File
advertisement

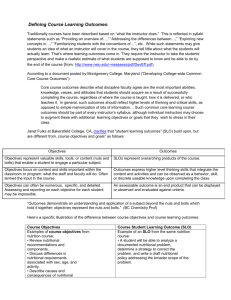
Case Study 33: Esophageal Cancer Treated with Surgery and Radiation DFM 484 Medical Nutrition Therapy Instructor: Julie Matel, MS, RD, CDE Polly Peru Rachelle Sebastian San Francisco State University October 20, 2014 Case Study 33: Esophageal Cancer Treated with Surgery and Radiation Nick Seyer is a 58 – year old man who, who after suffering from recurrent heartburn for over a year, seeks medical attention. He presents to his physician with difficulty swallowing and a significant unexplained weight loss. 1. Mr. Seyer was diagnosed with adenocarcinoma of the esophagus. What does the term adenocarcinnoma mean? Adenocarcinoma is a type of cancer that forms in mucus-secreting glands throughout the body. It can occur in many different places in the body, and is most prevalent in the following cancer types: lung, prostate, pancreatic, esophageal, and colorectal. 4. Cancer is generally treated with a combination of therapies. These can include surgical resection, radiation therapy, chemotherapy, and immunotherapy. The type of malignancy and staging of the disease will, in part, determine the types of therapies that are prescribed. Define and describe each of these therapies. Briefly describe the mechanism for each. In general, how do they act to treat a malignancy? a. Surgical Resection: A surgical resection is a surgical procedure to remove part of an organ, gland, a whole body part, tumors and some of the normal tissue around them to ensure that all of the abnormal tissue is removed. The type of resection is based on the tumor location, size, and type. Example: Surgery to remove some or most of the esophagus is called an esophagectomy and how much of the esophagus is removed depends upon the stage of the tumor and where it’s located. b. Radiation Therapy: Radiation therapy is used to shrink tumors and kill cancer cells. Highenergy radiation such as x-rays, gamma rays, and charged particles are used in the treatments. The radiation can be delivered by a machine outside of the body; come from radioactive material placed in the body near cancer cells; or in the blood to kill cancer cells. Radiation therapy destroys cancer cells by altering cellular and nuclear material, most notably DNA. Radiation therapy is most often used with surgery and/or chemotherapy. c. Chemotherapy: Chemotherapy is a form of chemical cytotoxic drug therapy that is used to destroy rapidly growing cells in the body such as cancer because cancer cells grow and divide faster than other cells. The chemotherapy drugs also destroy healthy cells in the body that rapidly divide such as bone marrow, epithelial lining of the gastrointestinal tract and hair cells. The drugs cannot tell the difference between cancer cells and normal cells. The Chemo drugs kill cells that are actively growing and dividing into new cells. Cancer cells do this more often than normal cells, so they are more likely to be killed by the treatment. Cancer cells are not as efficant at repairing themselves as normal cells. Normal cells can usually repair any damage caused by chemotherapy. The drugs that are used in the chemo treatments are usually delivered intravenously and in combinations with each other. There are many chemotherapy drugs available and the drugs used depend on the type and location of the cancer. Chemotherapy can cause many negative side effects such as vomiting, loss of appetite, neutropenia, anemia, diarrhea, mucositis, and hair loss. Immunotherapy: Immunotherapy is a treatment that uses our own immune system to fight cancer and other diseases. There are a couple of ways that Immunotherapy acts to kill cancer; 1) the stimulation of our own immune system to work harder to attack cancer cells; 2) an individual receives man-made immune system protein components. 6. Many cancer patients experience changes in nutritional status. Briefly describe the potential effect of cancer on nutritional status. Cancer and the treatments used to kill it can cause many metabolic alterations that can have negative effects on an individual’s nutritional status which can lead to malnutrition. Cancer patients may experience mucositis, anemia, nausea, vomiting, dysgeusia, diarrhea, constipation,early satiety, xerostomia, neutropenia, and weight loss. These metabolic alterations can cause severe anorexia and cachexia that may not be amenable to common nutritional interventions (Nelms, 2011, pg. 718). 7. Both surgery and radiation affect nutritional status. Describe potential nutritional and metabolic effects of these treatments. Both surgery and radiation affect nutritional status. Radiation therapy targets localized cancerous cells but it can negatively affect surrounding cells. Side effects of radiation therapy to the head and neck area include fatigue, mucositis, dysgeusia, xerostomia secondary to salivary gland destruction, dysphagia, odynophagia, and severe esophagitis. Radiation treatment to the abdominal and pelvic area can result in radiation enteritis. Symptoms include abdominal pain, severe diarrhea, malabsorption, and lactose intolerance. Patients undergoing cancer surgery experiences significant and long-term nutritional side effects. Surgical procedures may potentially change an individual’s physical appearance, alter organ function (esophagectomy), or both which can contribute to reduced food intake and weight loss. Surgical treatments for esophageal cancer can significantly delay recovery of oral intake, and often patients require placement of a jejunal feeding tube during surgery. Moreover, the patient is at high risk of dehydration due to inadequate fluid intake, and may need intravenous (I.V.) fluids for hydration and electrolyte correction because the esophageal tissue may become extremely irritated and fragile. A surgically placed feeding tube can increase the risk of bleeding from the fragile nature of the esophagus. In addition, the esophagus may be totally or partially obstructed by the tumor mass, which prevents placement of a feeding tube. 8. Calculate and evaluate Mr. Seyer’s %UBW and BMI. BMI: (198/ (75 x 75) x 703 = 24.7 %UBW: 198/230 x 100 = 86% Mr. Seyer’s BMI is in the normal Body Mass Index range and his Percent Usual Body Weight indicates that he has lost 14% of his body weight in approximately six months. 9. Summarize your findings regarding his status. Classify the severity of his weight loss. What factors may have contributed to his weight loss? Explain. Mr. Seyer stated that his 30lb unintentional weight loss occurred over a period of several months. Since I did not have an accurate time period I used 6 months since that seems to be when most of his symptoms appeared to classify the severity of his weight loss. His Percent Usual Body Weight calculation indicated a weight loss of 14% over a six month period which is severe. Mr. Seyer stated that he has been unable to consume his usual food preferences or his usual energy intake due to lack of appetite, a filling full all of the time, regurgitation of some foods,dysphasia (X 3 - 4 months), odynophagia (X 5 – 6 months) and heartburn (X approx. one year). The symptoms that Mr. Seyers described appear to be the factors that have contributed to his unintentional weight loss. 11. Estimate Mr. Seyer’s energy and protein requirements based on his current weight. a. energy requirement Weight: 198 lbs. = 90 kg Height: 6’3”= 75”=190.5 cm Male: 66.5+ 13.8W+ 5H-6.8A REE=66.5 + 13.8 (90 kg) + 5 (190.5 cm)-6.8 (58 years old) =66.5 + 1242+ 952.5- 394.4 1866.6 X 1.3= 2425.8 1866.6 X 1.5=2799 REE ~2430-2800 kcal b. protein requirement Protein in g/kg/d Non-stressed cancer: 1-1.5 Extreme wasting: 1.5-2.5 90 kg X 1.5 g/kg= 135 g Mr. Seyer’s admission chart indicated that he has some evidence of muscle wasting, therefore 1.5 g/kg was used to estimate his protein needs. 12. Estimate Mr. Seyer’s fluid requirements based on his current weight. • Average Adult 30-35 mL/kg 90 kg X 35 mL= 3,150 mL 13. What factors noted in Mr. Seyer’s history and physical may indicate problems with eating prior to admission? Prior to admission, the factors noted in Mr. Seyer’s history and physical that may indicate problems with eating include difficulty swallowing foods that have texture because of pain and heartburn; dysphagia x3-4 months and odynophagia x5-6 months, which may lead to decreased appetite, feeling full of the time, and regurgitation of some foods. The patient experienced a significant unexplained weight loss of over 30 lbs. in the last several months. Mr. Seyer uses two packs of tobacco per day and consumes one to two drinks 1-2x per week. In addition, the patient experiences constant heartburn and persistent cough at night. 17. Review the patient’s chemistries upon admission. Identify any that are abnormal and describe their clinical significance for this patient, the likely reason for each abnormality and its nutritional implications. Laboratory Chemistries ˅Total Protein Ref. Range 6-8 Mr. Seyer’s Value 5.7 Clinical Significance, Reason for Abnormality, and Nutritional Implications Protein supports cellular growth and development and is a reliable tool for nutrition assessment. When the body is experiencing metabolic stress it draws protein from the muscles to meet its needs but under normal circumstances it draws from fat and glycogen stores. Protein status is focused on two compartments: somatic (skeletal muscle) and visceral (non-muscular). Mr. Seyer has not been consuming adequate energy or protein due to lack of ˅ Albumin 3.5 - 5 3.1 ˅Prealbumin 16 - 35 15 ˅ RBC Count 4.5 – 6.2 4.2 appetite, a filling full all of the time, regurgitation of some foods,dysphasia (X 3 - 4 months), odynophagia (X 5 – 6 months) and heartburn (X approx. one year). His admission chart noted that there was evidence of muscle wasting. Decreased protein levels are associated with increased morbidity and mortality. Albumin is responsible for many functions in the body but most importantly as a transport protein and as a component of vascular fluid and electrolytes. Albumin changes often reflect illness and not necessarily nutritional status. It is a good screening tool but in an acute care setting it is not a reliable overall indicator of protein and nutritional status due to the effects of diseases, hydration, and other factors. Decreased albumin levels are associated with increased morbidity, mortality, and length of hospital stay. Albumin levels are a better indicator of stress and inflammation than overall protein status. Albumin has a long half life (17 – 20 days) therefore it is not a good indicator of short term changes in protein status or short term interventions to improve protein status. Albumin levels are affected by metabolic stress, acute and chronic inflammation, cirrhosis, and infection. Mr Seyer’s albumin levels are low and this may be a result of the metabolic stress caused by the cancer, immflammation, and overall poor nutrition and malaborption issues he is experiencing. He has been experiencing some of his symptoms for 6 months to a year. Prealbumin is responsible for transport of thyroxine and is associated with retinol-binding protein. Prealbumin has a short half life (2 days) and responds to short term changes in nutritional intake and interventions and is a useful tool to assess those at nutritional risk. Prealbumin levels drop as a result of illness, surgery, infection, metabolic stress, trauma, and malaborption. Mr. Seyer’s low Prealbumin levels can be associated with the cancer, metabolic stress, and inflammation that he is experiencing along with poor nutritional intake and malabsorption. RBC count is an important component of nutrition assessment and the diagnosis of all anemia types. RBCs contain hemoglobin, which carries oxygen. How much oxygen your body tissues get depends on how many RBCs you have and how well they work. Lower-than-normal numbers of RBCs may be due to: anemia, nutrition deficiencies of iron, copper, folic acid, vitamin B12, vitamin B6, malnutrition, over hydration, and many other factors. Severe or long-lasting anemia can damage the heart, brain, and other organs in your body. Very severe anemia may even cause death. Mr Seyer’s low blood count is possibly ˅Hemoglobin 14 - 17 13.5 ˅ Hematocrit 40 - 54 38 caused by his inability to consume adequate energy which has resulted in nutrition deficiencies of iron, copper, folic acid, vitamin B12, vitamin B6. Hemoglobin is a protein found in red blood cells that deliver oxygen to cells and pick up CO2 for expiration from the lungs. Measurement of hemoglobin in used to diagnose anemias, especially iron deficiency anemia. Low hemoglobin is found in individuals with some chronic diseases and protein energy malnutrition (PEM). It is not the most specific hematological test of nutritional status. Untreated low hemoglobin levels are a risk of increased morbidity and mortality. Nutritional factors that can lead to low hemoglobin counts are deficiencies of iron, folic acid, or vitamin B 12. This type of anemia is pernicious anemia. Mr. Seyer ‘s diagnosis of cancer and the extended period of time that he has not been able to consume adequate nutrients has resulted in his low hemoglobin status and lead to anemia. Hematocrit is the percentage of blood that is actually composed of red blood cells. It will decrease only in the final stages of iron deficiency. Low hematocrit may be due to: anemia, bleeding, destruction of red blood cells, leukemia, malnutriton, nutritional deficiencies of iron, folate, vitamin B12, over hydration and metabolic stress. Mr. Seyer’s has not been consuming adequate energy as indicated in his 24 hour recall due to lack of appetite, a filling fullness all of the time, regurgitation of some foods, dysphasia (X 3 - 4 months), odynophagia (X 5 – 6 months) and heartburn (X approx. one year) which has lead to decreased hematocrit levels and a higher risk of increased morbidity and mortality. ˄Mean Cell Hgb 26 - 32 32.4 ˅PT (sec) 12.4 – 14.4 12 Mean cell Hgb is an estimation of the amount of hemoglobin in each blood cell. MCV is useful in classifying anemias. The main reason that the MCH level would be too high is because of macrocytic anemia. Macrocytic anemia is a blood disorder in which not enough red blood cells are produced, but the ones that are present are large. Macrocytic anemia is often caused by having too little vitamin B12 or folic acid. Mr. Seyer has been unable to consume adequate nutrients and this has resulted in him not getting enough B12 and folate in his diet and has contributed to Mr. Seyer developing Macrocytic anemia. Prothrombin time (PT) is a blood test that measures the time it takes for the liquid plasma of your blood to clot.When iron is low in the body; zinc is substituted for iron within hemoglobin. Causes of low PT may be due to bleeding disorders, disseminated intravascular coagulation, liver disease or low levels of Vitamin K. Mr Seyer has not been able to consume adequate nutrients and is most likely experiencing malaborption due to his cancer diagnosis and metabolic stress therefore he is not getting enough vitamin K as indicated by his low PT level. His PT is not very low but may continue to drop if nutritional intervention is not initiated in a timely manner. 20. Select two high-priority nutrition problems after Mr. Seyer’s surgery and complete the PES statement for each. 1. Inadequate energy intake related to difficulty in eating due to dysphasia and painful swallowing as evidenced by 24 hour recall of kcal intake. 2. Unintentional weight loss of >30 lbs related to insufficient energy intake as evidenced by decreased appetite and reporting of insufficient energy dietary intake.