Eating Disorders and the Psychology of Adolescence - PBL-J-2015
advertisement
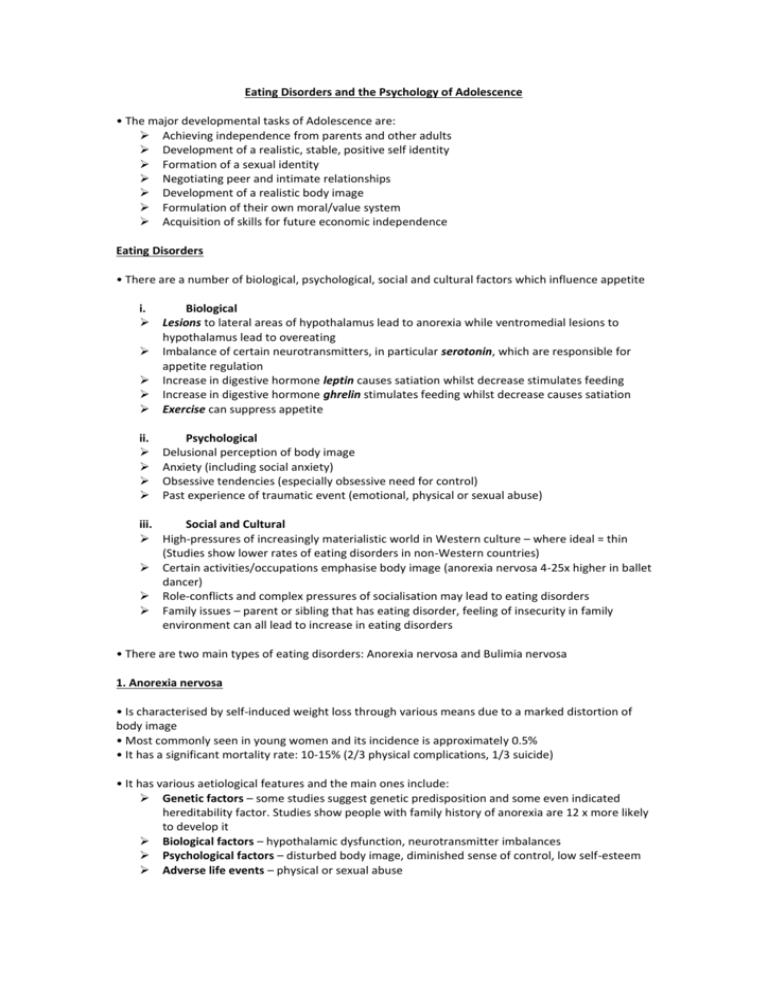
Eating Disorders and the Psychology of Adolescence • The major developmental tasks of Adolescence are: Achieving independence from parents and other adults Development of a realistic, stable, positive self identity Formation of a sexual identity Negotiating peer and intimate relationships Development of a realistic body image Formulation of their own moral/value system Acquisition of skills for future economic independence Eating Disorders • There are a number of biological, psychological, social and cultural factors which influence appetite i. Biological Lesions to lateral areas of hypothalamus lead to anorexia while ventromedial lesions to hypothalamus lead to overeating Imbalance of certain neurotransmitters, in particular serotonin, which are responsible for appetite regulation Increase in digestive hormone leptin causes satiation whilst decrease stimulates feeding Increase in digestive hormone ghrelin stimulates feeding whilst decrease causes satiation Exercise can suppress appetite ii. Psychological Delusional perception of body image Anxiety (including social anxiety) Obsessive tendencies (especially obsessive need for control) Past experience of traumatic event (emotional, physical or sexual abuse) iii. Social and Cultural High-pressures of increasingly materialistic world in Western culture – where ideal = thin (Studies show lower rates of eating disorders in non-Western countries) Certain activities/occupations emphasise body image (anorexia nervosa 4-25x higher in ballet dancer) Role-conflicts and complex pressures of socialisation may lead to eating disorders Family issues – parent or sibling that has eating disorder, feeling of insecurity in family environment can all lead to increase in eating disorders • There are two main types of eating disorders: Anorexia nervosa and Bulimia nervosa 1. Anorexia nervosa • Is characterised by self-induced weight loss through various means due to a marked distortion of body image • Most commonly seen in young women and its incidence is approximately 0.5% • It has a significant mortality rate: 10-15% (2/3 physical complications, 1/3 suicide) • It has various aetiological features and the main ones include: Genetic factors – some studies suggest genetic predisposition and some even indicated hereditability factor. Studies show people with family history of anorexia are 12 x more likely to develop it Biological factors – hypothalamic dysfunction, neurotransmitter imbalances Psychological factors – disturbed body image, diminished sense of control, low self-esteem Adverse life events – physical or sexual abuse Clinical features Physical – significant weight loss, thinning or loss of hair, amenorrhoea (young women), insomnia, constipation Behavioural – unusual eating habits, excessive exercise, social withdrawal Psychological – depression, perfectionism, unwarranted belief of being fat or intense fear of becoming fat Diagnostic Criteria – DSM IV for Anorexia nervosa A. Refusal to maintain body weight at or above a minimally normal weight for age and height (body weight less than 85% of what is expected) B. Intense fear of gaining weight or becoming fat, even though underweight C. Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight. D. In postmenarcheal females, amenorrhea, i.e. the absence of at least three or more consecutive menstrual cycles. (A woman is considered to have amenorrhea if her periods occur only following hormone, e.g. oestrogen, administration). Specific subtypes Restricting Type: during current episode of Anorexia nervosa, person has not regularly engaged in binge-eating or purging behaviour Binge-eating/Purging type: during current episode of Anorexia nervosa, person has regularly engaged in binge-eating or purging behaviour Treatment • Coercive/threatening approach is counterproductive. It requires supportive combined approach of: Pharmacological – selective serotonin reuptake inhibitors such as Fluoxetine (especially if there are clear obsessional ideas regarding food) Psychological – involvement of family in treatment, individual behavioural therapy, use of psychologists and psychiatrists Education – nutritional education (dietary advice, use of food diary) • Hospital admission should only be considered if there are serious medical problems 2. Bulimia nervosa • Is characterised by recurrent binge eating and purging, accompanied with delusional perception of body shape and weight • Most commonly seen in young women and its incidence is approximately 2% • Often history of Anorexia nervosa (30-50%) of people who have Bulimia nervosa • It has similar aetiology to Anorexia Nervosa • It has similar clinical features except in physical characteristics patient can present with normal weight. Also get fluctuation of weight due to bingeing and purging, and swollen salivary glands • It has similar treatment method as Anorexia nervosa Final thought • There are certain behavioural characteristics or personality traits which contribute to the development of eating disorders. They include: Obsessive-compulsive type behaviours Depression Anxiety Perfectionists Low self-esteem/poor sense of identity