File
advertisement
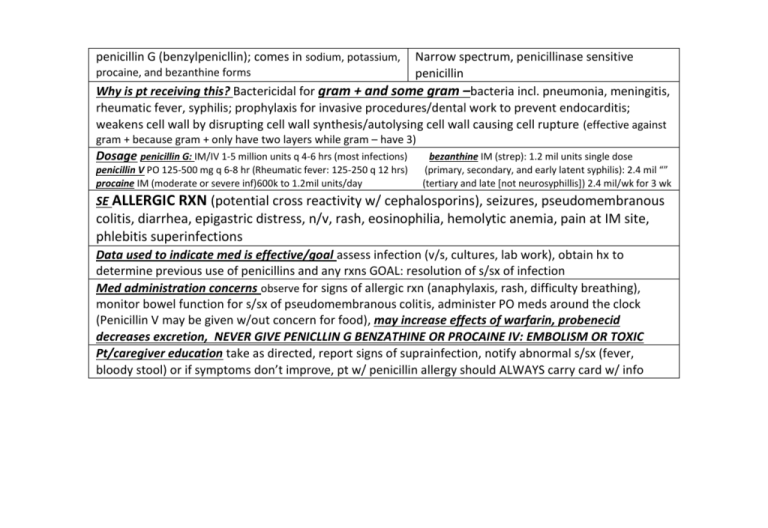
penicillin G (benzylpenicllin); comes in sodium, potassium, Narrow spectrum, penicillinase sensitive penicillin Why is pt receiving this? Bactericidal for gram + and some gram –bacteria incl. pneumonia, meningitis, rheumatic fever, syphilis; prophylaxis for invasive procedures/dental work to prevent endocarditis; weakens cell wall by disrupting cell wall synthesis/autolysing cell wall causing cell rupture (effective against procaine, and bezanthine forms gram + because gram + only have two layers while gram – have 3) Dosage penicillin G: IM/IV 1-5 million units q 4-6 hrs (most infections) penicillin V PO 125-500 mg q 6-8 hr (Rheumatic fever: 125-250 q 12 hrs) procaine IM (moderate or severe inf)600k to 1.2mil units/day bezanthine IM (strep): 1.2 mil units single dose (primary, secondary, and early latent syphilis): 2.4 mil “” (tertiary and late [not neurosyphillis]) 2.4 mil/wk for 3 wk SE ALLERGIC RXN (potential cross reactivity w/ cephalosporins), seizures, pseudomembranous colitis, diarrhea, epigastric distress, n/v, rash, eosinophilia, hemolytic anemia, pain at IM site, phlebitis superinfections Data used to indicate med is effective/goal assess infection (v/s, cultures, lab work), obtain hx to determine previous use of penicillins and any rxns GOAL: resolution of s/sx of infection Med administration concerns observe for signs of allergic rxn (anaphylaxis, rash, difficulty breathing), monitor bowel function for s/sx of pseudomembranous colitis, administer PO meds around the clock (Penicillin V may be given w/out concern for food), may increase effects of warfarin, probenecid decreases excretion, NEVER GIVE PENICLLIN G BENZATHINE OR PROCAINE IV: EMBOLISM OR TOXIC Pt/caregiver education take as directed, report signs of suprainfection, notify abnormal s/sx (fever, bloody stool) or if symptoms don’t improve, pt w/ penicillin allergy should ALWAYS carry card w/ info dicloxacillin (Nallpen) Narrow spectrum penicillinase resistant penicillin Why is pt receiving this? treatment of resp., skin/skin structure, and sinus infection due to penicillinase-producing staphylococci (staph infections), also indicated in osteomyelitis. Binds to bacterial cell wall, leading to death. Dosage PO 125-250 mg q 6hr (up to 2g/day) SE Seizures (high doses), pseudomembranous colitis, diarrhea, n/v, drug induced hepatitis, rashes, allergic reactions incl Anaphylaxis and serum sickness superinfections Data used to assess effectiveness/goal Assess infection, obtain hx of penicillin use/rxn, liver function tests as indicated GOAL: resolution of s/sx of infection Medication administration concernsobserve for s/sx of anaphylaxis, s/sx of pseudomembranous colitis and jaundice, administer medication around the clock, take with full glass of water (Penicillins are weak/easily destroyed in acid and fruit juices may decrease absorption), may increase effects of warfarin, probenecid decreases excretion Pt/caregiver education report s/sx of suprainfection (fuzzy tongue, vaginal itching or discharge, loose or foul smelling stools), abnormal s/sx (fever, diarrhea, blood in stool), notify if symptoms do not improve amoxicillin Broad spectrum penicillins (aminopenicillins) Why is pt receiving this? treatment of skin and skin structure infections, otitis media, sinusitis, resp infections, gu infection, endocarditis prophylaxis, post exposure of anthrax inhalation and mgmt. of PUD caused by H pylori Dosage most infections: 250-500 mg PO q 8 hr or 500-875 mg q 12 hr (not to exceed 2-3 g/day) SE Seizures (high doses), pseudomembranous colitis, n/v, diarrhea, increased lvier enzymes, rash, ALLERGIC RXNS, superinfections Data used to assess effectiveness/goal Assess for infection before and throughout therapy, obtain hx of previous use/rxn to penicillin GOAL: resolution of s/sx of infection Med administration concerns Administer PO med around the clock, can be given w/out regard to meals (can be given w/ meals to decrease GI side effects), monitor for s/sx of anaphylaxis, pseudomembranous colitis ; decreases effectiveness of oral contraceptives, increases effects of warfarin, probenecid decreases excretion Pt/caregiver education report s/sx of suprainfection (fuzzy tongue, vaginal itching or discharge, loose or foul smelling stools), abnormal s/sx (fever, diarrhea, blood in stool), notify if symptoms do not improve, advise female pts using oral contraceptives to consult other b/c methods piperacillin (Zosyn when combined w/ Extended spectrum penicillins (spectrum is extended tazobactam) compared to other penicillins, incl gram negitve aerobes such as pseudomonas aeruginosa, active against anaerobic bact.) Why is pt receiving this? appendicitis, peritonitis, skin/skin structure infections, gyenecologic infections, community acquired and nosocomial pneumonia; binds to bacterial cell wall membrane causing death Dosage given IV, depending on infection, renal impairment adjustments as appropriate SE Seizures (higher doses), confusion, dizziness, HA, insomnia, pseudomembranous colitis, diarrhea, constipation, drug induced hepatitis, n/v, interstitial nephritis, SJS, TENS, rash, bleeding, leukopenia, pain/phlebitis @ IV site, ALLERGIC RXNS Assessment data to determine effective/goal assess infection, obtain hx of PCN use and rxn GOAL: resolution of s/sx of infection Med administration concerns probenecid decreases excretion, may alter lithium, potassium losing diuretics/corticosteroids/amphotericin B may increase risk of hypokalemia, may increase risk of heptatoxicity w/ other hepatotoxic agents, may decreases levels of aminoglycosides; assess for s/sx of anaphylaxis, SJS/TENS, pseudoemembranous colitis Pt/caregiver education: report s/sx of suprainfection (fuzzy tongue, vaginal itching or discharge, loose or foul smelling stools), abnormal s/sx (fever, diarrhea, blood in stool), notify if symptoms do not improve, advise female pts using oral contraceptives to consult other b/c methods amoxicillin + clavulanate (Augmentin) Just like Aminopenicillins/betalactamase inhibitors Unasym (ampicillin + sulbactam) Why is pt receiving this? Treatment of variety of infections; penicillin binds to cell wall to inhibit synthesis (bact. cell lysis) and betalactamase inhibitor resists bacterial defense mechanisms beta lactamase destroys penicillin Dosage most infections PO 250 mg q 8 hrs or 500 mg q 12 hrs; serious infections and resp. infections PO 875 mg q 12 hr or 500 mg q 8 hr SE seizures (high doses), pseudomembranous colitis, diarrhea, hepatic dysfunction, n/v, vaginal candidiasis, ALLERGIC rxns Data used to assess effectiveness/goal Assess for infection before and throughout therapy, obtain hx of previous use/rxn to penicillin GOAL: resolution of s/sx of infection Med administration concerns Administer PO med around the clock, can be given w/out regard to meals (can be given w/ meals to decrease GI side effects), AVOID HIGH FAT MEALS (decreases absorption of clavulanate) monitor for s/sx of anaphylaxis, pseudomembranous colitis ; decreases effectiveness of oral contraceptives, increases effects of warfarin, probenecid decreases excretion Pt/caregiver education report s/sx of suprainfection (fuzzy tongue, vaginal itching or discharge, loose or foul smelling stools), abnormal s/sx (fever, diarrhea, blood in stool), notify if symptoms do not improve, advise female pts using oral contraceptives to consult other b/c methods cefazolin (Ancef) First generation cephalosporin (narrow spectrum) Why is pt receiving this? perioperative prophylaxis, treatment of skin/skin structure, pneumonia, UTIs, bone and join infections and septicemia Produce lysis like PCN’s, binds to penicillin binding proteins which disrupts cell wall synthesis (causes cell lysis); used with many gram + and some gram Dosage IM, IV moderate to severe infections: 500 mg-2g q 6-8 hrs; mild infections w/ gram positive cocci: 250-500 mg q 8 hr perioperative prophylaxis: 1 g given 30-60 min prior to surgery (additional 500 mg-1g given for surgeries > 2 hr) SE seizures (high doses), pseudomembranous colitis, diarrhea, n/v, Stevens Johnson syndrome, rashes, agranulocytosis, eosinophilla, hemolytic anemia, neutropenia, thrombocytopenia, pain at IM site, phlebitis at IV site ALLERGIC RXN incl anaphylaxis and serum sickness (if pt has PCN allergy, 5-10% chance of cross rxn with cephalosporins) superinfection Data used to assess effectiveness/goal Assess for infection before and throughout therapy, obtain hx of previous use/rxn to penicillin GOAL: resolution of s/sx of infection, decreased incidence of infection when used prophylactically Med administration concerns: probenecid decreases excretion, concurrent use of loop diuretics or aminoglycosides can result in nephrotoxicity, assess for s/sx of anaphylaxis, pseudomembranous colitis, SJS Pt/caregiver education report unusal s/sx including changes in breathing,bowel habits (bloody, diarrheal stools), fever, and rash, report signs of superinfection cefuroxime (Ceftin) Second generation cephalosporin (increased activity to more gram negative than first generation (e.g. more broad spectrum than first generation) Why is pt receiving this? treatment of resp., skin/skin structure, bone and joint, UTI, infections caused by susceptible organisms, as well as meningitis, gynecologic infections and lyme disease Dosage oral tablets and oral suspension ARE NOT substitutable (not bioequivalent) PO varies based on infection, gonorrhea- 1 g single dose IM, IV: varies based on infection SE seizures (high doses), pseudomembranous colitis, diarrhea, cramps, n/v, rashes, agranulocytosis, bleeding, eosinophilia, hemolytic anemia, neutropenia, thrombocytopenia, pain at IM site, phlebitis at IV site, Allergic rxns Data used to assess effectiveness/goal Assess for infection before and throughout therapy, obtain hx of previous use/rxn to penicillin GOAL: resolution of s/sx of infection Med administration concerns Tablets should be swallowed whole and not broken to avoid lasting bitter aftertaste, may be taken w/out regard to food, probenecid decreases excretion, concurrent use of loop diuretics or aminoglycosides can result in nephrotoxicity, assess for s/sx of anaphylaxis, pseudomembranous colitis Pt education report unusal s/sx including changes in breathing,bowel habits (bloody, diarrheal stools), fever, and rash, report signs of superinfection ceftriaxone (Rocephin) Third generation cephalosporin (less effective than previous generations in treating staphylococci, whereas activity against gram negative pathogens is greater) Why is pt receiving this? treatment of skin/skin structure, urinary and gynecologic, resp., bone/joint infections, meningitis, intra-abdominal infections and septicemia, otitis media, perioperative prophylaxis, and lyme disease Dosage IM, IV Most infections: 1-2 g q 12-24 hr, Gonorrhea 250 mg IM (single dose) meningitis: 2 g q 12 hr. perioperative prophylaxis: 1 g 30 min-2hr before surgery SE seizures (high doses), pseudomembranous colitis, diarrhea, cramps, n/v, rashes, agranulocytosis, bleeding, SJS, eosinophilia, hemolytic anemia, neutropenia, thrombocytopenia, pain at IM site, phlebitis at IV site, Allergic rxns Data used to assess effectiveness/goal Assess for infection before and throughout therapy, obtain hx of previous use/rxn to penicillin GOAL: resolution of s/sx of infection, decreased incidence of infection when used preoperatively Med administration concerns: probenecid decreases excretion, concurrent use of loop diuretics or aminoglycosides can result in nephrotoxicity, should not be given with calcium containing solutions, assess for s/sx of anaphylaxis, pseudomembranous colitis, SJS Pt/caregiver education report unusal s/sx including changes in breathing,bowel habits (bloody, diarrheal stools), fever, and rash, report signs of superinfection cefepime (Maxipime) Fourth generation cephalosporin (less effective than previous generations in treating staphylococci, whereas activity against gram negative pathogens is greater) Why is pt receiving this? treatment of following infections: uncomplicated skin and skin skin structure infections, bone and joint infections, uncomplicated/complicated UTI’s, respiratory tract infections, complicated intra-abdominal infections, septicemia DosageIM: mild/moderate (un)complicated UTI due to E.coli: .5-1 g every 12 hr IV: varies based on infection; see manufacturer’s recommendations for impaired renal adjustment SE Seizures (increased risk in renal impairment), encephalopathy, HA, pseudomembranous coltis, diarrhea, n/v, rahes, bleeding, eosinophila, hemolytic anemia, neutropenia, thrombocytopenia, pain @ IM site, phlebitis @ IV, allergic rxns , superinfection Data used to assess effectiveness/goal Assess for infection before and throughout therapy, obtain hx of previous use/rxn to penicillin GOAL: resolution of s/sx of infection Med administration concerns: probenecid decreases excretion, concurrent use of loop diuretics or aminoglycosides can result in nephrotoxicity, should not be given with calcium containing solutions, assess for s/sx of anaphylaxis, pseudomembranous colitis Pt/caregiver education report unusal s/sx including changes in breathing,bowel habits (bloody, diarrheal stools), fever, and rash, report signs of superinfection imipenem (Primaxim) (imipenem/cilastatin Carbapenems broad spectrum betalactam [cilastatin prevents renal inactivation]) Why is pt receiving this? Bacterostatic but can be bactericidal; treatment of pseudomans aeruginosa, lower RTIs, UTI’s, abd infections, skin/skin structure infection, gyenecologic infections, bone and joint, bacteremia, endocarditis, polymicrobic infections Dosage IV mild: 250-500 mg q 6 hrs/moderate: 500 mg q 6-8 or 1 g q 8 hrs/ serious: 500 mg q 6 hrs to 1 g q 6-8 hrs; [250 mg/mL w/ 250-mg vial; 5 mg/mL w/ 500 mg vial], Rate: doses under 500 mg inf over 20-30 min; > or equal to 750 over 40-60 min IM: 500-750 mg q 12 hr Renal impairment adjustments SE: Hypersensitivity, GI effects, suprainfections, seizures, dizziness, somulence, hypotension, pseudomembranous colitis, diarrhea, n/v, rash, phlebitis Data used to assess effectiveness: Assess for infection before and throughout therapy, obtain hx of previous use/rxn to penicillin GOAL: resolution of s/sx of infection Med administration concerns observe for anaphylaxis, suprainfections, probenecid decreases renal excretion, may be inactivated if used w/ aminoglycosides Pt/caregiver education pts Notify for signs of rxn, signs of suprainfection, and bloody/diarrheal stool, fever vancomycin (Lyphocin) anti-infectives Why is pt receiving this? Bactericidial treatment of potentially life threatening infections when less toxic anti-infectives are contraindicated. Particularly useful in staphylococcal infections incl endocarditis (can be used prophylactically IV), MRSA, Cdiff (PO); binds to cell wall Dosage Renal impairment adjustments Serious systemic infections: IV 500 mg q 6 hr or 1 g q 12 hr (up to 4 g/day) Endocarditis prophylaxis: IV: 1 g signle dose 1 hr pre-procedure Diarrhea due to C. diff PO: 125 mg q 6 hr for 10 days Staph. Enterocolitis: PO 500-2000 mg/day in 3-4 divided doses for 7-10 days SE N/V, altered taste, otoxicity (reversible, but not always), hypotension, nephrotoxicity, eosinophilia, leukopenia, phlebitis, HYPERSENSITIVITY rxns RED MAN/RED NECK SYNDROME (occurs if given too fast, not a genuine allergic rxn, pt can still receive if diluted over 60 min) Data used to assess effectiveness signs of infection, severity of diarrhea, bowel status Med administration concerns additive ototoxic and nephrotoxic effects w/ other agents, monitor IV site closely for signs of vein irritation, monitor Is and OS and daily weight (cloudy/pink urine may be sign of nephrotoxicity), assess for signs of superinfection, anaphylaxis; orally administered only for C diff and Staph, Pt/caregiver education take as directed, do not double dose, instruct pt to reporst signs of hypersensitivity, tinnitus, vertigo, hearing loss, notify if no improvement seen, tetracycline (Sumycin) Tetracycines (bacteriostatic inhibitors of prn synthesis) Why is pt receiving this? various infections caused by unusal organisms, incl. rickettsial disease, chlamydia trachomatis, brucellosis, cholera, mycoplasma pneumonia, lyme disease, anthrax; inhibits bacterial synthesis at level of 30s bacterial ribosome Tetracycline also indicated in acne Dosage PO 250-500 mg q 6 hr or 500 mg-1 g q 12 hr SE: benign intracranial hypertension, Hepatoxicity, pseudomembranous colitis, diarrhea, n/v, esophagitis, pancreatitis, SJS, TENS, photosensitivity, thrombophlebitis, hepatotoxicity, renal toxicity, vestibular toxicity Data used to assess effectiveness assess s/sx of infection, Medication administration concern risk of permanent staining of teeth in infant if used during last half of pregnancy, contraindicated in children under 8; food slows fast/intermediate acting forms (minocycline) administer w/ full glass of water 1 hs to prevent esophageal upset; chelating agent will bind to calcium supplements, milk products, iron supplements, magnesium laxatives, and antacids GIVE 1 HR BEFORE MEALS OR 2 HR AFTER MEALmay increase effect of warfarin and decrease effect of estrogen contraceptives, monitor bowel function, signs of rash Pt/caregiver education take exactly as directed and finish regiment even if feeling better, advise pt to avoid taking milk or dairy w/ oral tetracylines as well as antacids, zinc, calcium, mg, or al containing medications, sodium bicarb and iron supplements; notify immediately s/sx of SJS/TENS, pseudomembranous colitis, hepatotoxicity occur, advise females to use non hormonal b/c methods, use sunscreen and protective clothing to prevent photosensitivy rxns, report suprainfection, discard outdated or decomposed tetracylines (may be toxic) gentamicin (“-micin”, “-mycin”) Aminoglycoside (bactericidal inhibitor of prn synthesis) (Gramycin/G-mycin) Why is pt receiving this? Treatment of infection cause by AEROBIC GRAM NEGATIVE BACILLI when penicillin contraindicated; can be used in tandem w/ other antibiotics for mgmt. of serious enterococcal infections, prevention of endocarditis (IV), treatment of localized infections (topical); inhibits bact synthesis by acting at 30 s subunit Dosage IM/IV 1-2 mg/kg q 8 hr (up to 6 mg/kg/day in 3 divided doses) SE IRREVERSIBLE OTOTOXICITY,NEPHROTOXICITY, hypersensitivity, neuromuscular blockade, hypomagnemesia, Med administration concerns VERY IMPORTANT MED TO DETERMINE SERUM LEVELS VIA PEAK/TROUGH (draw peak 30 min after IV administration and trough 1 hr before next dose), Inactivated by cephalosporins and penecillins, increase risk of ototoxicity w/ loop diuretics, Assess 8th cranial nerve function constantly throughout therapy, s/sx of infection and superinfection , monitor Is and Os for assessment of renal function Pt caregiver education Importance of encouraging fluids erythromycin (-ycin) macrolides Why is pt receiving this? Infections normally treated with penicillin where pt has penicillin infection (for example: legionella pneumophilia, bordatella pertussis, corynebacterium diphtheria, chlamidia) , broad spectrum(gram + and some gram -) bacteriostatic antibiotic that inhibits prn synthesis at 50s bacterial ribosome Dosage (depends on form)most infections PO: 250 mg q 6 hr or 333 mg q 8 hr or 500 mg q 12 hr IV: 250-500 mg (up to 1 g) q 6 hr SE seizures (rare), otoxicity, TORSADES DE POINTES, VENTRICULAR ARRYTHMIA (QT Interval elongation) pseudomembranous colitis, n/v, abd pain, cramping, CHOLESTATIC HEPATITIS interstitial nephritis, phlebitis @ IV site, ALLERGIC RXNS, superinfection Med Administration Concerns use w/ diltiazem, verapamil, and protease inhibitors can increase risk of cardiac arrhythmias; may increase levels of ergotamine and dihydroergotamine and risk for acute ergot toxicity, concurrent use with amioderone increases risk of torsades, INTERACTS W/ DIGOXIN, WARFARIN, STATINS, CCBS, monitor bowel status/function, better absorption if given 1 hr before meals and 2 hrs after Pt/caregiver education BAD METALLIC TASTE, notify s/sx of fever/diarrhea, adverse signs, superinfection clindamycin (Cleocin) Anti-infective Why is pt receiving this? indicated for anaerobic infections located outside of CNS Dosage PO: most infections 150-450 mg q 6 hrs; IM/IV: 300-600 mg q 6-8 hrs or 900 mg q 8 hrs IV: dilute 300/600 mg in 50 mL D5W, NS, D5NS, D51/2NS, LR; 900/1200 in 100 mL [] not to exceed 1800 mg/mL and not to exceed rate of 30 mg/min (can cause cardiopulmonary arrest) SE PSEUDOMEMBRANOUS COLITIS , arrhythmias, hypotension, dizziness, confusion, diarrhea, n/v, phlebitis @ IV site Med administration concern Monitor s/sx of infection and for pseudomembranous colitis, assess for hypersensitivity; administer PO w/ full glass of water, do not administer >600 mg in single IM injection, Pt/caregiver teaching pts report abnormal s/sx, signs of suprainfection, bitter taste occurs with IV, sulfamethoxone-trimethoprim (Bactrim) SULFA drug (BROAD SPECTRUM) Why is pt receiving this? Bronchitis, shigella, otitis media, UTI’s pneumocystic pneumonia (PCP), prevention of PCP in HIV+ patients; burn (unlabeled use) Inhibits folic acid production by bacteria Dosage PO/IV depends on infection SE HYPERSENSITIVITY , Red man syndrome, SJS, fatigue, hypotension, kernicterus in neonates, hyperkalemia, hyponatremia, crystaluria, photosensitivity, hypoglycemia, agranulocytosis, aplastic anemia, phlebitis Med Administration Concerns can increase effects of digoxin and warfarin, increase risk of thrombocytopenia from thiazide diruetics (esp in geriatrics), risk of hyperkalemia w/ concurrent use of ACE inhibitors, monitor for phlebitis, hypersensitivity rxns, monitor Is and Os and bowel function Pt/caregiver education Encourage fluids to prevent crystaluria, monitor for allergy, notify for adverse s/sx nitrofurantonin (Fuadantin) Anti-infective Why is pt receiving this? prevention/treatment of UTI’s; BACTERIOSTATIC: [low]; BACTERICIDAL [high] Dosage Active infection: 50-100 mg q 6-8 hr or 100 mg q 12 hr (extended release) Chronic suppression: 50-100 mg single evening dose SE: dizziness, drowsiness, HA, nystagmus, pneumonitis, pulmonary fibrosis, pseudomembranous colitis, anorexia, n/v, hepatotoxicity, photosensitivity, peripheral neuropathy, HYPERSENSITIVITY Med admin concerns antacid can decrease absorption, additive hepatotoxic effects; administer with food or mild to minimize GI irritation, dealy/increase absorption, increase peak concentration; DO NOT CRUSH; Pt/caregiver education wear sunscreen/protective clothing after d/c (photosensitivity), report adverse s/sx, rust colored discoloration of urine normal, may cause dizziness/drowsiness phenazopyridine (Pyridium) Urinary tract analgesics (nonopioid) Why is pt receiving this? Provides relief from UT symptoms: pain, itching, burning, urgency, frequency DosagePO 200 mg 3 times daily for 2 days SE: BRIGHT ORANGE URINE , may make skin looked jaundice, HA, vertigo, hepatotoxicity, nausea, rash Data used to determine med’s effectiveness Assess pain, GOAL: decrease in pain and burning on urination Med administration concerns Med should be discontinued after pain relieved, administer with or following meals to decrease GI irritation, DO NOT CRUSH, Pt/caregiver education Educate that although this may be discontinued after relief, very important to continue antibiotic regimen, orange discoloration of urine normal, may cause staining of soft contact lenses ciprofloxacin (Cipro) Fluoroquinolones Why is pt receiving this? urinary tract infections incl cystitis and prostatis, gonorrhea (not first line due to increasing resistance) gynecologic infections, respiratory tract infections including sinustitis, acute exacer. chronic bronchitis, skin and skin structure infections, bone/joint infections, infectious diarrhea, postexposure treatment of inhalational anthrax; inhibits bacterial DNA gyrase enzyme BROAD SPECTRUM Dosage PO (most infections): 500-750 mg q 12 hr; IV (most infections): 400 mg q 12 hr; [1-2 mg/mL], administer over 60 min into large vein Renal impairment adjustment SE Elevated intracranial pressure, seizures, HA, CNS symtpoms, Hepatotoxicity, Pseudomembranous colitis, diarrhea, nausea, Candida suprainfection of pharynx and vagina, tendon rupture (especially in children <1 and elderly) HYPERSENSITIVITY, SJS Med Administration Concerns concurrent use of amioderone, erythromycin, quinide, and some antipsychotics increases risk of torsades, CHELATION agent, may increase effects of warfarin, cimetidine may impair elimination, probenecid decreases renal excretion, use w/ corticosteroids increases risk of tendon rupture, suspension should not be administered in feeding tube Pt/caregiver education Notify for signs of hypersensitivity, pseudomembranous colitis, may cause dizziness/ drowsiness, partners of pt being treated for gonorrhea must be tested metronidazole (Flagyl) Anti-infectives/antiprotozoals Why is pt receiving this: PO/IV: Tretment of protozal infections (may be used w/ a cephalosporin), obiglate anaerobes, and H. Pylori , PO: amebacide, IV: perioperative prophylactic ; prohibits prn and DNA synthesis Dosage: Dosage varies based on infection IV: [5 mg/mL] over 30-60 min SE: Neurotoxicity, ALLERGY, superinfections, Disulfiram (antabuse like) rxn w/ alcohol, Seizures, dizziness, HA, asceptic meningitis/encephalopathy (IV), optic neuropothy, abd pain, anorexia, nausea, SJS, rash, urticarial; Phlebitis @ IV site Med Administration Concerns Cimetidine may decrease absorption, phenobarbitol and rifampin may increase metab (decrease effectiveness), increases effects of phenytoin, lithium, and warfarin; Disulfiram rxn can be so bad as to affect a person using mouthwash. Assess for rash. Pt caregiver education: Take as directed, finish regimen; when used for trichiminosis, sexual partners may be asymptomatic sources of reinfection (get tested); avoid use of alcohol until at least 3 days after last part of treatment; unpleasant medical taste; medication may turn urine dark Amphotericin B (Fungizone) (referred to as “amphoterrible”) Antifungal HIGH ALERT Why is pt receiving this? Treatment of progressive, potentially fatal fungal infections .Binds to fungal cell membrane, allowing leakage of cellular contents. Selective for ergosterol (fungal) more than cholesterol. May be fungistatic or fungicidal. Dosage IV/IT. IV: give test dose of 1 mg. If test dose tolerated, initate therapy w/ .25 mg/kg/day. SE: HIGHLY TOXIC Tissue sloughs away w/ infiltration; Infusion RXNS: fever, chills, rigors, nausea, HA (can be reduced slightly w/ pretreatment w/ diphenhydramine plus acetaminophen. ASA can help but can cause kidney damage). Nephrotoxicity, Hypokalemia, chest pain, hypotension, diarrhea, hyperbillirubinemia, n/v, HYPERSENSITIVTY RXNS Med Administration Concerns Unknown metabolism/elimination, wear gloves when handling, need to invert/shake solution every ½ hr to keep in suspension, concurrent use w/ corticosteroids increases effects of hypokalemia (remember Cushing’s disease) MONITOR PT FOR FIRST ½ HR after infusion started, assess IV site frequently, monitor VS every 15 min of infection and 30 min for 2-4 hrs post infusion , Pt/caregiver education: inform pt of potential side effects and discomfort at IV site, Notify HCP if ANY adverse effects experienced ketoconazole (Nizoral) (-“azole”) Systemic anti-infectives Why is pt receiving this? Treatment of less severe fungal infections, candidiasis, chromomycosis, coccoidomycosis, histoplasmosis, blastyomycosis, etc. Inhibits synthesis of ergosterol Dosage PO: 200-400 mg/day single dose; can also be used topically SE (generally less in topical treatment) Hepatotoxicity, dizziness/drowsiness, TORSADE’s, n/v, sex hormone changes (decrease in sperm count, decreased male libido, menstral irregularities, gynecomastia), adrenal insufficiency, ANAPHYLAXIS Med Administration Concerns significant CYP450 player, can increase levels of quinidine, may increase levels and risks of statins, may increase levels and risk toxicity with ergotamine and dihydroergotamine, can increase levels of digoxin, oral hypoglycemic agents, warfarin, carbamezpine; may alter effectiveness of hormonal contraceptives, H2 blockers and PPI decrease absorption, risk of hepatoxicty w/ alcohol or other hepatotoxic agents, administer WITH meals to decrease GI upset Pt caregiver education: instruct pt to take med as directed at same time each day, avoid concurrent use of alcohol, may cause dizziness/drowsiness (avoid driving, fall risk precautions), photophobic precautions, use nonhormonal form of contraception griseofulvin Systemic anti-fungal Why is pt recieivng this? Treatment of superifical (tinea) infections that do not respond to topical antifungals. Tinea capitis (head), pedis (foot) onychomycosis (nail fungus); Inhibits fungal mitosis Dosage PO: microsize Tinea pedis, onychomycosis 500 mg q 12 hr. Tinea capitis, corporis, or curis: 250 mg q 12 hr or 500 mg once daily Ultramicrosize Tinea pedis, onychomycosis 375 mg q 12 hr. Tinea capitis, corporis, or curis: 187.5 mg q 12 hr or 375 mg once daily SE transient HA, rash, GI, insomnia, tiredness, HEPATOTOXICITY, SJS, TENS, HYPERSENSITIVITY RXNS Med Administration Concerns taken w/ alcohol can result in tachycardia, flushing, and increased CNS depression , phenobarbitol may decrease effectiveness, Increased absorption by fatty foods; assess history of PCN rxns (cross rxn may exist) Pt Caregiver education Take complete regimen as prescribed (This med therapy is longer than others lasting weeks to months) , hygine to control sources of infection, dizziness (driving/fallprecautions), avoid alcohol nystatin (Mycostatin) Local (topical) antifungals Why is pt receiving this? Treatment of oropharyngeal and intestinal candidiasis. Alters membrane permeability of fungus Dosage Swish/swallow; losenges PO: 400,000-600,00 units 4 times daily as oral suspension 200,000-400,000 4-5 times daily as lozenges SE: minimal. Diarrhea, nausea, stomach pain, contact dermatitis, SJS Med administration conerns: no significant drug interactions; shake thoroughly before each dose, oral hygiene before each dose, swish and swallow Acyclovir (-cy/ciclovir) Antiviral ; purine analog Why is pt receiving this? Herpes Simplex Virus, Varicella Zoster Virus, Suppresses synthesis of viral DNA Dosage PO/IV varies based on infection and reccurence ; renal impairment dosage adjustments SE seizures, dizziness, HA, hallucinations, diarrhea, N/V, reversible nephrotoxicity, cyrstaluria, SJS, changes in menstruation, pain, phlebitis Med administration concerns Probenecid increases blood levels, theophylline increases risk of toxicity, decreases blood levels (may decrease effectiveness) of valporic acid or phenytoin. Additive nephrotoxic effects. Administered w/out regard to food w/ full glass of water (crystaluria), shake oral suspension before administration Pt caregiver education use of OTC creams/topical meds may delay healing and actually spread infection, acyclovir is no a cure, condoms should be used during sexual contact, women with herpes should undergo yearly Pap smears, avoid drug contact in eyes, zidovudine (Retrovir; AZT) Nucleoside Reverse Transcriptase Inhibitor (NRTI) Why is pt receiving this? HIV infection as part of “HIV cocktail” known as HAART (Highly Aggressive Anti-retroviral Therapy); acts as “analog” to nucleotide to bind with and inhibit HIV enzyme reverse transcriptase. Allows for increasing CD4 count to delay or prevent onset of AIDS. Dosage Mgmt of HIV infection: PO 100 mg q 4 hr while awake or 200 mg 3 times daily or 300 mg twice daily; IV: 1 mg/kg infused over 1 hr q 4 hr (change to oral therapy ASAP) ----------------------Prevention of Maternal/fetal transmission: Adults >14 weeks pregnant PO 100 mg 5 times daily until onset of labor, (during labor/delivery): IV: 2 mg/kg over 1 hr then continuous infusion of 1 mg/kg/hr until cord is campled SE Seizures, HA, weakness, anxiety, confusion, decreased mental acuity, dizziness, HEPATOMEGALY, PANCREATITIS, abd pain, diarrhea, nausea, LACTIC ACIDOSIS, fat redistribution, gynecomastia, anemia, granulocytopenia, neutropenia, Med administration concerns increased bone marrow depression w/ other agents, antineoplastics, and radiation therapy; increased nephrotoxicity w/ acyclovir; toxicity may be increased with Probenecid Pt caregiver education Instruct to take as directed, around the clock, even if sleep is disturbed. Importance of compliance of therapy and routine follow ups. May cause dizziness/fainting (driving, fall risk), not a cure for HIV, notify abnormal s/sx, redistribution and accumulation of body fat may occur (body image counseling), do not breast feed during therapy nevirapine (Viramune) Non-nucleoside Reverse Transcriptase Inhibitor (NNRTI) Why is pt receiving this? mgmt. of HIV in combination with NRTI as part of HAART; binds directly to reverse transcriptase to disrupt its effects ; post exposure prophylaxis (PEP) Dosage PO: varies based on either Immediate release or extended release; renal impairment dose adjustment SE HA, HEPATOTOXICITY, nausea, abd pain, rash (may progress to TENS), granulocytopenia, myalgia, paresthesia, SJS, fever Med Administration Concerns significantly decreases ketoconazole levels, decrease level and effectiveness of hormonal contraceptives, decreased by rifampin, may increase risk of bleeding w/ warfarin, use of prednisone w/in first two weeks may increase risk of rash, additive risk of rash w/ other drugs causing rash; DoNOTCrush extended release tabs, may be given w/out regard to food, if therapy is interrupted for 7 days or more, restart therapy Pt caregiver education Instruct to take as directed, around the clock, even if sleep is disturbed. Importance of compliance of therapy and routine follow ups. May cause dizziness/fainting (driving, fall risk), not a cure for HIV, notify abnormal s/sx, redistribution and accumulation of body fat may occur (body image counseling) indinavir (Crixivan) (-avir) Protease Inhibitor Why is pt receiving this? Mgmt of HIV infection w/ other antiretrovirals as part of HAART, post exposure prophylaxis (PEP) ; inhibits HIV protease which prevents cleavage of viral polyproteins Dosage PO 800 mg q 8 hr SE dizziness/drowsiness, fatigue, HA, insomnia, abd pain, acid regurg, alterted taste, asymptomatic hyperbillirubinemia, diarrhea HEPATOTOXICITY, nephrolithiasis, HYPERGLYCEMIA, HYPERLIPIDEMIA, FAT REDISTROBUTION, KETOACIDOSIS, back/flank pain increased bleeding in hemopheliacs, reduced bone mineral density, elevation of serum transaminases Med Admin Concerns increase risk of toxicity from amioderone, ergot derivatives, rifampin decreases blood levels, risk of myopathy w/ statins, blood levels increased by ketoconazole; HIGH FAT OR HIGH PRN MEALS decreases absorption administer w/ water 1 hr before or 2 hr after a meal. Pt/caregiver education Take as directed, important to adhere to regimen. If missed dose is within 2 hrs of next dose, skip dose and take next schedule dose; store in original container (sensitive to moisture), may cause kidney stones, may cause hyperglycemia, does not cure HIV, drowsiness/dizziness, body fat redistribution, avoid breastfeeding, importance of regular follow up enfuirtide (Fuzeon or T-20) Fusion inhibitor Why is pt receiving this? can be used w/ HAART, prevents HIV envelope from fusing w/ cell membrane of CD4 cell Dosage Sub Q 90 mg twice daily SE fatigue, conjunctivitis, cough, pna, sinusitis, diarrhea, nausea, abd pain, injection site reactions, myalgia, limb pain , HYPERSENSITIVITY, Med Admin concerns no drug/drug interactions