum eccentric in position. Irregular small spaces filled with a clear fluid appear within the follicular mass. An increase in the amount of the fluid causes a further increase in the size of follicle. The small spaces fuse to form a single cavity , the antrum which filled with liquor folliculi, aviscid fluid rich in hyaluronic acid. The ovum surrounded by a group of follicular cells, is pressed to one side and form a definite projection into the antrum cavity , this eccentric mound is known the cumulus oophorus . The follicular cells of the cumulus oophorus directly in relation to the ovum become radially arranged and form the corona radiata. The stratified epi, composed of follicular cells ,form acontinuos regular layer around the antrum cavity , the membrane granulose. As the follicle increase in size , the adjacent stroma organizes into a capsule the theca folliculi , this differentiate into two layers , an inner vascular layer the theca interna and an outer fibrous layer the theca externa. Theca interna consists of enlarged stromal cells between which are numerous capillaries. Theca externa composed of closely packed collagenous fibers and fusiform cells. Mature Graafian Follicle : The follicle require 10-14 days to reach maturity , and is about 10mm or more in diameter. It bulge on the free surface of the ovary . At this point ,called the stigma , the tunica albuginea & the theca folliculi become attenuated .The large antrum ,distended with fluid . the ovum has attained its full size, and surrounded by thick zona pellucid & a clear corona radiate. Small irregular spaces occur between the cells of cumulus oophorus thus weakening the connection of the ovu with membrane granulosa. As te follicle reach maturity, there is increased secretion of liquid more watery than that formed previously. This is called preovulatory swelling. The follicle ruptures at the stigma, and follicular fluid released into the peritoneal cavity . The ovum with its corona radiate leaves the ovary this process is the ovulation. The free ovum retains the capacity to be fertilized only for (24) hours In human female , ovulation occur at intervals average 28 days. The Corpus Luteum : After ovulation , the wall of follicle collapses and thrown into folds. The follicular wall transformed into a temporary glandular structure the corpus luteum. The cells of membrane granulose differentiate into large pale-staining cells with large vesicular nuclei. The cytoplasm contains accumulation of fine lipid droplets. The transformed granulose cells are called granulose lutein cells and they form a thick folded layer around the remains of follicular cavity. Cells of theca interna increased in size and form theca lutein cells ,they are smaller in size than granulose lutein cells and have compact dark-staining nuclei. The theca externa do not undergo transformation. If the ovum is not fertilized , the corpus luteum attains its greatest development about (9 days) after ovulation and then degenerate ,this the corpus luteum of menstruation. If the ovum is fertilized , the corpus luteum increase in size and is known the corpus luteum of pregnancy. The cells continue to grow in size until the middle mouths of pregnancy, and thereafter slow involution occur. After delivery, involution proceeds rapidly. The resulting corpus albicans is large and causes a retraction the surface of the ovary. The Fallopian Tube : Uterine tubes or oviducts, are paired structures extend from the ovary to the uterus in a fold of peritoneum ,the upper free margin of the broud ligament. Each is 12-15cm long and 1cm in diameter . The end in relation to ovary opens into peritoneal cavity the other end opens into the uterine cavity . The uterine tube shows four regions : The infundibulum , is funnel-shaped opening into the peritoneal cavity . Its margins have numerous frnged folds (fimberia). 2- The expanded intermediate segment the ampulla comprising the two third of tube and it has thin walled. 3- isthmus , slender & narrow connect with the uterus . 4-Intramural portion is the continuation of the canal through the uterine wall. The wall of uterine tube consists of 1- mucous membrane 2- a muscular layer and 3- a serosa. Mucosa : The mucosa has longitudinal folds that are most numerous in ampulla and branched in a complex manner. In isthmus ,the folds rarly branch . in the intramural portion, the folds are low. The epithelium consists of simple columnar cells, contains two types of cells. One has cilia, the other is secretory. The nonciliated cells are narrow and peg-shaped and secretory in nature, contributing nutritive materials for ovum. Ciliated cells occur in small groups alternating with groups of nonciliated cells. The proportion of cells with cilia is greatest at the infundibulum, and least at the isthmus. The cilia play important role in transport of the ovum through the ampulla to the ampullo-isthmic junction ,the normal site of fertilization. The lamina propria is composed of loose con.t. The muscularis consists of a broad inner circular and a thin outer longitudinal. The outer sheath is the serosa consisting of a loose con.t with mesothelium. The Uterus : Is a pear-shaped organ ,consists of two major portions 1- The expanded upper portion the body or corpus uteri 2- The lowermost, cylindrical portion, the neck or cervix , which projects into vagina.The terms fundus refers to the rounded upper end of the body, from which extend the oviducts . The isthmus is the narrow zone of transition between the body & the cervix. The wall of the uterus consists of three layers : 1-The outer layer, the serosa or perimetrium. Consisting of a single layer of mesothelial cells supported by a thin layer of con.t. 2- The middle layer , the muscularis or myometrium : Is the tnickest layer o uters , composed of bundles of smooth muscle fibers separated by con. The muscle fibers are large and their length varies from (40-90µm) . During pregnancy , the fibers increase greatly in size and reach (600 µm) as aresult of hypertrophy , and also increase in number (hyperplasia). The bundles of smooth muscle fibers form three poorly defined layers. An inner & outer layers are arranged longitudinally . The middle layer circularly arranged and contains larger blood vessels. 3- The inner layer the mucosa or endometrium : Consists of simple columnar epi and the lamina propria containing simple tubular gland that sometimes branch in their deeper portions. The epithelial cells are a mixture of of ciliated and secretory simple columnar cells. The epi of glands is similar to the superficial epi but ciliated cells are rare within the glands . Stromal cells of the lamina prporia resemble mesenchymal cells are stellate in shape with large ovoid nucleus. The endometrial layer can be subdivided into two zones; the functionalis which constitute the portion sloughed off at menstruation and replaced during each menstrual cycle and the basalis , the portion retained after menstruation that subsequently proliferate and provid a new epi and lamina propria for renewal of endometrium . Cyclic Changes In the Endometrium : The endometrium subject to cyclic changes in response to ovarian secretory activities. Three stages can be recognized in a continuous cycle of events. Menstrual stage is defined as the first to fourth days of the cycle .(1-4) Proliferative stage is the fifth to fourteenth days. (5-14) Secretory or luteal stage is the fifteenth to twenty-eight days. (15-28) 1--The proliferative (Follicular) stage : This stage begins at the end of a menstrual flow and is characterized by rapid regeneration of the endometrium from narrow zone remaining after menstruation . The mucosa increases in thickness from from (1mm or less) to (2mm or more). This increase coincides with growth of ovarian follicles and secretion of estrogen. The glands proliferate , increase in length and become closely packed . Rebuilding of lamina propria . Toward the end of this stage , the lumen of the gland s widen, and only a thin mucoild secretion is released at this stage. Coild arteries grow into the regenerating tissue but are not found in the superficial third of the endometrium. 2- The Progestational (secretory or luteal) stage : This stage start after ovulation in response to formation of the corpus luteum , which secretes progesterone. The endometrium Increase in thickness to 4mm or more as a result of a ccumulation of secretions and the edema of the stroma. The glands swell and secrete profusely. The secretion is thick and rich in glycogen. . The elongation and convolution of the coild artery continue , and extend into the superficial of the endometrium. 3- The menstrual stage : When fertilization of the ovum not occur , the corpus luteum ceases functioning after about 14 days . The level of progesterone and estrogen in the blood drop rapidly. At the end of secretory stage , the wall of coiled artey contract , closing off the blood and the functional layer become pale asaresult of anemia and anoxia which leads to death of their walls . The functional layer undergoes necrosis and is shed. After a number of hours, the walls of vessels near the surface break and the blood is added to the secretion of the glands and the necrotic endometrial tissue.