Pain Management for Hospice Patients
advertisement
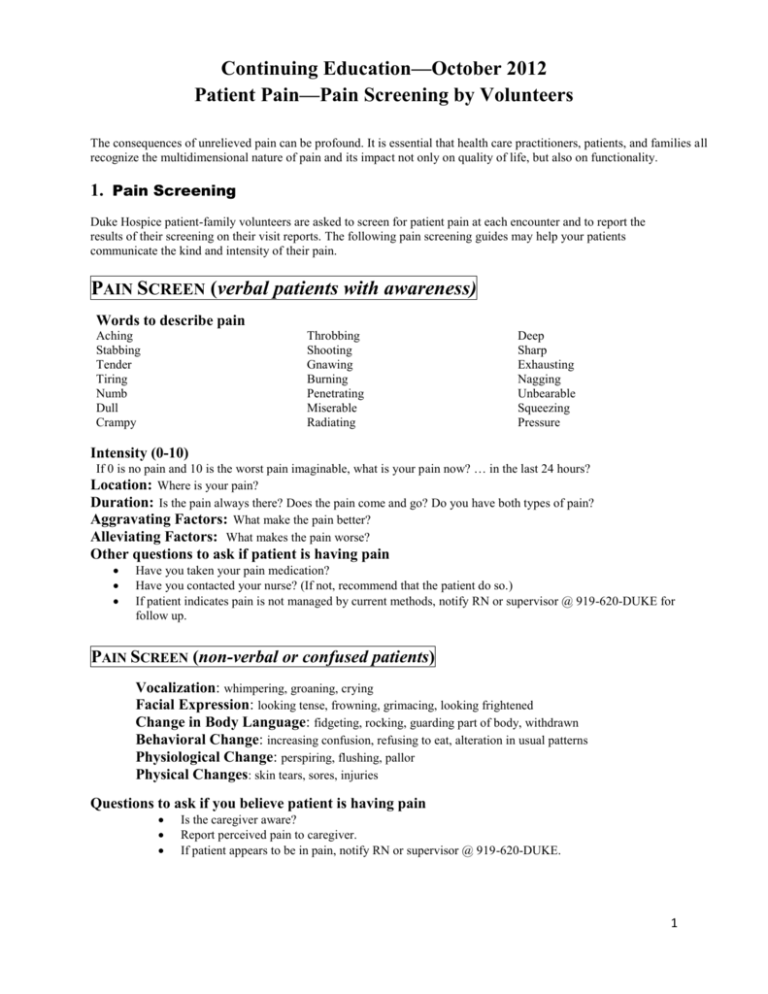
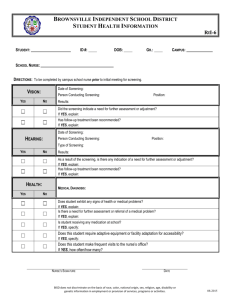
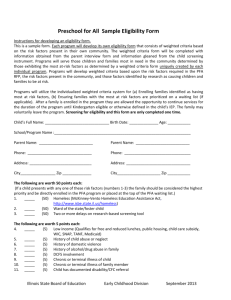
Continuing Education—October 2012 Patient Pain—Pain Screening by Volunteers The consequences of unrelieved pain can be profound. It is essential that health care practitioners, patients, and families all recognize the multidimensional nature of pain and its impact not only on quality of life, but also on functionality. 1. Pain Screening Duke Hospice patient-family volunteers are asked to screen for patient pain at each encounter and to report the results of their screening on their visit reports. The following pain screening guides may help your patients communicate the kind and intensity of their pain. PAIN SCREEN (verbal patients with awareness) Words to describe pain Aching Stabbing Tender Tiring Numb Dull Crampy Throbbing Shooting Gnawing Burning Penetrating Miserable Radiating Deep Sharp Exhausting Nagging Unbearable Squeezing Pressure Intensity (0-10) If 0 is no pain and 10 is the worst pain imaginable, what is your pain now? … in the last 24 hours? Location: Where is your pain? Duration: Is the pain always there? Does the pain come and go? Do you have both types of pain? Aggravating Factors: What make the pain better? Alleviating Factors: What makes the pain worse? Other questions to ask if patient is having pain Have you taken your pain medication? Have you contacted your nurse? (If not, recommend that the patient do so.) If patient indicates pain is not managed by current methods, notify RN or supervisor @ 919-620-DUKE for follow up. PAIN SCREEN (non-verbal or confused patients) Vocalization: whimpering, groaning, crying Facial Expression: looking tense, frowning, grimacing, looking frightened Change in Body Language: fidgeting, rocking, guarding part of body, withdrawn Behavioral Change: increasing confusion, refusing to eat, alteration in usual patterns Physiological Change: perspiring, flushing, pallor Physical Changes: skin tears, sores, injuries Questions to ask if you believe patient is having pain Is the caregiver aware? Report perceived pain to caregiver. If patient appears to be in pain, notify RN or supervisor @ 919-620-DUKE. 1 2. Consequences of Unrelieved Pain So why is all of this screening so important? Physical Fatigue/Decrease in Activity—results in diminished strength and endurance. Poor Appetite/Anorexia—results in diminished strength, delayed wound healing, and reduced tolerance of disease and/or treatment. Nausea—compounds problem of poor appetite and anorexia. Altered Sleep—unable to sleep or frequently awakens as a result of pain. May diminish overall sense of well being and ability to cope. Altered Immune Status—evidence supports that distress from pain can compromise the immune system. Psychological Diminished Leisure/Enjoyment—results in isolation, depression, boredom, and hopelessness. Anxiety—directly related to the presence of pain or indirectly related to the fear of potential pain such as an acute exacerbation with movement or procedures. Depression—pain often serves as a constant reminder of disease, uncontrollable disease progression, and death. It may evoke concerns of diminishing quality of life and loss of control. Loss of Control—pain may impede vocational functions, normal family activity, and self-care, resulting in a feeling of diminished usefulness. Difficulty Concentrating—inability to attend to the task at hand. Poor Compliance—patients may become so distressed by pain and treatment induced toxicities that they forgo treatment or seek “unproven” therapies that will induce little or no pain. Agitation/Irritability/Anger—pain anxiety, and loss of control can cause many individuals to feel very angry and frustrated. Fear—research has demonstrated that pain is an extremely frightening experience and patients and families facing cancer believe that pain will worsen. It is felt that this fear may best explain the overall influence of pain on psychological well being. Suicidal Ideation—pain, or fear of pain, may create a sense of hopelessness that can result in feeling as though life is not worth living if in pain. Social Diminished Social Relationships—pain interferes with the ability to interact with others. Many people become isolated and do not leave their homes when pain is not controlled. Sexuality/Affection—pain can interfere with an individual’s ability to provide or receive physical attention; loved ones may be reluctant for fear of hurting the individual with pain. Financial Effects—pain may prevent individuals from returning to work which may not only cause a financial burden, but can also change their family/social role. In addition, pain medications and therapies may be quite expensive, causing patients to have to choose between therapy and other necessities. Spiritual Increased Suffering—suffering denotes an extended sense of threat to self-image and life, a perceived lack of options for coping, a sense of personal loss, and a lack of a basis for hope. Religiosity—pain can cause an individual to question their beliefs or feel as though they have somehow displeased their God, for which they are now being punished. Altered Meaning—pain may create a sense of hopelessness that can result in feeling as though life is not worth living if in pain. Pain may also serve to positively impact one’s life and sense of purpose. Purpose—culturally, pain may be expected and considered positive or purposeful, helping to heighten an individual’s place in an afterlife. 2