Care plan
advertisement

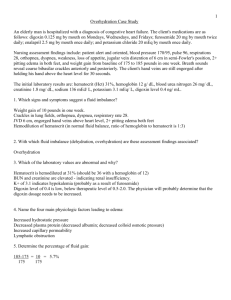
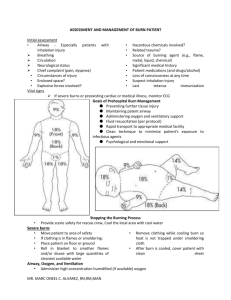
Anesthesia Care Plan Surgical Considerations Anticipated Procedure: Surgery Requirements: (positioning, surgeon requests, muscle relaxants, block placement, etc) Position: Anticipated Surgical Time: Estimated Blood Loss (EBL): Anesthesia Concerns: Preoperative Considerations Patient Data: Weight (kg): NPO Status: Allergies: Medical History: Anesthesia Concerns/Impact on plan: Ways to Maximize Patient Preoperatively: Lab Values: (Correcting electrolyte/glucose imbalances, nausea prophylaxis, albuterol, infuse blood/platelets, medical consultation, Chest x-ray, reschedule, etc) Anesthetic Technique General General/IV sedation MAC -Intravenous -Inhalational -Rapid Sequence (RSI) Regional PNB -spinal -epidural -caudal Local used: -type: -Bier Block Comments/Reasoning: Airway Management Equipment: Nasal Cannula Mask Size: Intubation Method Direct Laryngoscopy RSI/Modified RSI Awake/Asleep Fiberoptic Flexible/Rigid Bronchoscope Blind Intubation C-spine traction Comments: LMA Size: Blades Macintosh Miller Size: ETT Surgical Airway Size: -tracheostomy -oral/nasal -cricothyrotomy -cuffed/uncuffed -RAE, laser -double lumen, uninvent Ventilation Hand Ventilate Spontaneous/Assisted Machine: VCV or PCV -Tidal Volume: RR: Jet Ventilation Apneic oxygenation PIP: PEEP: Fluid Considerations Intravenous Line(s): -place IV/no IV -place IV: pre-op/intra-op -Location: -size: -number of IVs: IV Line Details: -10 or 60 drops/min -Buretrol -Extension tubing -T-connectors -extra stopcocks Fluid Options: -LR/NS -Hespan -Albumin -PRBC (donor/autologous) -platelets -FFP -other: Administration: (standard, pressure bag, rapid transfuser, etc) Comments: Calculating Fluid Requirements: Hourly Fluid Requirements: (4-2-1 rule: 4ml/kg for first 10 kg, 2ml/kg for next 10kg, and 1 ml/kg for remainder) Fluid Deficit: (NPO hours x hourly requirement): (Replace half of deficit in first hour, divide rest into second and third hour) Third Spacing: -minimal surgery -moderate tissue trauma -extreme tissue trauma 3-4 ml/kg/hr 5-6 ml/kg/hr 7-8 ml/kg/hr Insensible Loss: (generally 2ml/kg/hr, add for urine excretion and bowel prep) Replacement of Blood Loss: (replace with crystalloid 3:1, or 1:1 for blood or colloids) Fluid Replacement Schedule: 1st hour Deficit Maintenance 3rd Space Insensible Blood Loss Replacement TOTAL 2nd hour 3rd hour 4th hour Blood Loss Concerns Calculate Estimated Blood Volume (EBV): Neonate (1-30 days old) 90 ml/kg Infant (1 month to 1 year) 85 ml/kg Child (1 year to puberty) 80 ml/kg Male Adult 70-75 ml/kg Female Adult 60-65 ml/kg Calculate Maximum Allowable Blood Loss (ABL): Max ABL=EBV x (Hcti -Hctl)/Hcta Hcti=starting Hematocrit Hctl=lowest allowable Hematocrit Hcta=average hematocrit (Hcti + Hctl)/2 Monitors and Equipment Standard Monitors: Pulse oximeter, NIBP, Capnograph, EKG, (3 or 5 lead), FIO2 monitor, nerve stimulator, precordial/esophageal stethoscope Additional Monitors: Arterial Line, central line, pulmonary artery line, foley, BIS monitor, ICP monitor, Doppler, EEG, evoked potentials Additional Equipment: Bair Hugger (upper, lower, full body), fluid warmer, infusion pump, oral/nasal gastric tube, axillary rolls, cushioning, padding, tourniquet Comments: Possible Pharmacological Intervention (Nitroglycerin, beta-blocker, insulin, albuterol) Anesthetic Agents Premedication: Agent: Versed (IV, oral, nasal) Glycopyrrolate Fentanyl Zantac/Reglan Albuterol Other (ABx): Dose Range: Explain technique/reasoning: Spinal/Epidural/Caudal/Peripheral Nerve Block/Bier Block Drugs: Techniques: Dosing Strategy: Comments: Induction: Pre-oxygenation Technique: Airway Management Strategy: Drugs with doses: Maintenance: Gases: Drugs: Emergence: Emergence/Extubation Technique: Drugs with doses: (reversal) Post-operative Transport/Care: PACU vs ICU, oxygen, drugs (If transporting to ICU, what will you need for the transport?) Comments: