November 2014 Small Animal Benchmark
advertisement

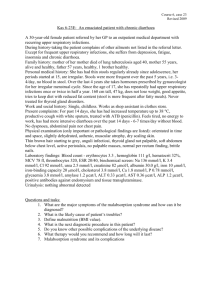
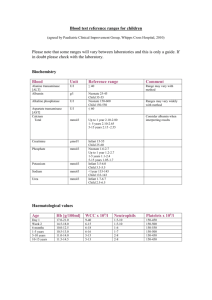
Small Animal Benchmark November 2014 Case 1 A 12-year-old neutered female domestic shorthair cat named “Cookie”(5 kg) presented to the ER for acute blindness. The owners noted that Cookie had been bumping into things in their house for several days and seemed tentative about jumping to and from her feeding station located on a dresser in the basement. The owners also felt like Cookie had been drinking and urinating excessively for the past several months. The cat was exclusively indoors and had no prior medical history, but had last been seen by a veterinarian 10 years ago. Physical examination was unremarkable except for mild tachycardia (heart rate, 220 beats per minute), a Grade II/VI systolic heart murmur, no menace bilaterally, and pupils that were mydriatic with no PLR (direct or consensual). A fundic examination was performed in the ER, and an image of Cookie’s right retina is displayed below: 1. Describe any abnormalities depicted in the image above. Systemic hypertension was suspected and confirmed with indirect measurement of Cookie’s blood pressure (BP) via Doppler (systolic BP: 230 mm Hg). 2. List 5 causes of secondary systemic hypertension in cats and indicate which two are most commonly observed. 3. Excluding the eye, describe clinical evidence of systemic hypertension in 3 different organ systems. 4. Does Cookie exhibit a hypertensive urgency or a hypertensive emergency? Explain. 5. List 5 classes of ORAL antihypertensive drugs available for use in veterinary patients. For each class listed, provide a drug, mechanism(s) of action, and 2 side effects. An emergency venous data was obtained and revealed the following abnormalities: Variable Na+ K+ ClGlucose pH pvCO2 HCO3BE Result 155 1.9 118 160 7.52 34 30 +8 Reference Range 140 – 151 mmol/L 3.5 – 4.9 mmol/L 104 – 116 mmol/L 70 – 130 mg/dl 7.36 – 7.44 35 – 45 mm Hg 18 – 24 mmol/L -4 – 4 mmol/L Your supervising criticalist suspected that Cookie suffered from feline primary hyperaldosteronism (PHA). 6. List ALL of the physical and/or laboratory abnormalities present in this case that supported this diagnosis. 7. Briefly describe the general pathophysiology of PHA. 8. Specifically describe the mechanism(s) via which hyperaldosteronism affects each of the following: a. Effective circulating volume b. Serum potassium concentration c. Systemic acid-base balance 9. Unrelated to systemic hypertension, describe two clinical syndromes and/or organ dysfunctions reported in association with PHA. PHA must be differentiated from secondary hyperaldosteronism (SHA), associated with conditions in which aldosterone production is a normal response to activation of the renin-angiotensin-aldosterone system (RAAS) (e.g., congestive heart failure, hepatic cirrhosis). 10. Describe activation of the renin-angiotensin system (RAS) in patients with SHA. List 8 physiologic effects of angiotensin II. 11. What are the two main stimuli for aldosterone secretion in patients with SHA? 12. List the 4 criteria for diagnosis of PHA in human patients. 13. Describe a) the rationale/utility and b) any limitation(s) of each of the following tests for achieving a diagnosis of PAH in this cat: Measurement of serum potassium Measurement of serum aldosterone (PAC) Measurement of plasma renin activity (PRA) Determination of the aldosterone:renin ratio (ARR) Urinary aldosterone:creatinine ratio (UACR) Abdominal ultrasound (AUS) Oral fludrocortisone suppression test The cat was admitted to the ICU for stabilization and a thorough diagnostic workup. No additional noteworthy abnormalities were noted on CBC or serum biochemistry profile. Thoracic radiographs were normal. Abdominal ultrasound revealed a unilateral right-sided hypoechoic 3.5×2.5 cm nodule adhered to the liver and caudal vena cava. Cookie’s serum aldosterone was 1650 pmol/l (reference interval: 110540) and plasma renin activity was <35 fmol/l/sec (reference interval: 60-630), confirming the diagnosis of PHA. On Cookie’s first day of hospitalization and prior to consideration of surgery for adrenalectomy, treatment of her hypertensive emergency and severe hypokalemia were prioritized. 14. During implementation of emergent antihypertensive therapy, an excessive drop in BP (still within the normal range) in a patient with chronic hypertension may lead to cerebral ischemia. Draw and utilize the cerebral autoregulation curve to explain this finding. 15. According to guidelines for emergency management of systemic hypertension in human patients, what are your initial goals over what time period for BP reduction in a patient with chronic severe hypertension? You elected to start a sodium nitroprusside (SNP) constant rate infusion on Cookie. 16. What is the mechanism of action of SNP? 17. Briefly describe your administration and monitoring protocols for SNP in this cat. 18. Describe the metabolism of SNP as this pertains to risk for cyanide toxicity. 19. List two drugs with possible efficacy for treatment of SNP toxicity from CN - poisoning and provide mechanism(s) of action and limitations of each. 20. Describe the specific effects of hypokalemia on membrane potentials of excitable tissues. 21. Describe how measurement of each of the following may aid in determining the cause or source of potassium loss in a hypokalemic patient: Fractional excretion of potassium (FEK) Transtubular potassium gradient (TKKG) 22. What is indicated by the red arrow in the ECG image depicted below and what is the potential clinical significance of this finding in a patient with severe hypokalemia? Your resident mate suggested to you that perhaps Cookie had been PU/PD at home because of her hypokalemia. 23. Explain how hypokalemia can cause PU/PD. Cookie was discharged on amlodipine, oral potassium gluconate (Tumil-K) and spironolactone while her owners contemplated surgical resection of her aldosterone-secreting adrenal mass. 24. What valuable information could have been relayed to Cookie’s owners pertaining to perioperative complications and outcome in cats undergoing surgery for PHA? Case 2 A 12-year-old FS Puli (15 kg) presented to the ER for a 2-month history of weight loss, and a 10-day history of progressive inappetence, PU/PD and perceived depression. Physical exam documented marked dehydration (estimated 8%), a body condition score of 3/9, mild to moderate diffuse muscle wasting (most notably of epaxial musculature), mild cranial organomegaly, discomfort and lipsmacking upon cranial abdominal palpation, and depressed mentation. Rectal temperature was 102.5F. Thoracic auscultation was unremarkable. Neurologic exam was normal aside from mental dullness. Point-of-care diagnostics are reported below: Blood pressure 134 mmHg (Doppler) PCV/TP 40% / 7.6 g/dL Venous Blood Gas Variable Na+ K+ ClGlucose pH pvCO2 HCO3BE Lactate Result 138 4.6 100 1180 7.365 33.8 18.6 -5.5 4.5 Reference Range 140 – 151 mmol/L 3.5 – 4.9 mmol/L 104 – 116 mmol/L 70 – 130 mg/dl 7.36 – 7.44 35 – 45 mm Hg 18 – 24 mmol/L -4 – 4 mmol/L < 2 mmol/L 1. Interpret the blood gas results: 2. Please calculate the effective osmolarity. How does this differ from calculated total osmolarity? What is the difference between osmolarity and osmolality? 3. Correct the sodium for the degree of hyperglycemia. 4. Describe the hyperosmolar hyperglycemic state (HHS). Does this patient meet the diagnostic criteria? 5. Discuss the pathogenesis of the HHS. 6. HHS and DKA are uncommon consequences of unregulated DM. Discuss common presenting complaints and physical exam findings in these patient populations. Which PE abnormalities are associated with outcome? 7. Discuss common comorbidities and any association with outcome in HHS dogs and cats. 8. Discuss differences in clinicopathologic findings between HNK and HK patients. Which changes(s) is/are prognostic? The patient was admitted to the hospital for rehydration and supportive care, and the following additional diagnostic results were obtained: HEMATOLOGY Variable WBC RBC HGB HCT MCV MCH MCHC RDW Platelet count Bands Neutrophils Lymphocytes Monocytes Eosinophils Basophils Abs. Bands Abs. Neutrophils Abs. Lymphocytes Abs. Monocytes Abs. Eosinophils CELL MORPHOLOGY Result Reference Range 21.8 6.0-17.1 10^3/uL 6.59 5.5-8.5 10^6/uL 13 12-18 g/dL 38.2 37-55 % 58 60-77 fL 19.7 20-26 pg 34 32-37 g/dL 20 14.0-18.5 % 523 200-475 10^3/uL 3 0-3 % 76 60-77 % 8 12-30 % 10 3-10 % 6 1-10 % 0 0-1 % 0.66 0-0.3 10^3/uL 16.57 2.8-10.1 10^3/uL 1.00 0.9-4.6 10^3/uL 2.18 0.1-1.4 10^3/uL 1.31 0.0-1.5 10^3/uL Anisocytosis 1+; Poikilocytes 1+ ; Platelet morphology normal; WBC morphology normal CHEMISTRY Variable Sodium Potassium Chloride Cholesterol Triglycerides ALP ALT (SGPT) AST GGT Total Bilirubin Amylase Lipase Glucose Total Protein Albumin Globulin BUN Creatinine Phosphorus Calcium Magnesium Bicarbonate Creatine Kinase URINALYSIS COLLECTION METHOD COLOR CLARITY SPECIFIC GRAVITY GLUCOSE BILIRUBIN KETONES BLOOD PH PROTEIN WBC RBC BACTERIA EPI CELL MUCUS CASTS CRYSTALS UROBILINOGEN URINE CULTURE: pending Spec cPL: pending Result 136 4.5 99 268 115 1,222 163 243 11 0.4 1,919 1,262 998 6.6 2.7 4.1 68 3.0 6.8 10.7 3.3 19.0 159 CYSTOCENTESIS STRAW HAZY 1.017 3+ NEGATIVE NEGATIVE 3+ 7.5 1+ 20-30 /HPF >100 /HPF 1+/HPF 2+ (3-5)/ HPF NONE SEEN NONE SEEN /HPF NONE SEEN /HPF NORMAL Reference Range 143-153 mEq/L 3.7-5.9 mEq/L 106-122 mEq/L 140-360 mg/dL 40-110 mg/dL 11-140 IU/L 10-90 IU/L 0-90 IU/L 0-12 U/L 0.1-0.6 mg/dL 400-1,500 U/L 77-695 U/L 75-125 mg/dL 5.5-8.0 g/dL 2.5-3.9 g/dL 2.0-4.0 g/dL 8-24 mg/dL 0.5-1.5 mg/dL 2.5-5.0 mg/dL 8.8-11.2 mg/dL 1.6-2.5 mg/dL 16.9-26.9 mEq/L 50-530 U/L CXR: normal geriatric thorax. ABDOMINAL ULTRASOUND REPORT: The liver is enlarged and has a rounded caudal contour. The hepatic parenchyma is diffusely hyperechoic. A small amount of predominantly dependent echogenic debris is noted within the gallbladder. The left renal pelvis is minimally dilated (4 mm). The right kidney is reduced in length (approximately 3.8 cm) and there is minimal corticomedullary demarcation. The right pelvis is mildly dilated (up to 6 mm). The entire ureter is mildly dilated (approximately 4 mm) to the level of the urinary bladder apex. The right ureteral wall is diffusely hyperechoic. The ureters are not identified at the ureterovesicular junction. A solitary hyperechoic calculus is noted within the dependent portion of the urinary bladder (6 mm). A small volume of anechoic effusion is noted in the cranial abdomen. The mesentery/fat and the cranial abdomen is lobulated and hyperechoic. The right aspect of the pancreas, at the junction of the pancreatic body and right pancreatic lobe, is thickened and has a lobulated contour (approximately 2 cm). Within the thickened portion of the pancreas a poorly marginated hypoechoic area is identified (approximately 1 x 1.5 cm). The spleen, stomach, small and large bowel, abdominal lymph nodes and urinary bladder are within normal limits. IMAGING CONCLUSIONS: Focally thickened pancreas in the region of the body/right lobe with poorly marginated hypoechoic area and hyperechoic nodule. Cranial abdominal steatitis and abdominal effusion. Findings are most compatible with pancreatitis. The possibility that the pancreatic changes represent neoplasia cannot be excluded. Minimal/mild bilateral pyelectasia with right-sided right hydroureter with hyperechoic ureteral walls. Findings on the right are suggestive of pyelonephritis and ureteritis. Some degree of pyelectasia may be seen secondary to fluid therapy. The possibility of a bilateral pyelonephritis cannot be excluded. Solitary cystic calculus. Mild hepatomegaly with hyperechoic parenchyma. This is a non-specific finding and differential diagnoses include: steroid/vacuolar hepatopathy, nodular hyperplasia, or chronic hepatitis/cholangiohepatitis. The possibility of infiltrative neoplasia cannot be excluded. A follow-up ultrasound is recommended to monitor for resolution/progression of these findings. Additionally fineneedle aspirate of the pancreas and the liver can be considered for a cytologic diagnosis. 9. Outline a rational treatment plan for the patient’s first day in the hospital. Serum phosphorous and magnesium levels were rechecked the morning after admission and both were found to be mildly decreased. 10. Discuss the pathophysiology and clinical relevance of these electrolyte derangements in animals being treated for HHS and DKA. 11. Based on the AUS suspicion for pancreatitis, fill in the following chart for additional diagnostics that can help support or refute a diagnosis of pancreatitis in dogs and cats. Diagnostic Change(s) Expected Diagnostic Utility Diagnostic Species Specific with Pancreatitis Specificity/Sensitivity Limitation(s) Considerations (if any) (if available) Serum Lipase Activity Serum Amylase Activity SerumTLI PLI SNAP PLI Pancreatic Elastase-1 (cPE-1) Trypsinogen Activation Peptide (TAP) AUS CT Pancreatic FNA Pancreatic BX The use of biomarkers has growing popularity to diagnose and define severity in many disease states. 12. Discuss the following biomarkers and their role in pancreatitis, as well as any evidence for their use in veterinary medicine. Trypsinogen Activation Peptide (TAP) C-reactive protein (CRP) 13. The following therapies are controversial in canine pancreatitis. Defend your argument for or against their use in this patient. Broad spectrum antibiotics Fresh frozen plasma (FFP) 14. When is surgery indicated in patients with pancreatitis and what is the prognosis (in small animals) with surgical intervention? 15. List short term (3) and long term (3) complications resulting from pancreatitis. 16. Describe 2 scoring systems currently published for canine pancreatitis patients. 17. Discuss the arguments for and against early and delayed enteral nutrition in pancreatitis. 18. List advantages and disadvantages of various enteral feeding tube options: Tube Type Nasoesophageal OR Nasogastric Esophagostomy Advantages Disadvantages Gastrostomy Surgically placed jejunostomy/gastrojejunostomy tube Fluoroscopic naso-jejunal tube 19. What role may the following nutritional substances play in immunomodulation of pancreatitis? Glutamine Arginine Probiotics 20. When should one consider parenteral nutrition (PN) for a patient with pancreatitis? Should PN solutions be limited in their lipid content? 21. Develop a nutritional plan for this patient. Take into consideration the patient’s caloric requirements, route and delivery method(s), and nutrient profile considerations. Case 3 Bella, a 10 year old, female spayed Golden Retriever presented to your hospital for dull mentation, PU/PD, and polyphagia. Upon further questioning, the owner reported that over the past several weeks, Bella was intermittently exhibiting bizarre behavior and had been weak in the hind end after exercise or when she was fed later in the morning than usual. Your physical examination was unremarkable. You decided to run a CBC, biochemistry profile, and urinalysis on this patient. The only noteworthy abnormality was a blood glucose of 45 mg/dl. 1. List 3 general categories of differential diagnoses for hypoglycemia (excluding laboratory error/spurious hypoglycemia). Provide 3 disease syndromes that fit under each category listed. 2. How is euglycemia maintained in a normal fasted dog? List the counterregulatory hormones involved in regulation of this process in your answer. You rechecked the blood glucose with a glucometer and confirmed that it is low. Based on the relatively normal physical exam and hypoglycemia noted on chemistry and spot check you are concerned about an insulinoma in Bella. You decided to pull extra blood in a serum separator tube and hold it for additional testing. 3. Briefly describe the composition of the endocrine pancreas. 4. List 4 physiologic effects of insulin. 5. Briefly describe the mechanism(s) for insulin-induced hypoglycemia. 6. List 5 of the most common historical and clinical signs associated with insulinomas in dogs. 7. The majority of clinical signs listed above are attributable to what two major effects that occur secondary to insulin-induced hypoglycemia? 8. How does glucose enter the brain and what are the intracranial compensatory mechanisms for hypoglycemia? 9. Briefly elucidate the mechanism(s) of hypoglycemia-induced neuronal injury. 10. Describe the 3 components of Whipple’s triad. 11. What are some additional diagnostics that you could perform on this patient to confirm a diagnosis of insulinoma? You diagnosed an insulinoma by a high insulin:glucose ratio. Abdominal ultrasound revealed no significant findings. 12. Discuss medical treatment options for insulinoma. You elected to stabilize Bella with glucagon. 13. In a recent study that evaluated the use of glucagon subcutaneously in healthy beagle dogs, the following response to therapy was observed? a. b. c. d. e. Glucagon administered subcutaneously failed to increase glucose concentrations above basal levels at any of the time points measured. Time to peak glucose concentration following subcutaneous administration was 20 minutes. The difference in the insulin-like immunoassay was significantly lower in the intravenous group compared to subcutaneous group. Subcutaneous glucagon increased ACTH but not cortisol concentrations at the 20-minute time point. The most common side effects to subcutaneous glucagon administration were pain at the injection site and vomiting. 14. Outline a protocol for the use of glucagon in this patient. 15. What is the benefit of surgical therapy for a patient with insulinoma? 16. Discuss some preanesthetic considerations for your patient. 17. List 3 potential post-operative complications to be aware of following partial pancreatectomy for insulinoma?