click here to the male health history form
advertisement
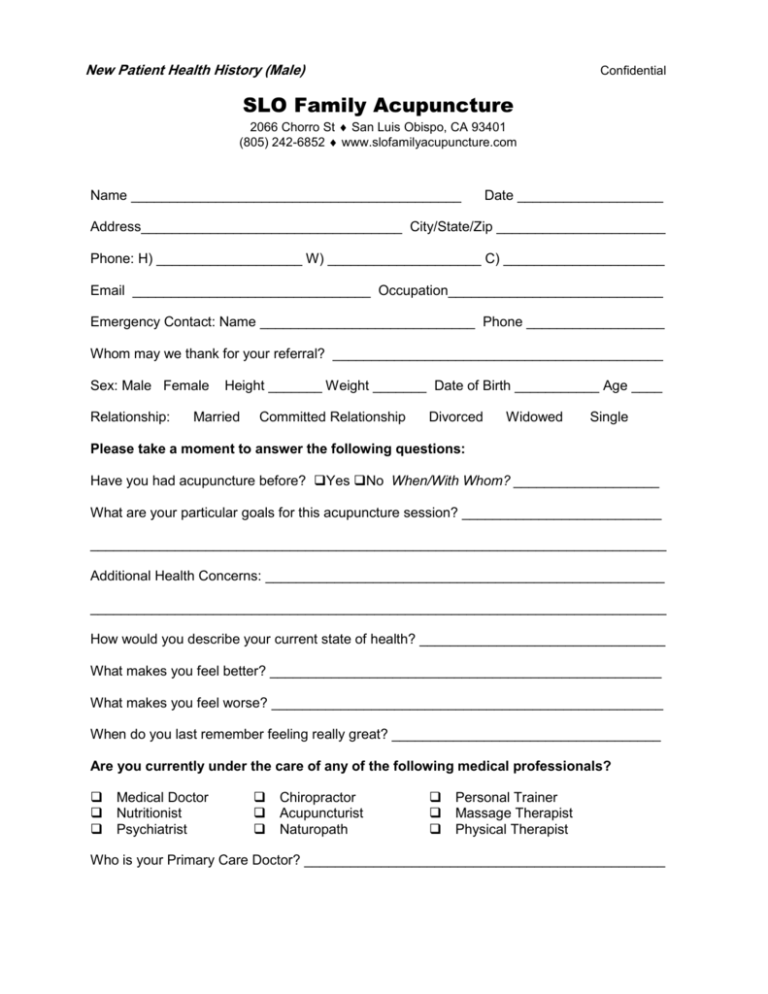
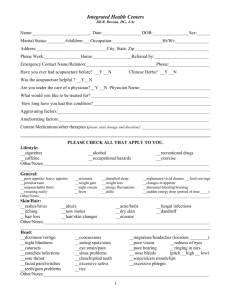
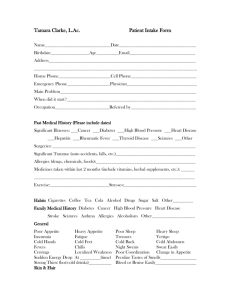
New Patient Health History (Male) Confidential SLO Family Acupuncture 2066 Chorro St San Luis Obispo, CA 93401 (805) 242-6852 www.slofamilyacupuncture.com Name ___________________________________________ Date ___________________ Address__________________________________ City/State/Zip ______________________ Phone: H) ___________________ W) ____________________ C) _____________________ Email _______________________________ Occupation____________________________ Emergency Contact: Name ____________________________ Phone __________________ Whom may we thank for your referral? ___________________________________________ Sex: Male Female Relationship: Height _______ Weight _______ Date of Birth ___________ Age ____ Married Committed Relationship Divorced Widowed Single Please take a moment to answer the following questions: Have you had acupuncture before? Yes No When/With Whom? ___________________ What are your particular goals for this acupuncture session? __________________________ ___________________________________________________________________________ Additional Health Concerns: ____________________________________________________ ___________________________________________________________________________ How would you describe your current state of health? ________________________________ What makes you feel better? ___________________________________________________ What makes you feel worse? ___________________________________________________ When do you last remember feeling really great? ___________________________________ Are you currently under the care of any of the following medical professionals? Medical Doctor Chiropractor Personal Trainer Nutritionist Acupuncturist Massage Therapist Psychiatrist Naturopath Physical Therapist Who is your Primary Care Doctor? _______________________________________________ New Patient Health History (Male) Confidential Please mark on the figures below where you are experiencing any discomfort, pain, or tension. Please check any that apply: Musculoskeletal System Arthritis Artificial Joints Bursitis Joint Pain Muscular Dystrophy Osteoporosis Plantar Fascitis Tendonitis Whiplash Carpal Tunnel Syndrome Digestive System Acid Reflux Diarrhea Constipation Ulcers Food Allergies Gall Stones Hepatitis Recent change in appetite Urinary System Frequent Urination Kidney Stones UTI Immune System Cancer Fibromyalgia Diabetes Edema HIV/AIDS Lupus Lymphoma Chronic Fatigue Syndrome Nervous System Alzheimer’s Headaches Migraines Multiple Sclerosis Parkinson’s Disease Seizures Sleep Disorders Shingles Spinal Cord Injury Respiratory System Asthma Allergies Bronchitis Sinusitis Frequent Cold/ Flu Integumentary System (Skin) Burns Dermatitis Eczema Fungal Infections Impetigo Scars Rash Circulatory System Atherosclerosis Thrombosis Heart Attack Stroke Varicose Veins Poor Circulation High Blood Pressure Low Blood Pressure Emotional System Depression Anxiety Grief Anger Other __________ New Patient Health History (Male) Confidential Date of last prostate check up ______________ PSA results _________________________ Manual prostate exam results __________ Lab results ______________________________ Frequency of urinations: daytime_______ nighttime_______ Pain with urination? ________ Color of urine: clear murky dark yellow other _____________ Any odor? __________ Please circle any that apply: Dribbling urination Retention of urine Decreased libido Impotence Premature ejaculation Testicular pain Delayed stream Incontinence Rectal dysfunction Back pain STD/STI’s: Syphilis Gonorrhea Other ______________________________ AIDS Herpes Chlamydia Date(s) ____________ Please list any accidents, surgeries, or hospitalizations (include approx date) ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ Please list any medications, vitamins, and herbs, with dosages, that you are currently taking and the reason why you are taking them: ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ Do you have any known allergies? ___________________________________________________________________________ ___________________________________________________________________________ ___________________________________________________________________________ Please indicate frequency of the following: Water ___________________ Coffee ________________ Soda ___________________ Tobacco __________________ Alcohol _________________ Drugs _________________ Exercise: Type ________________________ How often? ___________________________ Family History of Disease: Cancer Emotional Disorders Diabetes Other: ___________________________ Stroke Seizures Unknown Heart Disease High Blood Pressure Thank you for taking the time to complete this intake form. I look forward to working with you. –Carla Nerelli, L.Ac

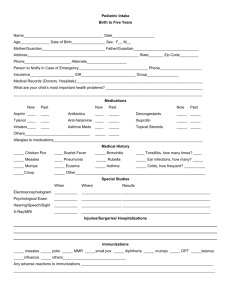
![Pediatric Health Histroy.Initial child.d[...]](http://s3.studylib.net/store/data/006593866_1-7ecae25d724665d2a564380f86b41e96-300x300.png)