case report a case of antiphospholipid syndrome for open
advertisement
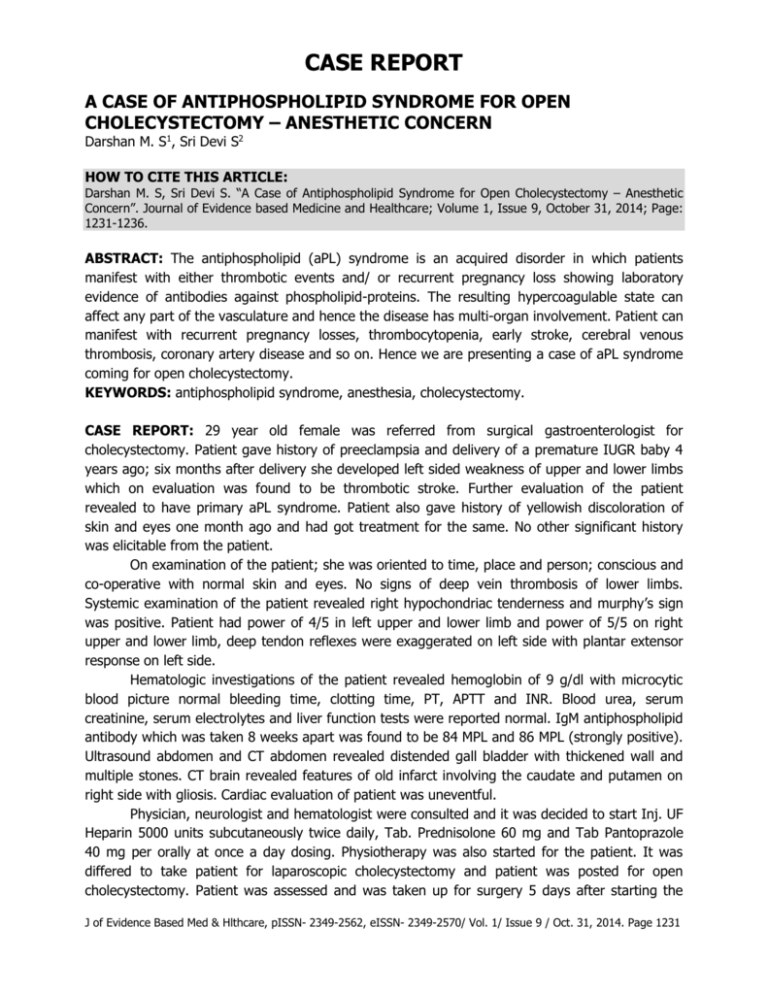
CASE REPORT A CASE OF ANTIPHOSPHOLIPID SYNDROME FOR OPEN CHOLECYSTECTOMY – ANESTHETIC CONCERN Darshan M. S1, Sri Devi S2 HOW TO CITE THIS ARTICLE: Darshan M. S, Sri Devi S. “A Case of Antiphospholipid Syndrome for Open Cholecystectomy – Anesthetic Concern”. Journal of Evidence based Medicine and Healthcare; Volume 1, Issue 9, October 31, 2014; Page: 1231-1236. ABSTRACT: The antiphospholipid (aPL) syndrome is an acquired disorder in which patients manifest with either thrombotic events and/ or recurrent pregnancy loss showing laboratory evidence of antibodies against phospholipid-proteins. The resulting hypercoagulable state can affect any part of the vasculature and hence the disease has multi-organ involvement. Patient can manifest with recurrent pregnancy losses, thrombocytopenia, early stroke, cerebral venous thrombosis, coronary artery disease and so on. Hence we are presenting a case of aPL syndrome coming for open cholecystectomy. KEYWORDS: antiphospholipid syndrome, anesthesia, cholecystectomy. CASE REPORT: 29 year old female was referred from surgical gastroenterologist for cholecystectomy. Patient gave history of preeclampsia and delivery of a premature IUGR baby 4 years ago; six months after delivery she developed left sided weakness of upper and lower limbs which on evaluation was found to be thrombotic stroke. Further evaluation of the patient revealed to have primary aPL syndrome. Patient also gave history of yellowish discoloration of skin and eyes one month ago and had got treatment for the same. No other significant history was elicitable from the patient. On examination of the patient; she was oriented to time, place and person; conscious and co-operative with normal skin and eyes. No signs of deep vein thrombosis of lower limbs. Systemic examination of the patient revealed right hypochondriac tenderness and murphy’s sign was positive. Patient had power of 4/5 in left upper and lower limb and power of 5/5 on right upper and lower limb, deep tendon reflexes were exaggerated on left side with plantar extensor response on left side. Hematologic investigations of the patient revealed hemoglobin of 9 g/dl with microcytic blood picture normal bleeding time, clotting time, PT, APTT and INR. Blood urea, serum creatinine, serum electrolytes and liver function tests were reported normal. IgM antiphospholipid antibody which was taken 8 weeks apart was found to be 84 MPL and 86 MPL (strongly positive). Ultrasound abdomen and CT abdomen revealed distended gall bladder with thickened wall and multiple stones. CT brain revealed features of old infarct involving the caudate and putamen on right side with gliosis. Cardiac evaluation of patient was uneventful. Physician, neurologist and hematologist were consulted and it was decided to start Inj. UF Heparin 5000 units subcutaneously twice daily, Tab. Prednisolone 60 mg and Tab Pantoprazole 40 mg per orally at once a day dosing. Physiotherapy was also started for the patient. It was differed to take patient for laparoscopic cholecystectomy and patient was posted for open cholecystectomy. Patient was assessed and was taken up for surgery 5 days after starting the J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/ Issue 9 / Oct. 31, 2014. Page 1231 CASE REPORT medication. High risk informed consent was obtained from the patient. Inj. Heparin was stopped 12 hours prior to surgery. Adequate amount of blood and blood components were kept reserved. Patient was advised to take Tab. Alprazolam 0.5 mg and Tab. Metaclopromide 10 mg orally night prior to the surgery. Day before surgery Bleeding time, Clotting time, platelet count, APTT and INR were repeated and found to be normal. General anesthesia was the planned mode of anesthesia. After reassessing and reassuring the patient she was connected to multi para monitor and, ECG, Oxygen saturation (Pulse oximetry) and NIBP were monitored. Intravenous cannulation was carried out with 18G peripheral venous catheter. Baseline vitals such as pulse rate, blood pressure and oxygen saturation were recorded. Pre anesthetic check of Boyle’s apparatus was done, Ambu bag, Airway gadgets, Emergency drugs were checked and kept available. TED (thrombo embolic deterrent) stockings were applied to patient to prevent deep vein thrombosis. Patient was pre medicated with Inj. Glycopyrrolate 0.2 mg, Inj. Midazolam 2 mg and Inj. Fentanyl 100 microgram intravenously. After preoxygenating the patient for 3 minutes with 100% Oxygen, Inj. Etomidate 15 mg i.v was given for induction of the patient Inj. Vecuronium 5 mg was used to ease the intubation for the patient. A gas mixture of 1 litre of oxygen 2 litres of Nitrous oxide and 1% sevoflurane was used for maintenance of anesthesia. Inj. Hydrocortisone 100 mg was given intravenously. Inj. Dexmeditomedine 50 microgram and Inj. Ondansetron 4 mg was given 20 minutes prior to the extubation, intra operative period was uneventful and patient at the end of surgery was reversed and extubated on table. Postoperatively Inj. Dexamethasone 8 mg iv was continued at frequency of twice daily. Inj. Heparin 5000 units was restarted subcutaneously 4 hours after the surgery. On the 5th postop day patient was switched over to Tab Prednisolone 60 mg from Inj.Dexamethasone and subcutaneous heparin by Tab Warfarin 10 mg per orally. Patient was put on TED stockings till she was mobilized on second postoperative day. Patient had uneventful perioperative period and was discharged from the hospital on the seventh postoperative day. Patient was advised for a review after 4 weeks for checking adequacy of anticoagulation and we aimed to keep INR between 2-3. DISCUSSION: The antiphospholipid (aPL) syndrome is an acquired disorder in which patients manifest with either thrombotic events and/ or recurrent pregnancy loss with laboratory evidence of antibodies against phospholipid-proteins.[1] Disease has multi-organ involvement and is called secondary aPL syndrome if they are associated with any major autoimmune disorders and called primary aPL syndrome if they occur in absence of them. Deep veins of lower limbs are the common site of thrombosis, but any part of vasculature either arterial or venous system can undergo thrombosis. Also any organ can be affected because of thromboembolism. Disease mimics Thrombotic Thrombocytopenic Purpura or DIC. Antiphospholipid syndrome is also known by following synonyms, the anticardiolipin (aCL) syndrome, aPL/cofactor syndrome, antibody-mediated thrombosis syndrome and Hughes syndrome. aPL syndrome was first described by Prof. Graham R.V Hughes in 1980. ETIOLOGY: It is said to be of autoimmune etiology. And the antibody recognizes protein cofactors rather than the phospholipid itself hence known as aPL cofactor syndrome. Familial J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/ Issue 9 / Oct. 31, 2014. Page 1232 CASE REPORT clustering suggest the concept of genetically susceptible host.[2,3] Strongest association of disease with HLA-DR-53 haplotype and some association with HLA-DQ-7. Antigenic triggers noted which includes varicella, hepatitis-C, cytomegalo virus and parvo B19 virus. Cellular apoptosis occurs following viral infection and hence exposure of the anionic phospholipid on the surface triggers the generation of antibodies.[4-6] Molecular mimicry between β2GPI-related synthetic peptides and structures within bacteria, viruses, tetanus toxoid, and CMV has reportedly caused experimental aPL syndrome.[7] Pathogenesis: Annexin A5 shield disruption Altered eicosanoid synthesis Endothelial damage Induced production of endothelial cell adhesive molecules Induction of tissue factor expression on monocytes and endothelial cells Induction of apoptosis Interference with protein C pathway Antiphospholipid binding to proteins C and S Acquired activated protein C resistance Cross-reactivity with oxidized low-density lipoprotein Increase of plasminogen activator inhibitor-1 Reduced fibrinolysis by impairment of autoactivation of factor XII and by antibodies to tissue-type plasminogen activator Platelet activation Activation of complement Antibodies against tissue factor pathway inhibitor Concentration of prothrombin locally Mechanism proposed for the pathogenesis of Anti-phospholipid Syndrome[1] Arterial and venous thrombosis: DVT, thoracic abdominal and pelvic vein thrombosis. Obstetric complications: Recurrent pregnancy losses, Preeclampsia, Growth retardation, CVS manifestations: CAD, Valvular heart disease, Peripheral vascular disease CNS manifestations: Stroke, Seizure, Chorea, Migraine, GB syndrome, dementia, Acute transverse myelopathy Hematologic manifestations: Bleeding, Thrombocytopenia, Hypoprothrombinemia, Inhibition to factor VIII, Inhibition to platelet function. Cutaneous manifestations: Livedo reticularis, Necrotizing vasculitis, Livedoid vasculitis, Thrombophlebitis, Cutaneous ulceration, Necrosis, Erythematous macules, purpura, ecchymoses Respiratory manifestations: Pulmonary hypertension, Pulmonary thromboembolism, NonJ of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/ Issue 9 / Oct. 31, 2014. Page 1233 CASE REPORT inflammatory pulmonary vasculopathy GIT manifestations: Budd-Chiari syndrome, Hepatic infarction, Esophageal necrosis, Intestinal ischemia, Pancreatitis, Colonic ulceration, Primary biliary cirrhosis, Acute acalculous cholecystitis Retinal manifestation: Cilioretinal artery occlusion, Optic neuropathy, Severe vasoocclusive retinopathy Renal manifestation: aPL syndrome nephropathy Clinical presentation of aPL Diagnosing criteria has been formulated by the International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome.[8] It states that for diagnosing aPL if a minimum of one clinical and one laboratory criteria are met. Clinical o One or more episodes of vascular thrombosis o Pregnancy morbidities Laboratory o aCL IgG and/or IgM antibody present in medium or high titer on two or more occasions, at least 6 weeks apart, measured by standard ELISA for β2GPIdependent aCL antibodies Anesthetic implications: Disease being having multi-organ involvement, evaluation in terms of in-depth history from the patient, and laboratory evaluation enables to find functional status of the patient. Immobilization of the patient and venous stasis following neuraxial procedure further predispose the patient for venous thrombo-embolism (VTE.) Hence current concept of early mobilization of patient is advocated. Physical and pharmacological strategies have been used to prevent such VTE. Physical modalities like graded compression stockings and intermittent pneumatic compression devices are used with risk reduction of around 45%. Pharmacologic methods for prophylaxis against VTE are either parenteral or oral anticoagulant drugs. Heparin which is most commonly used drug has a risk reduction of 60-70%.[9] Some surgeries like ocular surgeries, dental procedures and dermatological procedures can safely be conducted without discontinuing the anticoagulation therapy. Risk benefit ratio to the patient determines whether these anticoagulant drugs need to be continued or stopped. For the patient requiring discontinuation of the anticoagulant therapy bridging therapy is initiated, if the risk of venous thromboembolism is moderate to high. Oral anticoagulation with warfarin is stopped five days prior to surgery and 36 hours after discontinuation of the drug heparin is started. Both unfractionated and fractionated forms of heparin can be used for anticoagulation. Both general and regional anesthesia can safely be initiated based on the requirements of the patient. Though regional anesthesia reduces the risk of VTE, it requires the prophylactic anticoagulant therapy. Since the patients have been put on anticoagulant drugs, for initiating neuraxial techniques guidelines by American Society of Regional Anesthesia should be followed. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/ Issue 9 / Oct. 31, 2014. Page 1234 CASE REPORT CONCLUSION: Most of the patients suffering from antiphospholipid syndrome who are undergoing surgery require a temporary interruption of the oral anticoagulant medication and need to be bridged by Inj. Heparin either fractionated or unfractionated. Patients can safely undergo both regional anesthesia and general anesthesia, adherence to the guidelines set by ASRA will help for the safe practice of regional anesthesia on such patients. REFERENCES: 1. Jacob H. Rand, The Antiphospholipid Syndrome, In: Williams Hematology, 8ed. Marshall A. Lichtman, Thomas J. Kipps, Uri Seligsohn et al, The McGraw Hill company, New York, 2010, 2145-62. 2. Sebastiani GD, Galeazzi M, Morozzi G, Marcolongo R: The immunogenetics of the antiphospholipid syndrome, anticardiolipin antibodies, and lupus anticoagulant. Semin Arthritis Rheum, 1996, 25: 414. 3. Goldstein R, Moulds JM, Smith CD, Sengar DP: MHC studies of the primary antiphospholipid antibody syndrome and of antiphospholipid antibodies in systemic lupus erythematosus. J Rheumatol, 1996, 23: 1173. 4. Eschwege V, Freyssinet JM: The possible contribution of cell apoptosis and necrosis to the generation of phospholipid-binding antibodies. Ann Med Interne Paris 1996, 147(1): 33. 5. Price BE, Rauch J, Shia MA, et al: Anti-phospholipid autoantibodies bind to apoptotic, but not viable, thymocytes in a beta 2-glycoprotein I-dependent manner. J Immunol, 1996, 157: 2201. 6. Pittoni V, Isenberg D: Apoptosis and antiphospholipid antibodies. Semin Arthritis Rheum, 1998, 28: 163. 7. Blank M, Asherson RA, Cervera R, Shoenfeld Y: Antiphospholipid syndrome infectious origin. J Clin Immunol 2004, 24: 12. 8. Wilson WA, Gharavi AE, Koike T, et al: International consensus statement on preliminary classification criteria for definite antiphospholipid syndrome: Report of an international workshop. Arthritis Rheum 1999, 42: 1309. 9. Adriana Dana Oprea, Hematologic Disorders, In: Stoelting's Anesthesia And Co-Existing Disease, 6th ed, Roberta L. Hines, Katherine E. Marschall, Elsevier Inc, Philadelphia, 2012, 407-36. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/ Issue 9 / Oct. 31, 2014. Page 1235 CASE REPORT AUTHORS: 1. Darshan M. S. 2. Sri Devi S. PARTICULARS OF CONTRIBUTORS: 1. Assistant Professor, Department of Anaesthesiology, Subbaiah Medical College, Shimoga. 2. Assistant Professor, Department of Anaesthesiology, Subbaiah Medical College, Shimoga. NAME ADDRESS EMAIL ID OF THE CORRESPONDING AUTHOR: Dr. Darshan M. S, C/o. Vasavi Clinic, M. G. Road, Chickmaglur, Karnataka 577101. E-mail: drdarshanms@gmail.com darshanms_jss@yahoo.com Date Date Date Date of of of of Submission: 15/10/2014. Peer Review: 16/10/2014. Acceptance: 27/10/2014. Publishing: 29/10/2014. J of Evidence Based Med & Hlthcare, pISSN- 2349-2562, eISSN- 2349-2570/ Vol. 1/ Issue 9 / Oct. 31, 2014. Page 1236