MIRA5004 Obstetric Sonography * Case Study 2: Third Trimester
advertisement

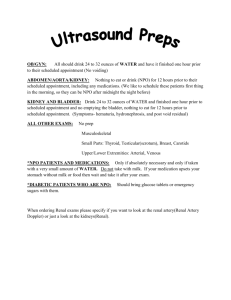
Vascular Sonography and Advanced Doppler Case Study Neil McLean 12025927 Case Study: Renal Duplex Fibromuscular Dysplasia Vascular Sonography and Advanced Doppler Case Study Background The patient is an 86 year old female with known fibromuscular dysplasia (FMD), presenting to our department 23/07/2015 for a renal duplex scan. The patient was not able to specifically name the disorder as it was only discovered recently, but was aware enough of the implications of the disease and the need for the ultrasound. Referral The referral clinical details simply stated FMD. The patient added that she had had a scan elsewhere and was now seeing a cardiologist who would like the scan findings confirmed before proceeding with further investigation or medication changes. The patient had a carotid Doppler scan the previous week looking for evidence of FMD. Those scan results were as follows: It was then presumed that the normal carotid may have prompted the referring doctor to investigate the veracity of the diagnosis of FMD and send the patient to us for another renal scan. Clinical assessment On initial sighting the patient was relaxed and comfortable. She exhibited no signs of peripheral vascular disease – no pain / claudication that couldn’t be equally explained by musculoskeletal complaints (she had arthritis). As far as she was aware the patient did not suffer hypertension but was unable to recall which medications she was on at the time. Her family history of vascular issues included only cardiovascular disease (her father died of a heart attack). Mobility was slightly limited by age but she was able to turn on the patient exam bed when needed and tolerated the scan well. Clinical Discussion – Fibromuscular Dysplasia History FMD is non atherosclerotic non inflammatory disease that has most recently been confirmed by an American Heart Association consensus statement as being of unknown pathogenesis. First described in a clinical case in 1938, FMD wasn’t classified pathologically until 1958 demonstrated angiographically until 1961. Prevalence The prevalence of the disease is disputed and not very well understood. Based on an American registry of FMD diagnosed individuals that women are more strongly represented (9:1). FMD usually affects renal (58% of cases) and cerebral (32% of cases) vessels though case reports have identified that any arterial bed can be involved (Olin et al. 2014). Signs Vascular Sonography and Advanced Doppler Case Study Renal FMD patients can be asymptomatic or present with signs including hypertension, abdominal bruit, abdominal angina, renal artery aneurysm or dissection (Poloskey et al. 2012). Classification of sub-types Histologic Classification of FMD by the layers of the vessel walls involved: Intimal (second most common - 1 – 5% of cases (Sperati et al. 2009) wide variety of appearances) Medial Peri-adventitial Medial FMD is further classified into separate histology types (Olin et al. 2014): Medial fibroplasia (>90% of all cases ‘string of beads’ appearance) Peri-medial fibroplasia (<1% of all cases) Medial hyperplasia (<1% of all cases, usually presents with uniform, smooth stenosis) Figure 1 - Histologic specimen taken from an FMD affected artery showing the proliferation of connective tissue forming a ridge intruding on the lumen. (Image from Olin et al 2014) Radiologic An alternate classification system was devised by a French and Belgian expert panel (Persu et al. 2012). The reasoning was that FMD is almost purely a radiological diagnosis and the classification by histology is obsolete. Their system divides the appearances of FMD into: Multi-focal (medial FMD string of beads lesions) Uni-focal (stenotic lesions <1cm long) Tubular (stenotic lesions >1cm long) Differential diagnoses (Sperati et al. 2009) Atherosclerosis Vasculitis (FMD is non inflammatory and can be differentiated by haematology analysis – no signs of anaemia, raised ESR or CRP) Renal artery dissection Neurofibromatosis Vascular Sonography and Advanced Doppler Case Study Ehlers-Danlos’ syndrome Marfan’s Syndrome Alport’s syndrome Alpha 1 anti-trypsin deficiency Diagnostic imaging Angiography gold standard Duplex ultrasound – 98% sensitive and specific (Mousa and Gill 2013) Intra-vascular ultrasound – compares well with angiography, but is invasive and generally reserved for intra-operative scenarios i.e. stent repair CTA – radiation involved and does not compare as well to angiography as other modalities MRA – compares well with angiography – sensitivity 97%, specificity 93% (Sperati et al. 2009) Figure 2 - Angiography of renal artery FMD showing mid to distal segment 'string of beads' appearance typical of the medial fibroplastic form of the disease. (Image taken from Mousa and Gill 2013) Sonographic appearances The alternating constrictions and dilatations of connective tissue create a ‘string of beads’ appearance on angiography that is also visible under colour Doppler ultrasound. (Olin et al. 2014) notes that the alternating dialtations are usually larger in caliber than the normal vessel and that the string of beads usually occur in the mid to distal section of the artery. (Mousa and Gill 2013) detail sonographic findings further: Raised peak systolic velocity suggestive of stenosis Aliasing of colour flow imaging through stenotic region Size difference between kidneys due to renal insufficiency Renal aortic ratio above 3.5 Equipment Selection The examination was conducted using a GE LOGIQ E9 ultrasound scanner and a curved C1-6 MHz. the renal artery protocol was selected. This protocol initialises the scan with reduced dynamic range, line density and field of view compared to the abdominal setting. The reasoning behind these changes is to improve frame rate and visualisation of the normally small calibre vessels. Vascular Sonography and Advanced Doppler Case Study Scanning Images This was one of the first renal artery scans I performed and some close supervision was provided during this scan. The patient was compliant so I was able to complete the scan with my supervisor close by to help with some of the rapid fire knob twiddling required in a duplex renal scan. Starting with the baseline aorta trace I took a representative measurement of the aortic calibre to show it was prominent. Although initially destroyed by some breathing motion, the aortic trace came clear and demonstrated normal velocity. I identified the left renal artery coming off the aorta and took the first two traces and a colour picture representing it. These images were achieved with the patient supine, scanning through the anterior abdominal wall and compressed stomach. We turned the patient to left decubitus to continue the analysis of the mid and distal portion of the left renal artery: Vascular Sonography and Advanced Doppler Case Study Unlike other left renal arteries I have scanned since this lady, her LRA was reasonably straight and uncomplicated to get velocity traces from. I then performed a scan through the left kidney, identifying two para pelvic cysts: I completed the left side with a representative intra-renal artery trace: Vascular Sonography and Advanced Doppler Case Study Rolling the patient back to supine and then propping up with a pad under her back for an RAO position, I put the probe on and noticed something awry with the right renal artery immediately: Fortunately I realised that the PRF was set way too low from the intra-renal artery trace and reset it, discovering an interesting appearance in the process: This looked like the textbook example of FMD that my colleague and I looked up before starting the scan. Aliasing was evident, as was the expected ‘lumpy’ appearance of the string of beads sign. The resulting traces of the right renal artery started well enough at the origin but quickly took a turn through the area of the stenosis: Vascular Sonography and Advanced Doppler Case Study The maximum velocity jet found at the distal end of the lesion was over 300 cm/s. This equated to a renal aortic ratio of 5.3! The post stenotic artery bifurcated before entering the renal hilum so I took a trace of each: The post stenotic waveforms demonstrated expected changes: the upper artery bifurcation was dampened with a very broad spectral peak and low end diastolic velocity compared to the normal segment at the origin. The lower artery had a more normal velocity profile but the waveform was jagged with turbulent flow. I ended the study after taking representative images of the right kidney and an intra-renal waveform: Vascular Sonography and Advanced Doppler Case Study In retrospect I would like to have taken a trace from an intra-renal artery in the upper pole to demonstrate any evidence of insufficiency in the segment of the kidney supplied by the tardus parvus flow of the upper RRA bifurcation. It would also have been nice to adjust the calipers in the image above so that the correct acceleration time and resistivity index were displayed. Findings The right renal artery displayed a region of stenosis in keeping with the appearances of medial fibroplasia type FMD. The vessel had alternating areas of constriction and dilatation under B-mode, aliasing of colour flow through the stenotic region and increased peak systolic velocity consistent with a 60 – 69% stenosis. Patient Management and Communication My explanation of the procedure to the patient involved the following points: Warm ultrasound gel on abdomen Colours on screen and whooshing noises from speakers indicate blood flow Firm pressure required with the transducer (‘let me know if I am pushing too hard’) There will be some rolling around on the table required Asking the patient for ID details and checking the referring doctor report delivery method Any concerns or questions – let me know The patient tolerated the scan incredibly well for her age. My initial grasp of renal artery traces involved having patients suspend respiration but at the insistence of my senior colleague I let the patient continue quiet respiration throughout the scan. Although certain traces were a little short on my normal criteria of the number of cycles displayed, I immediately saw the benefits. The patient was more comfortable, suspended respiration may have been counterproductive once the patient became fatigued and it taught me to be quicker with the probe and also try to anticipate when the best time to capture the trace would be. Once we had finished the scan we showed the images to a radiologist. We then returned to the patient and ensured we had the correct contact details for their referring specialist and also their GP. Vascular Sonography and Advanced Doppler Case Study References Mousa, Albeir Y., and Gurpreet Gill. 2013. "Renal fibromuscular dysplasia." Seminars in Vascular Surgery 26 (4):213-218. doi: http://dx.doi.org/10.1053/j.semvascsurg.2014.06.006. Olin, Jeffrey W., Heather L. Gornik, J. Michael Bacharach, Jose Biller, Lawrence J. Fine, Bruce H. Gray, William A. Gray, Rishi Gupta, Naomi M. Hamburg, Barry T. Katzen, Robert A. Lookstein, Alan B. Lumsden, Jane W. Newburger, Tatjana Rundek, C. John Sperati, and James C. Stanley. 2014. "Fibromuscular Dysplasia: State of the Science and Critical Unanswered Questions: A Scientific Statement From the American Heart Association." Circulation 129 (9):1048-1078. doi: 10.1161/01.cir.0000442577.96802.8c. Persu, Alexandre, Emmanuel Touzé, Elie Mousseaux, Xavier Barral, Francis Joffre, and Pierre-François Plouin. 2012. "Diagnosis and management of fibromuscular dysplasia: an expert consensus." European Journal of Clinical Investigation 42 (3):338-347. doi: 10.1111/j.13652362.2011.02577.x. Poloskey, Stacey L., Jeffrey W. Olin, Pamela Mace, and Heather L. Gornik. 2012. "Fibromuscular Dysplasia." Circulation 125 (18):e636-e639. doi: 10.1161/circulationaha.111.090449. Sperati, C. John, Nisha Aggarwal, Aravind Arepally, and Mohamed G. Atta. 2009. "Fibromuscular dysplasia." Kidney International 75 (3):333-6. doi: http://dx.doi.org/10.1038/ki.2008.232.