Hospital Consultants and the Consultants Contract August 2013
advertisement
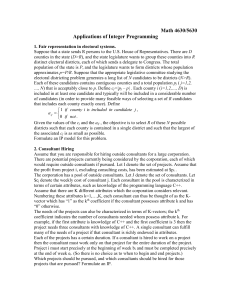
Hospital Consultants and the Consultants Contract August 2013 Note: This paper is intended as background information for the media. It is not intended as a comprehensive BMA policy paper What is a consultant? A consultant is the most senior grade of doctor working in a hospital. They are highly trained and skilled with vast expertise gained through a lengthy and extensive training programme. As the most senior specialist doctors in the hospital they have the ultimate responsibility for the care of patients referred to them. In addition to their clinical work in treating and caring for patients, they also take the lead role in developing services for patients, supervise and train other doctors, undertake research to improve treatments, and oversee the running of clinical services. Their workload is often very high, intensely demanding and exceedingly complex. How you become a consultant It usually takes around 12 years to become a consultant. Most doctors begin their medical training at medical school where they spend five years as an undergraduate at university. This is then followed by two years of general training in hospital on a Foundation Programme during which time they will be known as foundation doctors. Foundation training is made up of F1 (foundation year one) and F2 (foundation year 2). After this point, a doctor’s training will vary depending on their chosen specialty of medicine and career path. To become a consultant, a doctor must then begin a specialty training programme. These usually take between five and seven years to complete. For more information on the training of doctors visit http://www.nhscareers.nhs.uk/ The consultant contract (England) The current NHS contract was implemented in 2003. There are separate contracts for the four UK nations, negotiated separately in the four nations. Pay Scale Consultants earn a basic salary which currently runs from £75,249 to £101,451. Pay freezes and sub-inflationary annual increases have been in place in recent years which have limited salary levels. Progression up the scale depends on satisfactory completion of duties, based on an annual job planning process. For the first four years of service as a consultant, progression takes place annually, but after that every five years. Typically doctors reach the top of the scale only after around 20 years of service as a consultant (or around 35 or 36 years after entering medical school.) The basic salary is based on a job plan of programmed activities (PAs). This is usually based on a 10 PA week of 40 hours, but some consultants can be contracted to work more than this. Clinical Excellence Awards (CEAs) Clinical Excellence Awards (CEAs) are intended to recognise and reward those consultants who contribute the highest levels of medical service. Any NHS consultant in England can apply for a CEA (separate schemes exist for consultants in Wales, Northern Ireland and Scotland). The Advisory Committee on Clinical Excellence Awards (ACCEA) is the body that administers CEAs. It states that they are given to “recognise and reward NHS consultants and academic GPs who perform “over and above” “the standard expected of their role.” To be considered for an award applicants “have to demonstrate achievements in developing and delivering high quality patient care, and commitment to the continuous improvement of the NHS.” This could mean delivering a high quality service, performing a leadership role, enhancing clinical quality or cost-effectiveness, making a personal contribution to a national or international health policy development, or taking forward medical research. There are two kinds of CEAs, both of which are paid as additional salary. National level CEAs (funded centrally from the overall ‘pot’ for consultant pay) reward consultants for their contribution at a national level, and are managed by ACCEA. Employer-based awards are maintained and funded by consultants’ employer / Trust. The current award rates are published at: bma.org.uk/practical-support-at-work/pay-fees-allowances/pay-scalesconsultants Other pay supplements On call work: Consultants who are available on call at night or at the weekend for emergencies out of hours receive a supplement which varies from 1% of basic salary for those working a low number of on call shifts to 8% of basic salary to those working a high number. Additional non-emergency work: Consultants are typically paid at time and a third for additional work required at weekends and, in England, all work before 7am or after 7pm on weekdays, that falls outside of their contracted hours. Consultants may also be approached for additional ad hoc work for their trust, but there are no nationally agreed rates of pay for such work in England, and remuneration is locally negotiated. Managerial Responsibilities: Many consultants also hold managerial positions, for example as Clinical Directors of hospital trusts. Medical management positions are often classified and remunerated separately to the consultant contract through a “responsibility payment”. Myths surrounding the contract and consultants’ pay MYTH: Consultant pay progression is automatic and is not linked to performance and Clinical Excellence Awards, designed to award consultants for “exceptional” performance are the “norm rather than the exception.” FACT: Consultants must meet agreed objectives and a number of other criteria to qualify for pay progression. The latest figures show that around four in 10 consultants currently don’t receive a CEA, with just 1% receiving the highest reward http://tinyurl.com/p276ze8 MYTH: Clinical Excellence Awards are not regularly reviewed to make sure that individual awards are still warranted and are value for money FACT: Yes, they are - all national awards are reviewed and the top level of local awards is also reviewed. MYTH: The significant increase in consultant pay resulting from the change in contract did not improve productivity. FACT: Crude productivity statistics do not reflect the way a consultant works. Productivity is very difficult to measure and does not show the quality of patient care. Doctors do not treat patients like factories churning out widgets and patients do not want to feel like they are being pushed through a machine. Some procedures are more complicated or the patient may have other risk factors which will affect the length of an operation. A surgeon may have trainee doctors working alongside which can also alter the length of procedures. There may be administrative or system delays in getting the patients into theatre on time. Research shows that there is no relationship between levels of productivity and when the consultant contract was changed. The contract, when implemented properly, has facilitated better team working to improve continuity of care, changed working patterns to improve efficiency, and allowed a greater presence of consultants on wards at key times and optimised the best use of theatre time. These benefits are not easy to measure using crude statistics. They can also be difficult to achieve when the NHS is forced to cut back on activity or on recruitment in order to save money. A National Audit Office report published in February 2013 showed that there was an improvement in productivity levels compared to those before the 2003 contract http://tinyurl.com/p3o97hr MYTH: The contract does not facilitate the provision of around-the-clock care and trusts continue to pay too much to secure work above contracted levels FACT: The contract ensures that there is an agreed arrangement for 24/7 on-call working and other provisions, such as dealing with emergencies. However it was not designed to facilitate routine work in the evenings or at weekends. Providing such a service would need considerable planning and resourcing. The NHS is already struggling to provide high quality care in the current difficult economic climate during the normal working day and considerable investment would be needed if NHS services were to be expanded. Ensuring that patients have high quality, round-the-clock access to urgent and emergency care must be our priority and many doctors already work throughout the night to provide this. But we also need to think about how these services are designed and provided, and crucially, how quality and safety can be assured. MYTH: Since the consultant contract was introduced in 2003, consultant pay has increased by 2428%. FACT: This is true. The contract was designed, in part, to recognise that consultant remuneration had fallen behind the pay levels that you would expect for a senior, highly qualified professional with significant responsibility. However the rise in salary has now been completely negated by recent pay cuts, freezes and other reductions to their earnings including the impact of less funding to clinical excellence awards and major changes to the NHS pension scheme.