Please find the schedule and abstracts for Saturday`s
advertisement
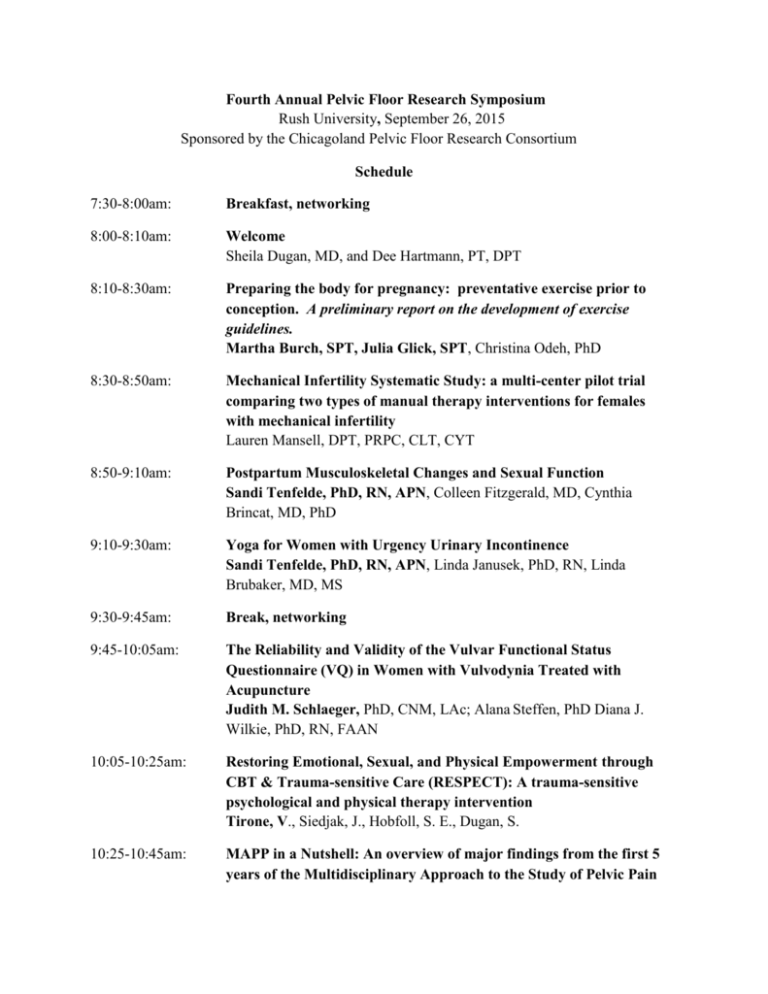
Fourth Annual Pelvic Floor Research Symposium Rush University, September 26, 2015 Sponsored by the Chicagoland Pelvic Floor Research Consortium Schedule 7:30-8:00am: Breakfast, networking 8:00-8:10am: Welcome Sheila Dugan, MD, and Dee Hartmann, PT, DPT 8:10-8:30am: Preparing the body for pregnancy: preventative exercise prior to conception. A preliminary report on the development of exercise guidelines. Martha Burch, SPT, Julia Glick, SPT, Christina Odeh, PhD 8:30-8:50am: Mechanical Infertility Systematic Study: a multi-center pilot trial comparing two types of manual therapy interventions for females with mechanical infertility Lauren Mansell, DPT, PRPC, CLT, CYT 8:50-9:10am: Postpartum Musculoskeletal Changes and Sexual Function Sandi Tenfelde, PhD, RN, APN, Colleen Fitzgerald, MD, Cynthia Brincat, MD, PhD 9:10-9:30am: Yoga for Women with Urgency Urinary Incontinence Sandi Tenfelde, PhD, RN, APN, Linda Janusek, PhD, RN, Linda Brubaker, MD, MS 9:30-9:45am: Break, networking 9:45-10:05am: The Reliability and Validity of the Vulvar Functional Status Questionnaire (VQ) in Women with Vulvodynia Treated with Acupuncture Judith M. Schlaeger, PhD, CNM, LAc; Alana Steffen, PhD Diana J. Wilkie, PhD, RN, FAAN 10:05-10:25am: Restoring Emotional, Sexual, and Physical Empowerment through CBT & Trauma-sensitive Care (RESPECT): A trauma-sensitive psychological and physical therapy intervention Tirone, V., Siedjak, J., Hobfoll, S. E., Dugan, S. 10:25-10:45am: MAPP in a Nutshell: An overview of major findings from the first 5 years of the Multidisciplinary Approach to the Study of Pelvic Pain (MAPP) Research Network Melissa A. Farmer, PhD 10:45-11:05am: Brain mechanisms of female urologic pelvic pain: Grant study proposal for critical discussion Melissa A. Farmer, PhD Preparing the body for pregnancy: preventative exercise prior to conception. A preliminary report on the development of exercise guidelines. Martha Burch, SPT, Julia Glick, SPT, Christina Odeh, PhD Introduction: More and more women are planning their pregnancies—they are told to take folic acid and eat healthy, but there are virtually no guidelines for exercise that can help prepare the body for pregnancy. The discussion of prenatal care needs to include and explore the importance of exercise prior to conception as a form of prevention for common musculoskeletal complications during pregnancy. Methods: A review of current literature was conducted to determine appropriate interventions for women to perform the year prior to conception. Researchers focused on the impact of exercise, both prior to and during pregnancy, on various conditions, including low back and pelvic pain and stress urinary incontinence. Results: Findings revealed a scarcity of research on women’s activity levels prior to pregnancy and the resulting complications during and post-pregnancy. In a PubMed search for “preconception care” 1951 articles were generated, but when physical activity or exercise were added ((preconception care and exercise)) OR (preconception care and physical activity) only 75 articles were generated. Conclusion: Due to the scarcity of research, recommendations of a pre-conception exercise protocol will be based on current knowledge of exercise interventions during pregnancy and sound biomechanical principles. Clinical Implications: Researchers have used the current literature of exercise and complications during pregnancy to develop a list of potential preventative exercises prior to pregnancy. Goal of presentation: Initiate discussion and raise awareness of prevalence and prevention of pregnancy-related complications while encouraging other researchers and clinicians to offer insight into this issue. Mechanical Infertility Systematic Study: a multi-center pilot trial comparing two types of manual therapy interventions for females with mechanical infertility Lauren Mansell, DPT, PRPC, CLT, CYT Introduction Infertility is defined by the CDC as the inability to conceive after one year of unprotected intercourse. Current treatments consist of hormone therapy, intra-uterine insemination and invitro insemination. These options are expensive, not necessarily covered by insurance, and carry different levels of short-term and long-term health risks such as multiple births and an increased rate of ovarian cancer. Many of the issues that contribute to infertility can be traced to scar tissue, fascial restriction, and lymphatic congestion in the pelvic region. These issues could make it difficult to conceive or continue a pregnancy. Just as each joint in the body has its range of motion, so do each of the organs. The uterus must respond to changes in position, the bladder filling, and food moving through the intestines. It is supported by ligaments and tension in those ligaments can alter the position and range of motion of the uterus. Manual therapy techniques exist to release fascial restrictions, to mobilize tight ligaments, and to drain congested lymphatics, all of which can be applied to the reproductive system. Aim The intent is to do a 30 subject pilot study as a model to assess the feasibility of a multi-center, nation-wide study with a goal to treat women using these theories and techniques published in 2012. The data will be used for a power analysis, attrition rates, and to assess any need for changes within the protocol. All women will need to be tested prior to participating as well as their partners to ensure there are no issues, such as fully blocked tubes or low sperm count that would exclude them from the study. Women will be randomly placed into either the physical therapy group or a massage therapy group. The physical therapy group will receive hands on treatment based on a protocol that addresses whichever physical issues are found on evaluation. The massage therapy group will receive general therapeutic massage. Once treatment has been completed, women will be called monthly for three full cycles to determine pregnancy status and, if pregnant, again after the due date to determine if the length of pregnancy. Upon completion of the study, those in the massage group will be offered the physical therapy treatments. Main Outcome Measures Pregnancy SF-36 Methods Manual Therapy Protocol to include: Muscle Energy, Positional Release, Arterial Release, Lyphmphatic Drainage, Visceral Mobilization Massage Group to include effleurage/petrissage globally excluding abdomen Result and Conclusion (Study just received IRB approval 8/17/15) TBA Postpartum Musculoskeletal Changes and Sexual Function Sandi Tenfelde, PhD, RN, APN, Colleen Fitzgerald, MD, Cynthia Brincat, MD, PhD Introduction: Many women experience postpartum musculoskeletal pelvic pain, significantly impacting their quality of life. Pelvic pain can be localized internally as pelvic floor myofascial pain or externally in pelvic girdle pain (PGP). Despite the high number of women affected by musculoskeletal pelvic pain after childbirth, the exact pathoanatomic etiologies remain unknown. The relationship between postpartum musculoskeletal pelvic pain and sexual function also is understudied. The majority of sexually active postpartum women report some form of sexual dysfunction with current research focusing on dyspareunia related to perineal trauma. Research in musculoskeletal pelvic pain after childbirth has generally been limited to populations outside of the United States and few studies have used validated measures with physical exam findings Aims: The specific AIMS are to 1) determine the extent internal myofascial pain is associated with sexual function and 2) determine the extent to which external pelvic girdle pain (PGP) is associated with sexual function. Main Outcome Measures: Female Sexual Function Index, vaginal assessment of pelvic floor muscle function (e.g. modified Oxford), musculoskeletal exams (e.g. P4 provocation, Patrick Faber’s). Methods: 100 women who have given birth within the last 12 months are being recruited to participate in a descriptive cross sectional study. Women complete questionnaires on demographic, general health, and pregnancy related data. A focused physical exam is also completed at the time of the study visit. Results: The study is ongoing. Preliminary data will be presented. (20 out of 100 total women have been recruited). Conclusion: Our long-term goal is to improve the quality of sexual function for women with postpartum musculoskeletal pelvic pain. Our central hypothesis is that women with musculoskeletal pelvic pain after childbirth will have more sexual dysfunction than women without musculoskeletal pelvic pain. Yoga for Women with Urgency Urinary Incontinence Sandi Tenfelde, PhD, RN, APN, Mentors: Linda Janusek, PhD, RN, Linda Brubaker, MD, MS Introduction: Women with urgency urinary incontinence (UUI) have considerable symptom burden resulting in psychological morbidity, impaired relationships, social isolation, and poor quality of life. Pharmacologic treatments for UUI have multiple adverse effects with decreasing efficacy in the long term, reducing the willingness of women to treat their symptoms with medications. Furthermore, new evidence indicates UUI symptoms are associated with elevated urinary proinflammatory cytokines, resulting in an imbalance of parasympathetic and sensory innervations of the bladder. Yoga, a popular mind-body therapy, may serve to benefit women with UUI by reducing UI symptom distress, perception of severity and impact on daily living. Increasing research demonstrates that the practice of yoga results in positive psycho-physiologic effects beneficial to health. AIM: The specific aims are to: (1) Determine the extent to which a yoga program reduces UUI symptoms (distress, severity, and impact on daily living) and (2) Evaluate associations among psychological stress, proinflammatory cytokines, sympatho-vagal balance and UUI symptoms in women completing a yoga program compared to control women. Main Outcome Measures: UDI-6, IL-6, CRP, heart rate variability monitoring Methods: This pilot study is using a psychoneuroimmunology (PNI) framework to advance understanding of symptom distress and to evaluate a self-care approach (yoga) for women to manage symptoms associated with UUI. Sample size is 40 women. 8 women with UUI symptoms have participated in an 8 week, twice weekly yoga program. Results: The study is ongoing. Preliminary data will be presented. (8 out of 40) Relevance: The evidence generated from this patient-oriented study will provide preliminary data to support the submission of a larger grant with a sample size that has sufficient power. The goal of this research is to challenge current UUI treatment paradigms and to equip women with UUI symptoms with an acceptable and cost-effective approach to self-manage their symptoms; empowering them to live active, normal lives. The Reliability and Validity of the Vulvar Functional Status Questionnaire (VQ) in Women with Vulvodynia Treated with Acupuncture 1Judith M. Schlaeger, PhD, CNM, LAc; 2Alana Steffen, PhD 3Diana J. Wilkie, PhD, RN, FAAN 1University of Illinois at Chicago College of Nursing Department of Women, Children and Family Health Science, Chicago, IL 2University of Illinois, Chicago College of Nursing Office of Research Facilitation, Chicago, 3University of Florida College of Nursing Department of Biobehavioral Nursing Science, Gainesville, FL Purpose: The measurement of the physical dimensions of vulvodynia with the VQ was tested only once on a sample of 60 women before and after physical therapy. Our purpose was to examine indicators of reliability and sensitivity of the VQ in an acupuncture study for treatment of vulvodynia. Theoretical Framework and Methods: This methodologic study focused on the psychometrics of the VQ in a 5-week study of 36 women (mean age 35.0 (7.6 SD), 34 white non-Latino and 2 African Americans) randomized to an acupuncture treatment group (n=18) or a wait-list control group (n=18). We evaluated test-retest reliability in the control group and internal consistency in the entire sample (intraclass correlation, ICC). Change scores were compared between groups using independent t-test to determine sensitivity to intervention effects in the sample, which was previously shown to differ on vulvar pain, dyspareunia, and overall sexual function. Results: Test-retest reliability was 0.88, showing stability over 5 weeks. Cronbach’s alpha was 0.72. The mean (SD) change scores for the acupuncture group was 0.72 (2.59) and for the waitlist control group was 2.67 (2.38), which was statistically significant (t(df=34)=2.35, p< .025). Conclusion: There was adequate test-retest reliability and internal consistency of the VQ. The construct validity of the VQ was supported by its sensitivity to the intervention effect. The VQ may be useful as a measure of functional status in women with vulvodynia in future acupuncture intervention studies. Restoring Emotional, Sexual, and Physical Empowerment through CBT & Traumasensitive Care (RESPECT): A trauma-sensitive psychological and physical therapy intervention Tirone, V., Siedjak, J., Hobfoll, S. E., Dugan, S. Background. Chronic Pelvic Pain (CPP) is comorbid with dyspareunia, depression, anxiety, relationship distress, functional impairment and poor quality of life (Roth, Punch, & Bachman, 2011). Sexual abuse is a type of trauma that is associated with development of CPP (Chandler, Ciccone, & Raphael, 2006) and the severity of comorbid concerns (Leclerc, Bergeron, Binik, & Khalife, 2009; Powers, et al., 2014). Frontline CPP treatments such as physical therapy and painspecific psychological interventions often fail to address sexual abuse. The invasive techniques utilized in physical therapy have the potential to trigger trauma-related symptoms. Neglecting sexual abuse in CPP treatment could contribute to poor treatment outcomes such as symptom persistence, low adherence, and attrition. Trauma-sensitive care, in which medical providers modify their delivery of interventions to facilitate recovery from trauma-related symptoms, may prevent poor treatment outcomes in this population. This project will develop and examine Restoring Emotional, Sexual, and Physical Empowerment through Cognitive Behavioral Therapy & Trauma-sensitive Care (RESPECT), a trauma-sensitive psychological and physical therapy intervention. Design. This open pilot trial will examine the following questions: Question 1. Is REPECT feasible and acceptable among physical therapy providers? Hypothesis 1. Training will develop physical therapists’ trauma-sensitive care knowledge and increase their comfort in treating abuse survivors. Question 2. Is RESPECT acceptable among patients? Hypothesis 2. Patients will adhere to the RESPECT protocol and will report expected benefit from and satisfaction with the intervention. Question 3. Does RESPECT impact CPP and comorbid concerns? Hypothesis 3. Patients’ CPP and comorbid concerns will be reduced following RESPECT. Method. Self-report measures will be used to assess providers’ use of trauma-sensitive behaviors and acceptability. RESPECT’s acceptability among patients and treatment outcomes (i.e., pain, sexual functioning, depression, and posttraumatic stress disorder) will be assessed using selfreport measures. Patients’ adherence will be measured using attendance at psychotherapy and physical therapy sessions. MAPP in a Nutshell: An overview of major findings from the first 5 years of the Multidisciplinary Approach to the Study of Pelvic Pain (MAPP) Research Network Melissa A. Farmer, PhD Department of Physiology, Northwestern University, Chicago IL The MAPP Research Network is the first multi-center research consortium to focus on urologic chronic pelvic pain syndrome (UCPPS), a research term that encompasses chronic prostatitis/chronic pelvic pain syndrome (CP/UCPPS) and bladder pain syndrome/interstitial cystitis (PBS/IC). Six universities including Northwestern University, University of California at Los Angeles, University of Southern California, Stanford University, University of Michigan, and University of Iowa gathered observational epidemiological, inflammatory biomarker, and neuroimaging data in over 400 men and women with UCPPS, in comparison with age-matched positive controls (irritable bowel syndrome, fibromyalgia, chronic fatigue syndrome, and their comorbidities) and healthy controls. Over the past year, the publications from the first 5 years of MAPP have generated the first empirical descriptions of UCPPS sex differences, pain flares, putative clinical subtypes based on pain with bladder filling, and brain imaging data suggesting that regional brain anatomy and its function changes in proportion to UCPPS symptom severity. This talk will highlight the major findings of these efforts, with a particular focus on potential mechanisms of UCPPS and their assessment, clinical markers of future symptom improvement, and potential treatment strategies to address peripheral and central nervous system changes thought to maintain urologic pelvic pain. Brain mechanisms of female urologic pelvic pain: Grant study proposal for critical discussion Melissa A. Farmer, PhD Department of Physiology, Northwestern University, Chicago IL Female urologic chronic pelvic pain syndrome (UCPPS) exacts a heavy psychological, societal, and healthcare burden. Recent ebrain imaging results have revealed functional and structural brain abnormalities related to pain and urinary symptom severity in women with bladder pain syndrome/interstitial cystitis (BPS/IC), including altered: 1) resting state activity (reflecting taskfree information transmission within the brain), 2) gray matter (neuronal) density and volume, and 3) white matter (axonal microstructure). These results establish that regional brain alterations related to ongoing symptom severity are core elements of the UCPPS disease profile. In the first description of white matter abnormalities in women with BPS/IC (Farmer et al., 2015), increased axonal integrity in a brain region that mediates pelvic floor muscle fine motor movements was correlated with pain and urinary dysfunction. This finding suggests that UCPPS severity is related to pelvic floor motor learning of postural changes. The nature of this hypothesized motor learning is unclear, and its relationship with other brain structures may provide a trail of evidence that can be leveraged to understand UCPPS mechanisms. Provision of pelvic floor physical therapy may directly influence the type/extent of motor learning related to UCPPS symptoms and can be experimentally manipulated to determine the correspondence between altered brain structure of pelvic floor motor learning. The presentation will focus on rationale behind this pelvic floor motor learning hypothesis, supporting evidence, critical discussion of how motor learning can be objectively assessed, and the potential impact of comorbid pelvic pain. Mechanical Infertility Systematic Study: a multi-center pilot trial comparing two types of manual therapy interventions for females with mechanical infertility All investigators except Dr. Sreedevi are pelvic physical therapists who have undergone training in the techniques used in the protocol as well as training in the protocol itself. Training included: Visceral Mobilization of the Urological System (17.75 hours), Visceral Mobilization of the Reproductive System (17.75 hours) and Lymph Drainage for the Pelvic PT (15 hours). Hand skills of each practitioner were evaluated for accuracy of palpation skills and ability to perform techniques correctly. Therapists with inadequate skills were not invited to participate in the study. All research staff have completed CITI training for conducting research involving human subjects. Dr. Sreedevi specializes in obstetrics and gynecology and is a member of the American College of Obstetrics and Gynecology. She will be available to consult with the therapists on subject inclusion or exclusion, and on questions that may arise during the course of treatment. Infertility is defined by the CDC as the inability to conceive after one year of unprotected intercourse. Current treatments consist of hormone therapy, intra-uterine insemination and invitro insemination. These options are expensive, not necessarily covered by insurance, and carry different levels of short-term and long-term health risks such as multiple births and an increased rate of ovarian cancer. Many of the issues that contribute to infertility can be traced to scar tissue, fascial restriction, and lymphatic congestion in the pelvic region. These issues could make it difficult to conceive or continue a pregnancy. Just as each joint in the body has its range of motion, so do each of the organs. The uterus must respond to changes in position, the bladder filling, and food moving through the intestines. It is supported by ligaments and tension in those ligaments can alter the position and range of motion of the uterus. Manual therapy techniques exist to release fascial restrictions, to mobilize tight ligaments, and to drain congested lymphatics, all of which can be applied to the reproductive system. A case series report was published in 2012 which employed these techniques to treat infertility. After receiving an average of 3.5 visits, 6 out of 10 of the women treated were able to conceive within three months after finishing treatments. All six of the women gave birth to healthy babies. The intent is to do a 30 subject pilot study as a model to assess the feasibility of a multi-center, nation-wide study with a goal to treat women using these theories and techniquest published in 2012. The data will be used for a power analysis, attrition rates, and to assess any need for changes within the protocol. All women will need to be tested prior to participating as well as their partners to ensure there are no issues, such as fully blocked tubes or low sperm count that would exclude them from the study. Women will be randomly placed into either the physical therapy group or a massage therapy group. The physical therapy group will receive hands on treatment based on a protocol that addresses whichever physical issues are found on evaluation. The massage therapy group will receive general therapeutic massage. Once treatment has been completed, women will be called monthly for three full cycles to determine pregnancy status and, if pregnant, again after the due date to determine if the length of pregnancy. Upon completion of the study, those in the massage group will be offered the physical therapy treatments. Physical therapy has already been shown to be effective in the treatment of pelvic pain and bladder dysfunction, and its role in women’s health can expand further. If this study is able to show that physical therapy is an effective method of treatment for infertility, the paradigm for treating infertility could shift. Just as PT is a first line of treatment for low back pain prior to surgery, PT could become the first line treatment for infertility. Infertility treatment could potentially become much more affordable and be attainable to a much larger segment of the population with fewer risks to women’s health. There will be two therapy groups: a physical therapy group and a massage therapy group. Both groups will receive six treatment sessions, lasting one hour each. All treatments will be performed by site investigators at the listed research sites. Each group will receive treatments once per week for the first month (four treatments), after which subjects will receive one treatment per month for the next two months. At the initial treatment session, subjects will fill out an SF-36, questionnaires about their prior treatments, and undergo a pregnancy test. Each month, the subject will take a pregnancy test at the facility to verify pregnancy status. The massage therapy group will receive a general, full body massage consisting of effleurage (soothing, stroking movements) and petrissage (massage movements with applied pressure, compressing the underlying muscles). The physical therapy group will receive manual therapies that include Muscle Energy Technique (mobilizing joints and relaxing muscles through subtle muscle contraction), positional release, manual lymphatic drainage, and visceral manipulation. Once the treatment portion of the study has concluded, subjects will return to their treatment site once per month for the next three months, or three full menstrual cycles. At these follow-up visits, the investigator will answer questions from the subjects, and subjects will undergo a pregnancy test. At the third follow up visit, she will also fill out another SF-36 form. After these follow-up visits, it will be disclosed to the subjects whether their group was the therapy being studied or the control. Subjects in the massage therapy group (the control) will be offered the physical therapy treatments. If subjects become pregnant during the term of the therapy or the follow-up, their site investigator will call them after their due date to determine the length and success of the pregnancy. Subjects who were originally in the control group who choose to receive the study procedures will be followed, but successes in this group will not be included in the same data set. Each female subject will also have a male partner in the study, with the aim of enrolling 30 subject pairs. The male partners will not have treatment for the study itself, but they will be required to have or to have had sperm testing in order to rule out their infertility as a contributing cause of the couple’s failure to achieve pregnancy. This testing will be done at outside clinics, and results will be shared with investigators. Male participants will have one visit with the investigator in order to obtain consent and authorization, and to discuss the study. We propose to withhold information pertaining to which group each subject has been randomly assigned, and which type of therapy is predicted to be therapeutic. This study will be singleblinded to reduce bias for or against the experimental procedure. By withholding random assignment information, participants should not be affected by the knowledge of what therapy they are receiving. We do not anticipate any additional risks due to withholding this information. Subject pairs are informed that they will not be told which form of therapy they will receive until the end of study. Subject pairs will also be informed that only one form of therapy is the treatment therapy, and one is the control therapy, but that they will not know which until after the study. After the follow-up period, subjects will be offered an opportunity to switch to the experimental procedure if they received the massage therapy. Female subjects will be debriefed at the three-month follow-up by the investigator that administered the treatment. The investigator will reveal what form of therapy (experimental or massage) the subject has received. If the subject received the massage therapy, the investigator will ask if the subject would like to receive the experimental treatment for the following three months. Therapists will recruit subjects at physician offices, OB/GYNs, county health clinics, Planned Parenthood organizations and with general advertising directed at a diverse population of women seeking infertility treatment. Subjects may be informed by her physician (for example, her OB/GYN) about participation in a clinical research study investigating the effects of manual therapy to increase fertility. The physician can refer the subject to the physical therapist who will inform the subject of the study and assess if she meets the inclusion criteria. If the subject is interested in participating, she will go through the informed consent process. Inclusion Criteria a. Women ages 18-42 b. Infertile by Centers for Disease Control definition (unable to achieve pregnancy after one year of unprotected sex) c. Undergoing no other concurrent treatments for infertility d. Partners with normal sperm counts and motility (assessed by physician) e. Women will have had (within one year of screening) or will have a full infertility work up as recommended by the American College of Obstetricians & Gynecologists f. No known reproductive abnormalities g. Have not undergone tubal ligation reversal surgery h. Subject and partner want to become pregnant/have children i. Subject is able to read and understand the informed consent form j. Subject has infertility problems that may be helped by this type of therapy Exclusion Criteria a. Subjects are pregnant b. Subjects are incarcerated c. Subjects are under the age of 18 or over the age of 42 d. Subject’s partner has had a vasectomy e. Subject and partner will not be having unprotected sexual intercourse while the study is taking place and three months after treatments end f. Subject’s partner’s sperm count or motility may be the cause of subject’s failure to conceive g. Subject’s partner refuses to have sperm motility tests administered on him Each researcher will treat and document the subject according to documentation required by their facility and HIPAA laws. In addition to this documentation, data will be collected by each investigator at initial evaluation (utilizing data collection form) and mailed to principal investigators. After this initial data collection, each subject will be identified by a facility code, therapist code and a randomly generated number (e.g., 3.2.8059: facility 3, therapist 2, number 8059). Data collected during the study will be emailed to principal investigators after each treatment session with information using only the number assigned. The data collection forms will be kept separately from the coded identifier list (locked in safe). Subjects will use the Kindara web and phone application to track their sexual activity and send it to site investigators. This study does involve minimal risks similar to those that one would face in a typical therapy session on any given day. The long-term effects of treatment cannot be known. Side effects of treatment may include: • increased urination; • increased sweating; • temporary change in body odor; • uterine cramping; • vaginal discharge; and • mild back pain. All precautions will be taken to protect privacy and confidentiality. If a data breach does occur, the participant will be contacted immediately. The participant is instructed to call her therapist if she experiences any problems or is injured as a result of participation in this study including research related injuries. Stress from dealing with infertility carries its own risks, and subjects and their partners will be informed that participation in the study could make them susceptible to psychological risks. Psychological risks include: • Anxiety • Depression • Isolation • Helplessness • Strained and stressful relationship with loved ones • Thoughts about death or suicide If subjects successfully conceive, pregnancy itself carries risks. In addition, some studies have linked a history of infertility to increased risk of birth defects. However, there is no evidence that the therapies used in this study increase the risk of the subject having a child with birth defects. Treatments could result in pregnancy. Only the rate of pregnancy will be studied, but other possible benefits include: • less pain; • more regular menstrual cycles; or • improvement in sexual function. Participation in this research will help to advance research for infertility. The research could potentially open up a new avenue of treatment for infertility by showing that hands-on treatment alone may be able to treat infertility. Given that current female infertility treatments are generally more invasive and expensive, this treatment could open access to infertility treatment. Risks to the participant are minimal and are equivalent to those that would be faced during typical physical therapy treatment sessions. Psychological risks are the same as those faced by patients with infertility; therefore, the risks are not higher for these patients. Further risks are associated with pregnancy and would be present if the woman becomes pregnant. Pregnancy is the desired outcome and is a benefit which far outweighs any risks anticipated during the study. Some studies have linked a history of infertility and use of infertility treatments to an increased risk of birth defects, but there is no conclusive link. Additionally, there is no current evidence linking massage or physical therapy to birth defects. Conversely, since the benefit of the trial would be successful pregnancies and possibly greater access to a less expensive and less invasive form of infertility treatment than current methods, these benefits to the study patients and those potentially served by the therapy outweigh the minimal risks posed by the study therapy itself and participation in the study. Reporting procedures will include internal reporting within the study, documentation, and procedures for immediate reporting to the IRB. Any adverse event will be immediately reported to the principal investigators (Lauren Mansell and Mary Ellen Kramp), with documentation in narrative form describing the adverse event within 24 hours of learning of the event. This information will be reported to the IRB as soon as the information is relayed to the chief investigators.