May 2014 Large Animal Benchmark
pCO
2
PO
2
HCO
3
-
BE
Na +
K +
Ca ++
Cl -
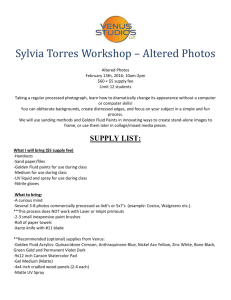
Large Animal Benchmark
May 2014
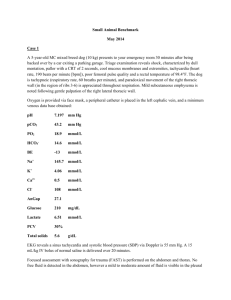
CASE 1:
A 15-year-old Quarter horse gelding (500 kg) presents to your clinic 30 minutes after being hit by a
Suburban traveling at 60 miles per hour. The horse walks into your clinic with a normal gait. Triage examination reveals signs of shock, characterized by dull mentation, mucous membrane pallor with a
CRT of 3 seconds, cool extremities, tachycardia (heart rate, 110 beats per minute), poor facial arterial pulse quality and a rectal temperature of 98.4
F. The horse is tachypneic (respiratory rate, 60 breaths per minute), and paradoxical movement of the right thoracic wall (in the region of ribs 13-16) is appreciated throughout respiration. Mild subcutaneous emphysema is noted following gentle palpation of the right lateral thoracic wall. A 5 cm laceration was noted in the right axilla.
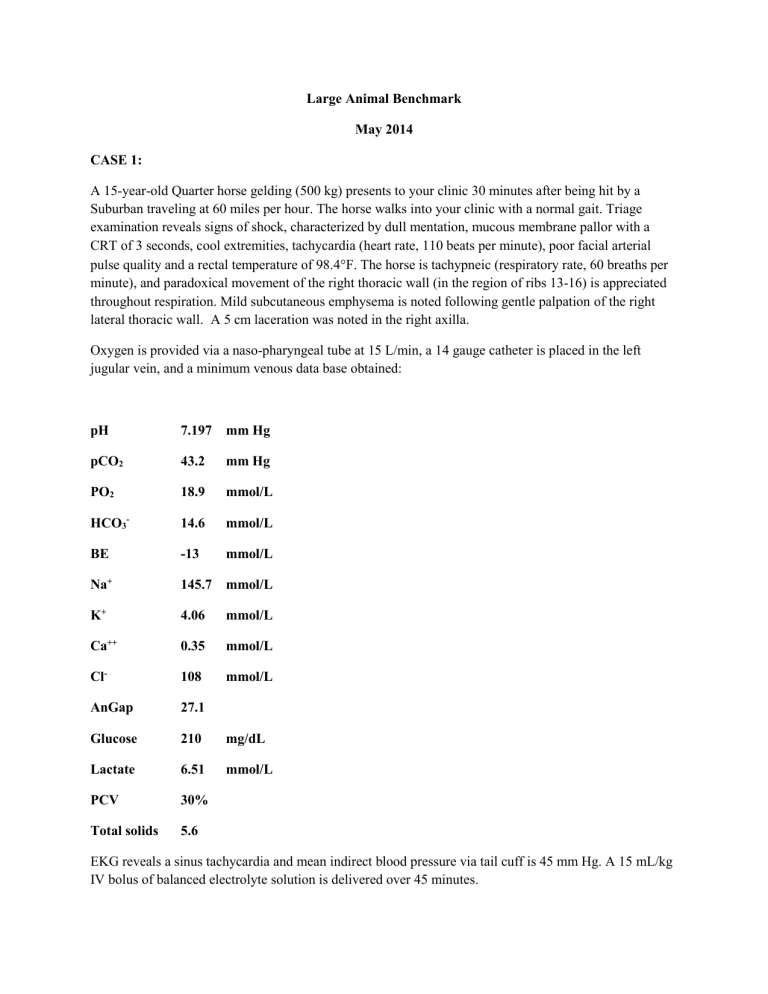
Oxygen is provided via a naso-pharyngeal tube at 15 L/min, a 14 gauge catheter is placed in the left jugular vein, and a minimum venous data base obtained: pH 7.197 mm Hg
43.2 mm Hg
18.9 mmol/L
14.6 mmol/L
-13 mmol/L
145.7 mmol/L
4.06
0.35
108 mmol/L mmol/L mmol/L
AnGap
Glucose
Lactate
PCV
27.1
210
6.51
30% mg/dL mmol/L
Total solids 5.6
EKG reveals a sinus tachycardia and mean indirect blood pressure via tail cuff is 45 mm Hg. A 15 mL/kg
IV bolus of balanced electrolyte solution is delivered over 45 minutes.
Based on a recent publication on fluid administration rates in the horse, describe the maximum rate that could be acquired in vivo using a 14 gauge catheter. What affects fluid rates, and what combination of fluid delivery set could give the highest flow rate?
Focused assessment with sonography for trauma (FAST) is performed on the abdomen and thorax. No free fluid is detected in the abdomen, however a mild to moderate amount of fluid is visible in the pleural cavity.
No pneumothorax or pericardial effusion is noted. The remainder of the thoracic cavity is fully examined with the ultrasound.
Describe the abnormalities noted in the following image obtained during that exam, labeled H: www.ultrasound-images.com
What are your tentative radiographic and clinical diagnoses?
Assign this horse an Animal Trauma Triage (ATT) score, extrapolated from the canine scoring system. Provide an evidence-based description of the utility of this scoring system in outcome prediction in veterinary trauma patients.
List 10 predictors of non-survival in dogs suffering from blunt trauma.
What is this horse’s Shock Index (SI)? Briefly discuss the utility of this parameter in assessment in dogs presenting to the emergency room.
Define flail chest.
What are the postulated mechanisms responsible for respiratory distress in patients diagnosed with flail chest?
Outline your initial management strategy specifically for this patient’s flail chest.
If conservative management fails, and surgical stabilization of the flail segment is indicated, briefly describe the technique you would choose for this patient.
You perform an ECG on the horse, and note this rhythm. What is the rhythm and what additional diagnosis should you include on your problem list? http://largeanimal.vethospitals.ufl.edu/
What are reported concurrent injuries associated with and consequences of this type of traumatic injury? What monitoring tools can be utilized for documentation of injury progression or resolution?
Heart rate remains elevated at 120 bpm despite adequate level of analgesia and normoxia (SPO
2
of 94%,
[FiO
2
estimated at 40%]). Mean blood pressure after initial isotonic crystalloid bolus is 50 mm Hg.
Follow-up PCV and TS are 20% and 3.5 g/dl, respectively. Repeat abdominal and thoracic FAST examinations reveal a static pleural effusion, but now moderate peritoneal effusion is visible. Diagnostic abdominocentesis is performed and a hemoperitoneum is confirmed (PCV of the fluid in the peritoneal cavity = 15%).
You check a PT and PTT. Both are out of the reference range.
Outline three hypotheses for the pathophysiology of acute traumatic coagulopathy (ATC).
List six key factors that have been shown to influence ATC. Of these six, which two have been globally accepted as the main initiators of ATC?
Briefly describe the purported difference put forth by some authors between ATC and traumainduced coagulopathy (TIC):
You suspect that your patient has ATC. How could you demonstrate a hyperfibrinolytic state in this patient?
Which of the following was recently demonstrated in a study evaluating the coagulation status of 40 dogs within 12 hours of severe acute trauma?
List two drugs which could be utilized to treat hyperfibrinolysis associated with ATC.
Briefly discuss mechanism/s of action and effects of these anti-fibrinolytic medications in horses, as well as the metabolism and potential adverse effects of these drugs.
You ask your senior clinician for their opinion on using an anti-fibrinolytic agent in your patient.
This person references a paper on the 2014 ACVECC Additional Journal Article List that was published in The Lancet in 2010. Briefly outline the major findings of the CRASH-2 trial.
Both anti-fibrinolytic medications are unavailable to you for immediate use. Your patient has a coagulopathy and clinical signs you deem referable to his anemia. Outline and justify your transfusion plan for this patient. Include in your answer blood products selected and product dosages and ratios.
CASE 2:
A 16-year old Warmblood mare is undergoing ventral midline laparotomy for cesarean section of a full term, breach presentation foal. She was admitted to your hospital one week prior for foal watch, and has been in labor approximately 15 minutes according to the technical staff. Preoperative blood work is within normal limits. Physical examination reveals no significant abnormalities and a 2/6 left apical holosystolic murmur. Anesthetic induction is uneventful.
With the patient under general anesthesia, an arterial catheter is placed in the right facial artery to facilitate monitoring of hemodynamics and respiration.
Briefly describe your technique for assembling, zeroing and leveling the electronic direct arterial pressure monitoring system.
Diagram and identify the major components of an idealized central arterial pressure waveform.
Superimpose on your diagram the expected changes as the pressure wave moves toward the periphery.
Define pulse pressure.
What is the most common cause of a low (narrow) pulse pressure?
List 3 specific causes of a high (wide) pulse pressure.
How is the mean arterial pressure (MAP) calculated using the systolic arterial blood pressure
(SAP) and diastolic arterial blood pressure (DAP)?
How is this accuracy of this calculation affected by patient heart rate?
Identify and briefly describe the test being performed below:
List 1 cause each for an underdamped and an overdamped fluid-filled monitoring system.
Underdamped:
Overdamped:
Your anesthesia technician informs you that the horse’s MAP has decreased to 40 mm Hg. A fluid challenge of 10 ml/kg of balanced electrolyte solution is administered over 15 minutes with no change in
MAP. The anesthesiologist enters the surgical suite and suggests that pulse pressure variation be determined in this patient.
Describe the theory behind and potential clinical utility of pulse pressure variation (PPV) in anesthetized patients.
This patient’s PPV is 21%. What does this indicate?
Increasing preload in this patient via a fluid bolus (5 ml/kg of Hetastarch) resulted in restoration of normotension (MAP, 85 mm Hg). This improvement in perfusion is likely due to augmentation of the patient’s cardiac output.
What cardiovascular factors contribute to a patient’s cardiac output?
Describe the difference between cardiac output and cardiac index.
What is the normal range for the cardiac index in a horse?
List 5 instruments specifically used for measurement of cardiac output (CO). Provide one limitation for each methodology listed.
Instrument Limitation
Using a pulmonary artery catheter (PAC), 2 methods can be used to measure CO. Name them and briefly describe how these techniques work.
Once the cardiac output is measured, Oxygen Delivery (DO
2
) and Oxygen Consumption (VO
2
) can be calculated. What are the formulas for calculating these two oxygen derived variables?
While the patient is being prepared for surgery there is an acute rise in heart rate and fall in blood pressure, this is associated with pallor of the mucous membranes. There is concern there has been a rupture of the uterine artery.
If cardiac output was being measured in this patient would you expect the CO to increase, decrease or stay the same in this situation?
Define systemic vascular resistance (SVR) and provide a formula for its calculation following determination of patient CO.
In this patient would you expect the systemic vascular resistance (SVR) to increase, decrease or stay the same?
What are the locations of the arterial and cardiopulmonary baroreceptors?
Using a diagram show how does the baroreceptor reflex works to maintain normal blood pressure?
You elect to use hypotensive resuscitation in this patient. Describe the principle of hypotensive resuscitation, what are the advantages of this resuscitation strategy, and indicate why it can be used safely in this patient.
What type of suture should be used to close the uterine incision?
List 10 detrimental effects of liberal peri-operative fluid administration and fluid overload in human (and likely veterinary) surgical patients.
Differentiate between type 1 and type 2 fluid shifts out of the intravascular space toward the interstitium in the perioperative period.
Briefly describe the revised Starling equation and glycocalyx model of transvascular fluid exchange as this pertains to perioperative fluid prescriptions.
List at least 3 inflammatory mediators that have been implicated to result in compromise of the
EGL.
There have been several proposed and experimental therapies that target the glycocalyx for protection and/or restoration. List 3 of these options.
The End