Depression

The Return of Electroshock Therapy
O NE MORNING in early October, on her final day as the chair of the psychiatry and behavioral-sciences department at the Duke University School of Medicine, Sarah
Hollingsworth Lisanby ushered me over to a display case in one of the department’s conference rooms. There, behind glass, sits the world’s only museum, such as it is, of electroconvulsive therapy (ECT), or what most people still call “shock therapy.”
The oldest artifacts on display, some of which are made of polished wood and brass, date to the late 19th century, when electrical stimulation was promoted as a cure for a host of ailments. A mid-20th-century relic labeled ELECTRO SHOCK
THERAPY EQUIPMENT features a red button in the center helpfully marked START
SHOCK .
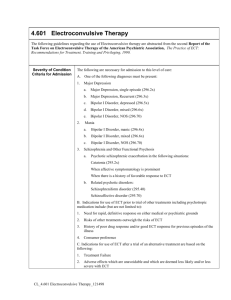
In the popular imagination, ECT—the application to the scalp of an electrical current strong enough to induce a brief seizure—is an archaic practice that might as well be relegated to a museum collection. But according to Lisanby and other leading researchers, the modern version of ECT, far from outmoded, is the most effective therapy available for severe, treatment-resistant depression and bipolar disorder (and even sometimes, when deployed early enough, schizophrenia). No one knows exactly why ECT works—there are many theories—but numerous studies have established that it does work: The vast majority of severely depressed, even suicidal, patients feel much better after a course of treatment. Many experience a total remission. Refinements over the past few decades, moreover, have dramatically reduced the temporary memory loss once associated with ECT.
And yet, due largely to the stigma surrounding the treatment, only a tiny fraction of the millions of Americans with depression unresponsive to psychotherapy or medication ever receive it.
NE MORNING in early October, on her final day as the chair of the psychiatry and behavioral-sciences department at the Duke University School of Medicine, Sarah
Hollingsworth Lisanby ushered me over to a display case in one of the department’s conference rooms. There, behind glass, sits the world’s only museum, such as it is, of electroconvulsive therapy (ECT), or what most people still call “shock therapy.”
The oldest artifacts on display, some of which are made of polished wood and brass, date to the late 19th century, when electrical stimulation was promoted as a cure for a host of ailments. A mid-20th-century relic labeled ELECTRO SHOCK
THERAPY EQUIPMENT features a red button in the center helpfully marked START
SHOCK .
In the popular imagination, ECT—the application to the scalp of an electrical current strong enough to induce a brief seizure—is an archaic practice that might as well be relegated to a museum collection. But according to Lisanby and other leading researchers, the modern version of ECT, far from outmoded, is the most effective therapy available for severe, treatment-resistant depression and bipolar disorder (and even sometimes, when deployed early enough, schizophrenia). No one knows exactly why ECT works—there are many theories—but numerous studies have established that it does work: The vast majority of severely depressed, even suicidal, patients feel much better after a course of treatment. Many experience a total remission. Refinements over the past few decades, moreover, have dramatically reduced the temporary memory loss once associated with ECT.
And yet, due largely to the stigma surrounding the treatment, only a tiny fraction of the millions of Americans with depression unresponsive to psychotherapy or medication ever receive it.
In the popular imagination, ECT is an archaic practice that might as well be relegated to a museum collection.
After several years of collaboration with researchers around the world, Lisanby had put together a magnetic device that she believed would be capable of inducing seizures in humans; all she needed was a person to test it on. A 20-year-old Swiss woman whose depression had not responded to standard treatments volunteered, and in April 2000, Lisanby shipped her heavy, one-of-a-kind equipment to the
University of Bern. She was about to fly over herself when one of her Swiss collaborators, Thomas Schlaepfer, called. “I have good news and bad news,” he told her. “The device arrived, but it’s in a thousand pieces.” With just days to go before the procedure, Lisanby had to lug some of the replacement parts in her baggage.
“Luckily it was before 9/11,” Lisanby recalled, “so the oscilloscope went right through security.”
Schlaepfer told me that he and Lisanby were nervous before the procedure. “There was still an edge in me saying, It might be dangerous . Did we calculate everything correctly?
” he confessed. “But it went absolutely fine.” The patient had four sessions of magnetic seizure therapy and eight regular ECT sessions, then went into full remission.
Multiple studies later, magnetic seizure therapy appears to be about as effective as ECT in relieving depression, while causing almost no discernible memory loss. Even so, the treatment remains unapproved for use in Europe and the U.S. The problem is that the small companies that build magnetic-seizure-therapy devices have not undertaken the kind of large, randomized trial the FDA would require before approving them for use outside of studies. Lisanby, however, has recently completed a new trial that she hopes will keep the ball moving.
In 2005, Lisanby became the founding director of Columbia’s division for brain stimulation and neuromodulation. By the time she moved to Duke in 2010, she had co-authored some 150 scientific papers and book chapters and served as president of two international professional organizations on brain stimulation.
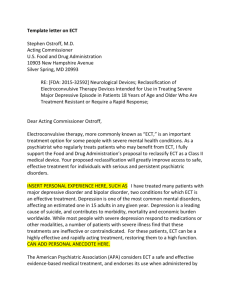
When the FDA held a hearing in 2011 to consider reclassifying ECT from Class III, its highest risk designation, to Class II, Lisanby testified as the chair of an American Psychiatric Association task force on ECT. “I’m here to deliver one critical point,” she told the panel. “Depression kills, while ECT saves lives.” She rattled off statistics. She reviewed decades of data. And, on a more personal note, she added, “I’m also the family member of a person whose life was saved by ECT.”
Each time Lisanby walked in and out of the room that day, an anti-ECT advocate in the audience made a buzzing noise, in an effort to imitate an ECT device. (In fact, the devices make no such sound.) In the end, despite all the testimony from Lisanby and many others, and despite the evidence from randomized trials involving hundreds of patients, the panel did not recommend reclassification.
To be fair, the reality of ECT early on—when stronger, less targeted jolts of electricity were given without the benefit of anesthesia—was brutal. But today, Lisanby and other leading practitioners insist, memory loss tends to be relatively mild. The treatment’s chief drawback, for now, is that without maintenance therapy (whether drugs or more ECT), its benefits last many patients only about six months to a year.
So why aren’t more doctors prescribing ECT? “Why indeed,” says Thomas Insel, the recently departed director of NIMH who recruited Lisanby. (He is headed to Google Life Sciences, which is looking to expand into mental-health care.) “If we were talking about Alzheimer’s, and I had a treatment that would largely resolve the major symptoms within six weeks 80 percent of the time, and then I told you this treatment is not accessible in many parts of the country and rarely used where it is available, you would say that can’t be.”
Insel hired Lisanby, he told me, in part because she has “a modern view of mental illness.” Through the 1970s, mental illness was seen as resulting primarily from early trauma and adverse experiences; the treatment was psychotherapy. Beginning in the 1980s, it was regarded as an imbalance of neurotransmitters, best treated with medication.
“Depression kills, while ECT saves lives.”
The public’s understanding of how ECT works, on the other hand, plainly frustrates
Lisanby. When the conversation shifted to the therapy’s reputation, Lisanby turned and, to my surprise, asked me whether a term like electro-seizure therapy would be more appealing than electroconvulsive therapy . After all, she pointed out, people don’t actually go into convulsions anymore, thanks to the muscle relaxants.
“Um,” I said, “I’m not sure that seizure has a lot of positive connotations.”
“Maybe,” she replied, “we should convene some consumer focus groups to find out how they respond to the name.” I was half joking; Lisanby, understandably, wasn’t.
A therapy with the power to transform lives goes unused in part because people recoil at its name. And yet, one study found that among people who had undergone the treatment, 98 percent said they would do it again if their depression recurred.
Maybe, under the circumstances, new terminology isn’t such a crazy idea.
When Lisanby and I talked again, a bit later in October, it was by phone—she had left North Carolina for Maryland, and was busy getting settled at NIMH. She’d had a great first week, she said, and was in the midst of planning new collaborations with scientists there
I hadn’t been able to stop wondering about the family member whose experience with ECT she’d guardedly mentioned in her FDA testimony, so I asked her whether she would tell me the story. She hesitated briefly.
“My grandfather had ECT, before I was born, in the 1950s,” she said. “It was before anesthesia, back when the dosing was so much higher and so many other things were different.” She paused. “I believe he would not have been alive for me to get to know him had it not been for ECT.”