Treatment of CAP – Adults CID 2007:44(Suppl 2) S28
advertisement

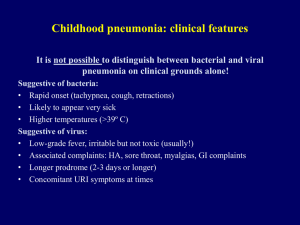
Treatment of CAP – Adults CID 2007:44(Suppl 2) S28-72 (Infectious Diseases Society of America/American Thoracic Society) Can J Infect Dis 2000;11:237-48 (Canadian Infectious Disease Society/Canadian Thoracic Society) Stanford Guide 2009 Outpatient Most Common Pathogens First Line Therapy Alternate Therapy No comorbid Strep pneumonia, Mycoplasma pneumonia, Haemophilus influenza, Chlamydophila pneumoniae Azithromycin/clarithromycin Doxycycline* Levofloxacin OR Ceftriaxone + azithromycin Azithromycin + amoxclavulin S. pneumonia, M. pneumonia, C. pneumoniae H. influenza, Legionella, ,Anaerobes S. pneumoniae Staphylococcus aureus (MSSA, CA-MRSA) Legionella species Gram-negative bacilli H. influenzae ICU bugs +MRSA Levofloxacin OR Ceftriaxone + azithromycin Levofloxaxin + ceftriaxone Levofloxacin + azithromycin Vancomycin + Levofloxacn Linezolid + Levofloxacin ICU bugs + p. aeruginosa Antipneumococcal, antipseudomonal β-lactamase° PLUS Ciprofloxacin or levofloxacin β-lactamase° + aminoglycoside + azithromycin OR β-lactamase° + aminoglycoside + cipro/levoquin Comorbid Abx in last 3 months macrolide resist strep pneumo (>25%) Inpatient Ward ICU§ ICU + suspect MRSA ICU + suspect pseudomonas Levofloxacin + piptazo *level III evidence § This is the minimal regime, often will require coverage of MRSA or pseudomonas. °pipercillin-tazobactam, cefepime, imipenem, meropenem 1 Etiology: In the patients managed as outpatients, M. pneumonia accounts for 15-37% of patients. It is likely strep pneumo is under diagnosed in this group. Strep pneumonia is accountable for about half of all cases requiring admission to hospital, followed by C. pneumonia and H influenza. Anaerobic gram negative bacilli like E-coli and Klebsiella are less common but are important to consider in patients who require ICU admission. They are also more common in a nursing home setting. Risk Factors / Features of CA-MRSA pneumonia Resistant to fewer antimicrobials than are hospital-acquired MRSA strains. Most produce a toxin associated with the clinical features of o necrotizing pneumonia o shock o respiratory failure F o formation of abscesses and empyemas (in patients without RF’s for anaerobic aspiration pneumonia) Risk Factors for Pseudomonas: Chronic oral steroid administration Severe underlying bronchopulmonary disease (ie COPD, asthma) Alcoholism Frequent antibiotic therapy Drug Resistant S. pneumonia: Resistance to numerous classes of antibiotics: penicillins, cephalosporins, macrolides, fluoroquinolones, tetracyclines, sulfonamides. Macrolide resistance in some parts of the world (ie Asia) approaches 50% Risk Factors: Unlcear on predictive values for these o Age <2 or >65 o Beta lactam therapy in last 3 months (most predictive) o Alcoholism, Immunosuppressive therapies or illness o Medical co-morbidities o Exposure to a child in daycare 2 Local S. Pneumoniae resistance Patterns 2010 from Calgary lab Services (% susceptible): o Penicillin 95% (was 83-91% 2009) o Ceftriaxone 95% o Erythromycin 78% o SXT 76% o Levofloxacin 86% o Tetracycline 87% Treatment of CAP – Pediatrics Paediatr Child Health. 2003:666-619 Alberta Clinical Practice Guideline 2008 Stanford guide 2009 Outpatient Most Common Pathogens First Line Therapy 1-3 month C. trachomatis, S. pneumonia, parainfluenzae, RSV, bordatella Streptococcus pneumoniae Erythromycin or Azithromycin Amoxicillin (80-90 mg/kg/day) Mycoplasma pneumoniae, Chlamydia pneumonia, S. pnemoniae Azithromycin 4mo – 5 yrs >5 yrs Alternative Therapy PCN allergy: azitho, clinda, or erythromycin Amoxicillin + Doxycycline (if > 8 yrs old) Amoxicillin + Clarithromycin Amoxicillin + erythromycin Inpatient Most Common Pathogens 1-3 month C. trachomatis, S. pneumonia, parainfluenzae, RSV, bordatella <5 yrs Streptococcus pneumoniae >5 yrs Mycoplasma pneumoniae, Chlamydia pneumonia, S. pnemoniae* Doxycycline if > 8 yrs old) Non-ICU Erythromycin or azithromycin Add cefuroxime or cefotaxime if febrile Ampicillin OR Cefotaxime OR cefuroxime Ceftriaxone + Azithro ICU Cefuroxime OR Cefotaxime + cloxacillin cefotaxime + azithromycin +/vancomycin Ceftriaxone + Azithro +/- Vanco (if evidence of lung necrosis) 3 Treatment of acute UTI and Pyelonephritis in Women CID 2011;52:e103-120 (Infectious Diseases Society of America/European Society for Microbiology and Infectious Diseases) Stanford Guide 2009 Uncomplicated UTI Most Common Pathogens First Line Therapy (TMP-SMX EColi resistance <20%) Outpatient management E. coli (75%–95%), Klebsiella pneumonia, Staph saprophyticus. Most Common Pathogens TMP-SMX° Nitrofurantoin* Fosomycin Outpatient E.Coli>enterococcus, Klebsiella pneumonia, Staph saprophyticus. Cipro / copro-ER PO TMP-SMX PO (treatment for 14days) Pyelonephritis Uncomplicated pyelo Alternative Therapy (TMP-SMX E-Coli resistance <20%, sulfa allergy) ciprofloxacin° ciprofloxacin-ER, nitrofurantoin Inpatient/ HPTP Gentamycin Ciprofloxacin IV Ceftriaxone Pip-tazo Ertapenem Non-ICU ICU *for use only in acute uncomplicated cystitis, NOT to be used in pyelonepthritis. Poor suppression of pathogens in periurethral, vaginal and rectal flora. °Know local resistance patterns Cystitis: TMP-SMX is still a recommended first guideline in areas with E-Coli resisntance <20% (in Calgary it is 21% 2010) Fosomycin is not effective against staph saprophyticus. o An anti-infective agent administered in a single 3g dose. o In vitro activity against VRE, MRSA, ESBL – still require clinical data o Not readily available, not often reported in routine susceptibilities. Β-lactms not recommended in treatment of acute uncomplicated cystitis. Local E-Coli susceptibility patterns: o Amoxicillin 55% o Cephalexin 73% o Cefazolin 94% 4 o o o o Ceftriaxone 97% TMP-SMX 79% Ciprofloxacin 94% Nitrofurantoin 98% Pyelonephritis: These recommendations are for acute uncomplicated pyelo only. Local E-Coli susceptibility patterns: o Pip/tazo 98% o Ceftriaxone 97% o TMP-SMX 79% o Ciprofloxacin 94% o Gentamycin 95% In Calgary, our ID experts have recommended that if we are going to treat a pyelonephritis we use gentamycin as a first line therapy. o Higher resistance patterns of ceftriaxone to E-Coli are being seen o Ceftriaxone excreted in bile (higher rate c. diff) compared to gentamycin excreted renally o No need to monitor gent levels in short 1-4 day course therapy o Toxicity very low with sort course, but a baseline creatinine is required. o Dose: 5-7 mg/kg LBW IV per day Lean Body Weight = (2.3 x height in inches over 5’ + 50kg M (45kg F)) o Exceptions, when to use ceftriaxone: (note that ceftriaxone does not cover enterococcus) Pregnant Renal impairment (GFR <60) Cirrhosis or liver transplant Previous aminoglycoside toxicity 5 Treatment of Acute Bacterial Meningitis Clinical Microbiology Reviews;2010:467–492 (Infectious Diseases Society of America) Paediatr Child Health;2008:309 (Canadian Paediatric Society) Stanford guide Patient Demographic Most Common Pathogens First Line Therapy Neonate (<1 mo) L. monocytogenes, E-Coli, Group B streptococcus, gram negative bacilli H. Influenza*, Strep. pneumoniae , N. meningitides Ampicillin +gentamycin OR Ampicillin +cefotaxime Cefotaxime or ceftriaxone + Vancomycinξ Healthy children >1 mo and Adults if Gram –ve bacilli on Gram stain Ampicillin + gentamycin + cefotaxime Meropenem + Vancomyin (+ Dexamethasone) Adults >50, immunocomprimised, alcoholic All of above + Enterobacteriaceae + Listeria monocytogenes (HIV +ve: staph aureus, salmonella) (+ Dexamethasone) Cefotaxime or ceftriaxone + Vancomycin + Ampicillin° (+ Dexamethasone) *Incidence of H. influenzus type b was dramatically reduced following vaccination. °For coverage of L. Monocytogenes ξThe addition of vancomycin is to provide double coverage of resistant S. pneumonia. Therapy can be narrowed based upon culture and sensitivity results 6 Treatment of Intra-abdominal sepsis Can J Infect Dis Med Microbiol. 2010;21:11-37 (Canadian Surgical Society/Association of Medical Microbiology and Infectious Disease Canada) CID 2010;50:133-164 (Guidelines from The Surgical Infection Society and the Infectious Diseases Society of America) Outpatient Most Common Pathogens Monotherapy Combination Community Acquired with no recent antimicrobial use (low to moderate severity)* Core pathogens: Streptococcus sp, Enterobacteriaceae ( E-coli, Klebsiella sp, Proteus sp, Serratia marcescens) + anaerobes (B. fragilis, nonfragilis Bacteroides sp, Clostridium sp, Fusobacterium sp, Lactobacillus sp, Peptostreptococcus sp, and Veillonella sp) Core pathogens + resistant G– bacilli, Enterococcus sp, P. aeruginosa, MRSA Cefoxitin or ertapenem, or moxifloxacin or tigecycline 2nd / 3rd cephalosporin + metronidazole ciprofloxacin + metronidazole Pip-tazo or Meropenem or imipenem 3rd / 4th cephalosporin +metronidazole ciprofloxacin + metronidazole Tigecycline + ciprofoxacin Pip-tazo + gent Meropenem + gent Community Acquired + recent antimicrobial use AND Health care associated +/recent antibiotic use AND Severely ill patients° *APACHE II <15 °APACHE II >15 Notes: Up to 15 different specimens can be cultured from same infected peritoneal cavity, and it is not always clear which ones are the key pathogens and which are commensals. Classification: o Uncomplicated (isolated organ system) o Complicated (infection beyond organ source + peritonitis) Community acquired Health care associated Primary – obvious source ie SBP, peritoneal dialysis Secondary – Soiling from hollow viscus ie. Perfed DU 7 Tertiary – recurrent infection Treatment of Skin and Soft tissue Infections CID 2005;41:1373-1406 (Infectious Diseases Society of America) CID 2011:52:18-55 (Infectious Diseases Society of America) Outpatient Most Common Pathogens β-hemolytic strep, strep B, C, G, staph aureus First Line Therapy Second Line Therapy Cephazolin/cephalexin Clindamycin or Clarithromycin, azithromycin or amox-clavulin, TMPSMX Cellulitis, purulent +MRSA RF’s β-hemolytic strep, strep B, C, G, staph aureus (MRSA) Diabetic, immunocomprimised β-hemolytic strep, strep B, C, G, staph aureus (MRSA), enterobacteriae, anaerobes TMP-SMX clindamycin Doxycycline Linezolid (mild-moderte) Clindamycin + gentamycin Or Clindamycin + Ciprofloxacin Cellulitis, non-purulent, no MRSA RF Severe) Vancomycin +piptazo Or Vanco/cipro/metroni dazole Inpatient Complicated cellulitis β-hemolytic strep, strep B, C, G, staph aureus Vancomycin Linezolid Daptomycin Notes: Complicated Skin and soft tissue infection: patients with deeper soft-tissue infections, surgical or traumatic wound infection, major abscesses, cellulitis, and infected ulcers and burns. RF’s for CA-MRSA: prison and jail inmates, injection drug users, Native American populations, gay men, participants in contact sports, and children 8 Treatment of postpartum endometritis Stanford Guide Population Most Common Pathogens First Line Therapy Second Line Therapy (includes both post C/S and post vaginal delivery)° G+: Group B streptococci,strep viridans, enterococci, G-: E. coli, P. bivia, anaer: bacteroides, aerobic streptococci, G. vaginalis, peptostreptococci other: C. trachomonatis, M. hominis (Cefoxitin or piptazo )+ doxycycline* Clindamycin + gentamycin Clindamycin + ceftriaxone °48hrs – 6 days MUST cover for C. trachomonatis *doxycycline cannot be administered during breastfeeding Pregnancy A) Controlled studies in women fail to demonstrate a risk to the fetus. B) Animal studies have not revealed toxicity but there are no adequate human studies, or animal studies have shown toxicity that was not confirmed in human studies. C) Animal studies have revealed toxicity and there are no adequate human studies, or studies in humans and animals are not available. Drug should only be given if potential benefit justifies the potential risk to the fetus. D) Positive evidence of human fetal risk, but the benefits from use in pregnant women may be acceptable despite the risk. X. Human and/or animal studies have shown a risk to the fetus, and risks outweigh benefits. Contraindicated in pregnancy. Lactation L1 = SAFEST: Drug used in a large number of breastfeeding women without affecting infant, or studies indicate that the possibility of harm to infant is remote, or the drug is not orally bioavailable in infants. L2 = SAFER: Drug used in a limited number of breastfeeding women without affecting infant, and/or risk to infant by using drug is remote. L3 = MODERATELY SAFE: There are no controlled studies. The risk of adverse effects in the infant is possible, or studies show only minimal non-threatening adverse reactions. Benefit versus risk to the infant must be considered. L4 = POSSIBLY HAZARDOUS: There is evidence of risk to the breastfed infant or breast milk production, but the benefits to the mother may outweigh the risk to the infant (e.g. in life-threatening situations or when safer drugs cannot be used). L5 = CONTRAINDICATED: Studies show a significant and documented risk to infants, or it is a drug that has a high risk of causing significant infant harm. The drug is contraindicated in breastfeeding, as the possible harm to the infant outweighs any potential 9 benefits from breastfeeding. AAP ratings: Recommendations from American Academy of Pediatrics (AAP), published in Pediatrics 2001;108:776-89. AAP ratings: Recommendations from American Academy of Pediatrics (AAP), published in Pediatrics 2001;108:776-89. = approved drug is usually compatible with breastfeeding. Breastfeeding and Lactation Guidelines Briggs GG, et al. Drugs in pregnancy and lactation. 7th ed. 2005/FDA Antibiotic Safe Pregnancy Safe Lactation Penicillins Pipercillin-Tazobactam Cephaolsporins Meropenem Aminoglycosides B B B B C L1 L2 L1/2 L3 L2 Azithromycin B L2 Clarithromycin Fluoroquinolones C C L2 L3 (Do not use) CLindamycin B L3 Metronidazole Nitrofurantoin B (NOT in 1st trimester) B (NOT in 3rd trimester) L2 L2 Sulfonamides C / D 3rd trimester L3 Tetracyclines Vancomycin D B L3/L4 (DO NOT use) L1 Notes (small amount excreted into milk, clinically not significant levels in infant) (small amount excreted, clinically not significant levels in infant) Greenish discoloration of teeth (infant may develop diarrhea) -G6PD and term fetuses may develop hemolytic anemia -G6PD and term fetuses may develop hemolytic anemia 10