134_2013_2906_MOESM22_ESM
advertisement
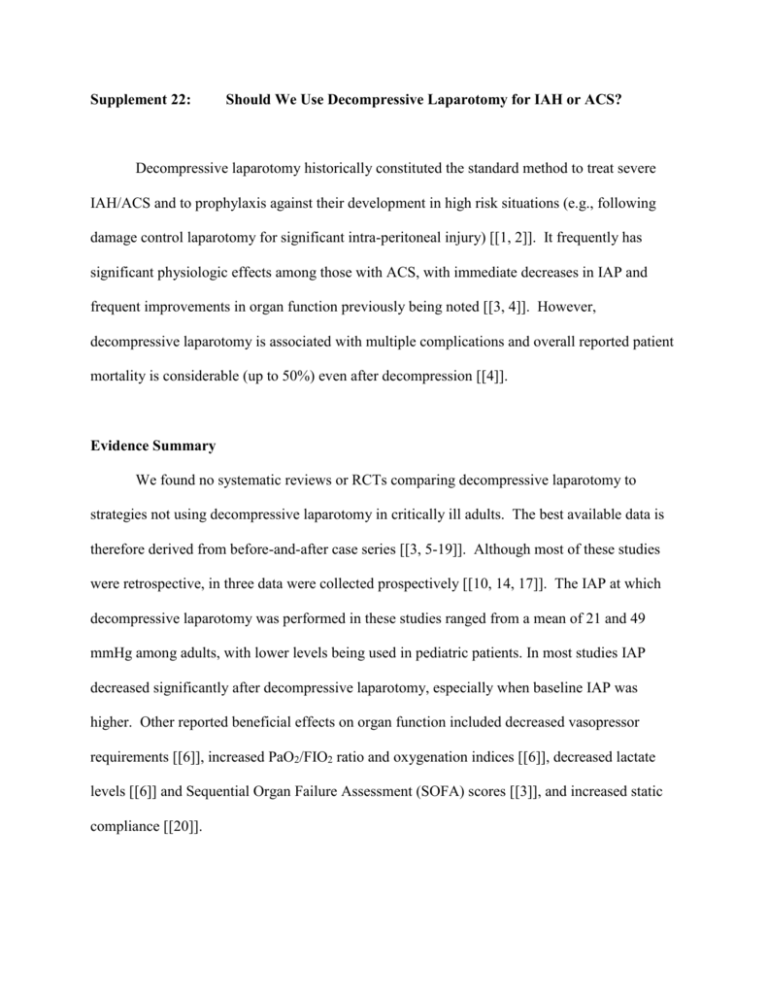
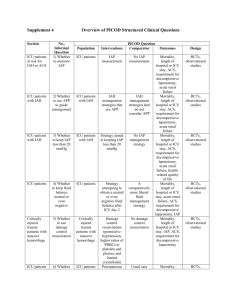
Supplement 22: Should We Use Decompressive Laparotomy for IAH or ACS? Decompressive laparotomy historically constituted the standard method to treat severe IAH/ACS and to prophylaxis against their development in high risk situations (e.g., following damage control laparotomy for significant intra-peritoneal injury) [[1, 2]]. It frequently has significant physiologic effects among those with ACS, with immediate decreases in IAP and frequent improvements in organ function previously being noted [[3, 4]]. However, decompressive laparotomy is associated with multiple complications and overall reported patient mortality is considerable (up to 50%) even after decompression [[4]]. Evidence Summary We found no systematic reviews or RCTs comparing decompressive laparotomy to strategies not using decompressive laparotomy in critically ill adults. The best available data is therefore derived from before-and-after case series [[3, 5-19]]. Although most of these studies were retrospective, in three data were collected prospectively [[10, 14, 17]]. The IAP at which decompressive laparotomy was performed in these studies ranged from a mean of 21 and 49 mmHg among adults, with lower levels being used in pediatric patients. In most studies IAP decreased significantly after decompressive laparotomy, especially when baseline IAP was higher. Other reported beneficial effects on organ function included decreased vasopressor requirements [[6]], increased PaO2/FIO2 ratio and oxygenation indices [[6]], decreased lactate levels [[6]] and Sequential Organ Failure Assessment (SOFA) scores [[3]], and increased static compliance [[20]]. Recommendation The WSACS RECOMMENDS the use of decompressive laparotomy to reduce IAP in cases of overt ACS compared to strategies that do not use decompressive laparotomy in critically ill adults with ACS in critical care units (Management Recommendation 5; GRADE 1D). Rationale: These studies were limited by risk of bias and inconsistency in the effect of decompressive laparotomy on IAP. Moreover, no study was able to examine the effect of decompressive laparotomy on patient-important outcomes such as mortality. While the overall quality of evidence describing the effect of decompressive laparotomy on outcomes was very low (D), decompressive laparotomy is frequently associated with a profound reversal of abnormal patient physiology. A Summary of Studies Table is available online at References 1. 2. 3. 4. Kirkpatrick AW, Ball CG, D'Amours SK, Zygun D, (2008) Acute resuscitation of the unstable adult trauma patient: Bedside diagnosis and therapy. Can J Surg 51: 57-69 Sugrue M, D'Amours SK, Joshipura M, (2004) Damage control surgery and the abdomen. Injury 35: 642-648 De Waele J, Desender L, De Laet I, Ceelen W, Pattyn P, Hoste E, (2010) Abdominal decompression for abdominal compartment syndrome in critically ill patients: A retrospective study. Acta Clin Belg 65: 399-403 De Waele JJ, Hoste EA, Malbrain ML, (2006) Decompressive laparotomy for abdominal compartment syndrome--a critical analysis. Crit Care 10: R51 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. Steinau G, Kaussen T, Bolten B, Schachtrupp A, Neumann UP, Conze J, Boehm G, (2011) Abdominal compartment syndrome in childhood: diagnostics, therapy and survival rate. Pediatric surgery international 27: 399-405 Pearson EG, Rollins MD, Vogler SA, Mills MK, Lehman EL, Jacques E, Barnhart DC, Scaife ER, Meyers RL, (2010) Decompressive laparotomy for abdominal compartment syndrome in children: before it is too late. Journal of pediatric surgery 45: 1324-1329 Zhou JC, Xu QP, Pan KH, Mao C, Jin CW, (2010) Effect of increased intra-abdominal pressure and decompressive laparotomy on aerated lung volume distribution. Journal of Zhejiang University Science B 11: 378-385 Mentula P, Hienonen P, Kemppainen E, Puolakkainen P, Leppaniemi A, (2010) Surgical decompression for abdominal compartment syndrome in severe acute pancreatitis. Archives of surgery 145: 764-769 Mayer D, Rancic Z, Meier C, Pfammatter T, Veith FJ, Lachat M, (2009) Open abdomen treatment following endovascular repair of ruptured abdominal aortic aneurysms. Journal of vascular surgery : official publication, the Society for Vascular Surgery [and] International Society for Cardiovascular Surgery, North American Chapter 50: 1-7 Batacchi S, Matano S, Nella A, Zagli G, Bonizzoli M, Pasquini A, Anichini V, Tucci V, Manca G, Ban K, Valeri A, Peris A, (2009) Vacuum-assisted closure device enhances recovery of critically ill patients following emergency surgical procedures. Critical care 13: R194 Joseph DAK, Dutton R, Scalea T (2003) Decompressive laparotomy to treat intractable intracranial hypertension after traumatic brain injury. In: Editor (ed)^(eds) Book Decompressive laparotomy to treat intractable intra-cranial hypertension after traumatic brain injury. City, pp. Balogh Z, McKinley BA, Holcomb JB, Miller CC, Cocanour CS, Kozar RA, Valdiva A, Ware DN, Moore FA, (2003) Both primary and secondary abdominal compartment syndrome can be predicted early and are harbingers of multiple organ failure. J Trauma 54: 848-861 McNelis J, Soffer S, Marini CP, Jurkiewicz A, Ritter G, Simms HH, Nathan I, (2002) Abdominal compartment syndrome in the surgical intensive care unit. Am Surg 68: 18-23 Raeburn CD, Moore EE, Biffl WL, Johnson JL, Meldrum DR, Offner PJ, Franciose RJ, Burch JM, (2001) The abdominal compartment syndrome is a morbid complication of postinjury damage control surgery. Am J Surg 182: 542-546 Biffl WL, Moore EE, Burch JM, Offner PJ, Francoise RJ, Johnson JL, (2001) Secondary abdominal compartment syndrome is a highly lethal event. Am J Surg 182: 645-648 Ertel W, Oberholzer A, Platz A, stocker R, Trentz O, (2000) Incidence and clinical pattern of the abdominal compartment syndrome after "damage control" laparotomy in 311 patients with severe abdominal and/or pelvic trauma. Crit Care Med 28: 1747-1753 Chang MC, Miller PR, D'Agostino R, Jr., Meredith JW, (1998) Effects of abdominal decompression on cardiopulmonary function and visceral perfusion in patients with intra-abdominal hypertension. The Journal of trauma 44: 440-445 Sugrue M, Jones F, Janjua KJ, Deane SA, Bristow P, Hillman K, (1998) Temporary abdominal closure: A prospective evaluation of its effects on renal and respiratory physiology. J Trauma 45: 914-921 Platell CF, Hall J, Clarke G, Lawrence-Brown M, (1990) Intra-abdominal pressure and renal function after surgery to the abdominal aorta. Aust N Z J Surg 60: 213-216 Balogh Z, McKinley BA, Holcomb JB, Miller CC, Cocanour CS, Kozar RA, Valdivia A, Ware DN, Moore FA, (2003) Both primary and secondary abdominal compartment syndrome can be predicted early and are harbingers of multiple organ failure. J Trauma 54: 848-859; discussion 859-861