Medicaid Behavioral Services for Children Outline

Medicaid Behavioral Services for Children
Nancy E. Wright, Esq. Newright.law@gmail.com
GAL Video Training 2015
1. A Confusing Assortment of Services
Eligibility varies by
Age
Diagnosis or condition
Living arrangement
Dependency status
Access varies by
Agency (and prior authorization contractors)
MCO and available network providers
ALL REQUIRE MEDICAID ELIGIBILITY
2. Child Welfare-Related
Special services offered only to children in the child welfare system
A. Medical Foster Care
Eligibility:
Medically complex (has chronic debilitating disease or
condition of 1 or more physiological or organ
systems that generally make person dependent on
24 hr medical, nursing, health supervision or
intervention) or
Medically fragile (medically complex + tech dependent
or needs heightened medical supervision)
Under 21 and in DCF custody
CMAT recommendation of MFC and Level of
Reimbursement (I, II, or III)
Operated through DOH/CMS regardless of type of
Medicaid enrollment
B. Child Health Services Targeted Case Management
Eligibility:
Age birth to 3 years and getting services from either
Early Steps or
In Medical Foster Care
Not getting Waiver services, ICF/DD or nursing home
Services:
Assessment of needs, assisting in access to medical,
social, education and other services
C. Specialized Therapeutic Foster Care Comprehensive Behavioral
Assessment
1
Eligibility for comprehensive behavioral assessment :
Under 21 and either
DCF out of home placement or sheltered and
Victim of abuse or neglect OR
Committed acts of juvenile delinquency,
Has emotional or serious emotional disturbance, AND is at risk for placement in residential setting
Available through MMA
D. Emotional Disturbance defined
Emotional Disturbance:
Diagnosed with mental, emotional or behavioral
disorder
Sufficient duration to meet most recent DSM
Behaviors don’t substantially interfere with or limit
function
Not temporary response to stressful situation
Serious Emotional Disturbance:
Same as above, but behaviors substantially interfere
with or limit function in family, school or community
E. STFC Services Level I or II
Authorized by multidisciplinary team (DCF or designee, local
Medicaid office and DJJ if applicable, plus others) OR
Available through MMA
Level I:
History of abuse, neglect or delinquent
behavior
Have an emotional disturbance
Either requires admission to psychiatric
hospital, CSU or residential treatment center
or been admitted in last two years
Level II:
Meets Level I plus exhibits more severe
behaviors, like property destruction, physical
aggression, SIB, suicidal ideation, or
functional inability to perform ADLs due to
psychiatric symptoms
F. STFC: Therapeutic Group Care Services
Eligibility:
Under 21
Resident of licensed residential group home
Has moderate to severe emotional disturbance
Services:
2
Community-based psychiatric residential treatment
Individualized treatment plan, including psychiatric
and therapy services, behavioral management,
social and rehabilitative services, substance abuse
treatment, etc.
Available through MMA
G.
Children’s Mental Health Targeted Case Management
Mental Health Targeted CM Handbook
Eligibility (via certification by a case manager and
supervisor):
Birth through 17, enrolled in a DCF mental health target
population
Has serious emotional disturbance that is likely to last at
least a year
Requires services for self sufficiency
Lacks a natural support system
Requires ongoing help to maintain needed care
Is in out-of-home MH placement or at risk
H. Behavioral Health Overlay
Services:
Mental health, substance abuse and supportive
services (therapy, behavior management,
therapeutic support) to meet needs of those in care
of DCF, Child Welfare or CBC
Assessment and Individual treatment plan
Available through MMA
Eligibility:
Has emotional or serious emotional disturbance
At risk due to ONE of 5 factors in last year
(suicidal/SIB, aggression toward people, animals or
property, run away or threatened, sexual aggression,
experienced trauma
3. Behavioral Health Services
Available to all children on Medicaid
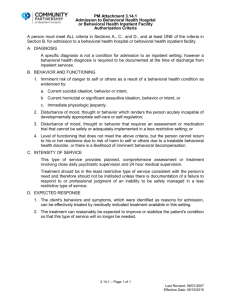
A. State In-Patient Psychiatric (SIPP)
F.A.C. Rule 59G-4.120, in proposed rule status
Services: Extended residential psychiatric treatment
Available through MMA
Eligibility:
Under age 21
Has emotional or serious emotional disturbance
3
Acute inpatient or intensive outpatient services cannot
resolve symptoms
Approval through DCF Substance Abuse and Mental
Health (SAMH) Program Office.
B. Community Behavioral Health Services (CBHS) Handbook
Includes both mental health and substance abuse services
I ntended for the “maximum reduction of the recipient’s
disability and restoration to the best possible functional level”
Available through MMAs
Not available for treatment of a cognitive deficit severe
enough to prohibit the service from being of benefit to the
recipient
C. CBHS: Assessment and Treatment Plan
Assessment required to develop treatment plan. Types:
psychiatric evaluation or record review, brief behavioral, in-
depth, bio-psychosocial, psychological, limited functional
Eligibility: Each type of assessment has its own explanation
of need
Treatment Plan and Modification required for all community
behavioral health services
D. CBHS: Medical and Psychiatric Services
Services:
Medication management
Brief individual medical psychotherapy
Brief group medical therapy
Behavioral health-related medical screening, verbal
interactions, alcohol and other drug testing
Medication assisted treatment
E. CBHS: Behavioral Health Therapies
Services:
Individual and family cognitive or supportive therapy
Group therapy
Eligibility: No age limit, medically necessary
Behavioral health day services
Eligibility: Age 2 through 5 with at least moderate impairment on behavioral or
functional rating scale
F. CBHS: Community Support & Rehabilitation Services
Psychosocial rehabilitation: to strengthen or regain
interpersonal and daily living skills
4
Eligibility: Having psychiatric, behavioral, cognitive or
clinic conditions significantly impairing personal,
social or educational functioning
Clubhouse services: structured group rehab services
Eligibility: At least 16 year old with mental health
diagnosis
G. CBHS: Therapeutic Behavioral On-Site Services
Intensive therapy, behavioral management and therapeutic
support services in the home
Eligibility:
Under 21 and in the home (permanent or
foster)
Criteria differs depending on age, but generally
having emotional or serious emotional
disturbance
Assessment indicates need for intensive,
therapeutic behavioral on-site services to
prevent more restrictive placement
Family agrees to services
H. Applied Behavior Analysis (ABA)
No Handbook yet
Required by federal court ( Garrido v Dudek
Not currently provided through MCOs
)
Must be authorized through AHCA Area Office
Eligibility:
Under 21
Diagnosed with Autism Spectrum Disorder
Prescribed by physician
Services:
CBA Assessment, Behavioral Plan, and
Intervention
Behavioral Assistant Services
5