Annual Report for Gloucester Academy
advertisement
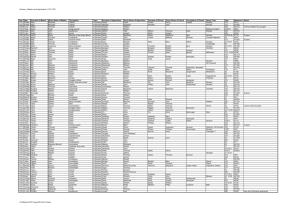
PSYCHIATRY AND ETHICS UNIT (TEACHING) ANNUAL REPORT JULY 2012 0 Contents Introduction ...................................................................................2 Report on Central Teaching ...........................................................3 Examinations in 2011-12 ................................................................4 Ethics ..............................................................................................6 Annual Report for Gloucester Academy ........................................7 Annual Report for AWP NHS Partnership Trust .............................9 Annual Report for Somerset Academy.........................................11 Student Feedback 2011-2012 ......................................................13 Final Site by Site Totals, Units 1-3, 2011/12 .................................16 Site Teaching Timetables for 2011-12 ..........................................19 1 Introduction When I look back to my presentation to all the year 3 students in September last year, my aim was to inspire and encourage the wisest and most thoughtful to consider Psychiatry; not just as a Unit to tick off but as the most holistic of medical sciences that we are all privileged to practice. Since that time there have been many personal and systemic peaks and troughs. Progress is being made, but inevitably in these austere times, there are many challenges, but we must not lose sight of the importance of encouraging and motivating the best of the next generation to consider psychiatry and perhaps more importantly to ensure that ALL our students are encouraged to think and practice in an integrated way that never neglects the human and emotional journey that we are all on. And so to a summary of the year. The major innovation in 2011/12 was the introduction of the new Direct Observation of Clinical Skills (DOCS) exam, in response to GMC and external examiner feedback. This necessitated a change in some aspects of the teaching with a focus on the rehearsal and development of clinical skills, as well as preparation of new style vignettes. On the whole and with hard work from all those involved, the change has been relatively seamless, and the new exam is seen as a major improvement on our previous assessment. There is still work to be done to optimise further, but we can all feel pleased with what has been achieved so far. The challenge will be to develop this further whilst being mindful that our aim is not to prepare Psychiatrists, but foundation year doctors. As a result of the nature of secondary care (and its funding and focus on SMI) we have perhaps moved to far away from the common and “milder” mental disorders; a major aim for the next year will be to ensure that we focus more on these, and this will necessitate optimum collaboration with our Trust teaching deliverers, at a time when there is much uncertainty in their structure, functioning and leadership. Within this we must ensure that students see patients and learn from them as Osler said: - “He who studies medicine without books sails an uncharted sea, but he who studies medicine without patients does not go to sea at all.” On that note I should also add that the “retro” step that we took last year of giving the students a textbook (PRN Psychiatry) has been an unqualified success and other Schools are likely to follow suit! Dr John Potokar, Teaching/Unit Lead 2 Report on Central Teaching This consists of one day of teaching, usually on the 2nd Friday of the attachment. It was comprehensively changed this year, to give students the opportunity to have an overview of the therapies available in psychiatry, delivered by specialists in these areas. Psychotherapeutic (AM) and pharmacological (PM) treatments are covered, as well as Dr Evans’ highly respected mind/body lecture bridging the two parts of the day. Some tweaks have been made following early feedback from the students to both parts of the day with feedback improving. Thus, quantitatively, the last two were as follows (the marks for the 3rd unit are the key ones for pharmacology, as this is the lecturer who will continue delivering these for 2012-2013). Psychological Treatments 1 Unit 3: 3.9 Unit 4: 3.7 Psychological Treatments 2 3.8 3.5 Mind & Brain 4.3 4.1 Pharmacological Treatments 1 4.4 2.7 Pharmacological Treatments 2 4.3 2.8 Qualitative feedback was generally good with no specific themes, apart from a wish to move the Day away from Friday, particularly the afternoon lectures. Logistically, this has not proven possible for a variety of reasons. Therefore, there will be little change for the 2012/2013 talks. There will be a group of speakers, led by Dr Andrew Clark, to provide the morning talks and role play on Psychological Therapies, with Dr Evans bridging to the afternoon with his mind/brain talk, followed by Dr Melichar in the afternoon covering Psychopharmacology. Dr Jan K Melichar, Central Teaching Lead 3 Examinations in 2011-12 The examinations for psychiatry and ethics in 2011-12 ran smoothly, predominately because of the significant amount of work by the clinical lecturers and the administration staff. There were some changes to the exams for this year, particularly in the clinical assessments and the feedback to students. Overall unit assessment scheme The overall assessment consists of two parts; component A (clinical assessment) and component B (written assessment). Component A – the clinical assessment has one part: Direct Observation of Clinical Skills (DOCS) Examination Component B-the written assessment has three constituent parts: Written Examination (EMQ/MCQ) (50% of component mark) Internal Psychiatry SSC (33% of component mark) Ethics Written Case (17% of component mark) Candidates must pass component A (40% of the total Unit mark) and component B (60% of the total Unit mark) to pass the Unit. To pass component A students must receive a mark of at least 50%. To pass component B students must receive a mark of at least 45% in each of the three constituent parts and a mark of at least 50% for the component overall. Clinical assessment (Component A) The clinical exams have used the viva format for many years. It was decided to change the format this year for a number of reasons. Firstly the psychiatry exam committee had been concerned for a number of years that some students, who were not weak candidates, failed the exam and that some borderline students, who might have passed in other units, failed psychiatry. Secondly, the GMC had indicated that vivas were not the most appropriate method of examining students and that more standardized methods should be introduced. Thirdly, the external examiner suggested that the clinical examinations should assess clinical skills as well as knowledge. Fourthly, other medical schools are changing their examinations. Given this background DOCS were introduced. DOCS (Direct Observation of Clinical Skills) are similar to an OSCE (Objective Structured Clinical Examination) but have fewer stations. The DOCS in psychiatry consisted of three stations with each station having a stimulated patient (ie an actor with a standardized history of a mental disorder). 4 Each station lasted 15 minutes which included 1 minute for the candidate to read the instructions, 12 minutes to perform the allotted task and 2 minutes to transfer to the next station (and for the examiner to decide the marks). The candidate moved directly from one station to the next and completed three stations in total. Thus the whole assessment took 45 minutes for each candidate. There was a single examiner at each station, and so each candidate was assessed by three different examiners. The candidate was marked across three domains, by the examiner, at each station and there was also a mark from the actor. The domains were approach to the patient, knowledge (asking the correct questions) and approach to the task (final summary) patient. Each domain was 30% of the mark for the station with the final 10% being the actor’s mark. Each of the three stations contributed a third of the overall mark. Given that this was a new examination, there was concern about the whole process, particularly the marking. In the event, all the exam days went well and the feedback from the students and examiners was positive. The marks were very similar with the previous year’s viva and there were no major differences between the units. Summary statistics of DOCS mark distribution for Psychiatry DOCS 2011-12 (and unit 4 viva 2011) Unit 4 –May 12 Unit 3-Mar 12 Unit 2-Jan 12 Unit 1-Nov 11 Viva (Jun11) Number of students 62 62 64 60 62 Mean mark (SD) 64.4 (4.8) 65.2 (5.5) 65.2 (4.8) 63.1 (4.6) 64.2 (8.5) 64.4 65.4 65.1 62.7 64.5 51.8-73.9 51.6-78.3 51.3-78.0 51.7-75.1 50-86 Median Range The main area of concern was that there were no fails in the clinical assessments (compared to 6 in 2010/11, 7 in 2009/10 and 8 in 2008/09). On this point there was reassurance from the external examiner who reported that the assessments, in her view, were probably too difficult. Written assessment (Component B) Changes to the written assessment were less that those to the clinical assessment. The main change to the end of year written examination was the use of the Angoff method as a form of criterion referencing. This had been piloted last year. The clinical academics continued to have some concern about criterion referencing in general with somewhat limited evidence that it was any more reliable that norm referencing. However, given that the university and the GMC have indicated that criterion referencing should be used, it was used this year. The result was that every candidate passed the end of year written exam (norm 5 referencing would have resulted in one candidate, who was more than 4 standard deviations below the mean, failing the examination). Given the change to the clinical assessments, in particular the loss of the long case, the iSSC was altered slightly so that the presentation started with a brief description of a case from which the main topic came. This was reflected in a minor adjustment to the marking scheme. There were no significant changes to the ethics assessment. Marks to the students Bristol University has fared badly in recent years in the students’ survey and one area of concern has been feedback. The Year 3 committee therefore decided that marks should be given to the students as soon as was possible after each exam. For psychiatry, marks are now available for each student individually after each DOCS exam. The available marks are the total for each station and the overall total for the clinical exam. For the written exam, the marks are available for the combined MCQ/EMQ, the iSSC and ethics. Changes for next year Changes for the coming academic year will be limited due to the significant changes this year. There will be some minor alterations of how the different parts of the exams are combined. There will also be some modifications of the DOCS. The setting of the MCQ/EMQ paper should be easier as the University joins with other universities in producing a large bank of questions which participating universities can use. Thanks to the clinical lecturers, the administrative staff, the examiners and the actors for a successful year which was very satisfactory given the significant changes made to the assessments. Dr Tim Amos, Examinations Lead Ethics Owing to maternity leave for Dr Ainsley Newson, Dr Natasha Hammond-Browning took over as Ethics element Lead in January 2012. Kerry Gutridge will be replacing Natasha from September 2012 to January 2013, it is expected that there will be a new person in a permanent role from January 2013 onwards. General Assessment: The Ethics Element continues to run smoothly. The standard of ethics case reports by students continues to be good and some were outstanding, we had a high number of distinctions this year. Feedback on case reports continues to be made available to students on an ‘opt-in’ basis, drawn to students’ attention in the handbook. However, we are looking at changing this to an automatic system of 6 informing the student of their feedback as the current system is time consuming to the administrator and not all students ask for feedback, including the weaker students who may need this. In future, all students will be sent their feedback once it becomes available, without their mark. Any students who have failed will be contacted and offered a face to face meeting to discuss the feedback. A record will be kept of those students who do/not take up this option. Grades will no longer be released by the Centre for Ethics in Medicine. Academy teaching has run smoothly and I would like to take this opportunity to formally thank all the academy ethics element co-ordinators and tutors for making the 2011/12 iteration of the course a success. Note on changes since last APR report: None that I am aware of. Points of Note: Fortunately I was able to hold an informal Away Day with the majority of the academy ethics tutors in April 2012. This was a very informative session where the tutors discussed teaching methods and suggested alterations to the content of the tutorials. This has been taken on board and will be largely incorporated into the new updated teaching materials. Unfortunately it was not possible to hold the 2012 ‘Training the Trainer’ Ethics Away Day due to time tabling/work constraints of both the ethics element lead and academy ethics element co-ordinators. The running of this event will be attempted again for 2012/2013 although it is envisaged that similar problems will be encountered. However, the ethics element lead remains available to offer advice and support for academy tutors and leads. 2 students failed Ethics this year and are resitting. Looking ahead to 2012/13 Continuing good relations with ethics tutors is foreseen and support provided through regular contact and advice. Dr Natasha Hammond-Browning, Locum Ethics Lead, June 2012 7 Annual Report for Gloucester Academy We had 45 students this year and the following are the highlights from 2011/12: Changes in Personnel Dr Attila Sipos left 2Gether NHS Foundation Trust for the sunnier climes of Basel, Switzerland in March 2012. We also lost Dr Ian Parnell, a dedicated and well respected education supervisor & internal iSSC examiner, who retired this year. We would like to extend our thanks for a job well done as well as our best wishes on their future endeavours. I was appointed to the task of filling Dr Sipos’ considerable shoes and took on the unit coordinator role in February 2012. Introductory Lecture Week and Weekly Tutorials The introductory week of lectures was generally successful and well received. The students found the sessions informative and many said it helped prepare them for their psychiatric block. A few complained about the length of the day as they had to sit through up to 5 different sessions in a day. A couple of students also complained about the intensity of the week and stated their preference for the lectures to be spread out across the attachment. However, most students preferred the introductory week to remain. The single 2½ hour MSE role-play session introduced 2 years ago was expanded to 2 consecutive sessions per attachment this year. These sessions aim to develop students’ interview skills with a focus on eliciting relevant psychopathology and information to perform a risk assessment. In each session, the students were divided into 2 groups; each with a facilitator (consultant psychiatrist or higher trainee) and a professional actor who played various patient roles. The expansion allowed every student the opportunity to be in the “hot seat” at least once. Feedback has been excellent with students wanting more of the same as well as having an additional session at the end of the attachment for exam practice. Clinical Placements We have continued to run a clinical placement system, which allocates students to individual Educational Supervisors across the three localities in our county. Students were allocated to specific teams (either inpatient or community) and were swapped round halfway through their attachment. Sessions with the Old Age & Learning Disability teams were timetabled into their schedule. Students were encouraged to explore other psychiatric sub-specialities and contact numbers/e-mail addresses were given in their welcome packs. 8 SIFT money was used to pay for a PT nurse, based with the Hospital Liaison Team. In return, our students were allocated to spend a day with the team. The student starts his/her day with a 1 to 1 session with either the consultant or team manager who goes through a 45 minute tutorial on Deliberate Self Harm and Risk Assessment. The student then shadows a member of the team on the rounds through A&E and the general hospitals. Feedback has been excellent and the Director of Medical Education has reassured me he will continue to support this. Junior Doctor Mentoring Scheme This scheme assigns each medical student to a junior doctor in their locality, who is able to offer additional support during their placement. The scheme is generally well received though unfortunately, it did not happen for students in Unit 3. The main reasons include the departure of the junior doctor coordinating this, as well as a significant change in junior doctors during the change over period. Future developments & challenges Changes in how mental health services in Gloucestershire are provided as well as in medical staff work patterns continue with the implementation of “Fair Horizons” in April 2012. As yet, there has not been significant impact on teaching though the changes in team bases has led to a few students in Unit 4 having difficulty contacting their allocated education supervisor/community teams. We plan to look into our current structure this summer to adapt to these changes. From the next academic year, once software issues have been resolved, students in Gloucestershire will be loaned iPads for the duration of their psychiatric attachment. Applications related to psychiatry, psychiatric notes and textbooks as well as links to on-line education resources will be enabled on these devices. Students will be able to access lecture/tutorial materials & handouts as well as the means of saving the material to a personal account or to have them printed. We are also looking into the possibility of using “Facetime” as a means of communication between the students and me. Dr Seng Hoong Tan, Unit Coordinator, Gloucester Academy Annual Report for AWP NHS Partnership Trust Clinical Teaching Fellow The Clinical Teaching Fellow, Dr Kate Seddon, completed her time with AWP on 30 June 2012. Kate has been a great asset and will be missed. Dr Nicola Taylor has been appointed to the Clinical Teaching Fellow post and she begins on the 1 August 2012. I look forward to welcoming and working with her. 9 Educational innovations across AWP: - Further development of mentorship scheme for students during the Unit. Mentors are generally junior doctors to provide a further opportunity to develop themselves as educators. This continues to run well in some sites and is receiving positive feedback from both mentors and students. The mentors have started to meet up for peer supervisions and the aim is to evaluate this formally over the next few months. - Ongoing development of educational resources - including creation of guides for teachers, database of teachers and development of the undergraduate section of the intranet. - We have created the new post of Associate Undergraduate Unit Tutor (AUUT). The Associate Unit Tutor is a formal, extended role and is aligned to recognised educational standards. Senior trainees apply for the role through a competitive process. They share the tutor’s responsibilities, with a focus on developing new learning approaches and opportunities. We have 6 AUUTs currently appointed – acting in all sites except Devizes. - Kate Seddon and Liz Anderson have a poster accepted at the AMEE conference in Lyon this August on the AUUT and Mentorship Programme. - Ongoing work developing educational supervisors across the Trust. Workshops have now been run at the majority of sites and a draft document outlining the roles and responsibilities of the Educational Supervisor has been developed. - Continuation of the Educational Programme for teachers of medical students within AWP. We have now run all 3 modules multiple times and plan to develop this further Kate Seddon and Liz Anderson presented a Poster about this programme at the Association for Medical Education Europe (AMEE) conference in August 2011. Sites AWP employs 6 site tutors: Eva Dietrich (North Somerset), Catherine Thompson (South Bristol), Sian Hughes (South Gloucestershire), Martin Marlowe (Bath), Hugh Herzig (North Bristol) and Kumar Selvarajah (Devizes). Dr Selvarajah and Dr Dietrich leave us at the end of this academic year and we will be advertising for replacements. The site tutor posts in South Gloucestershire and Bath will also be re-advertised in July as these are three yearly posts and they are up for renewal. 10 There has been a common challenge across the sites, namely the redesign of services (changing from sector teams to teams based on specialties or functions), educational supervisors moving or reducing in numbers and reducing number of inpatient beds. A challenge for all sites is to provide an educational experience for the student where the student can feel part of a team (as would be the case in an apprenticeship model with a consultant in a team) and an educational experience where the student can move to other teams to gain a wider and more standardised let of clinical experiences (eg inpatient and community, general adult and later life etc). Educational supervisors now work in specialist functional teams and we will need to find new ways of providing diverse clinical teaching and experiences. SIFT Budget It did not prove possible to restructure the SIFT budget as this would have destabilised some posts. I have now been informed that this is no longer the case and I am in the process of putting together a briefing on a proposed budget, the principles of which have been agreed. Hopefully this can now be completed for the next financial year. RIO Much work went into trying to get students a RIO card so that they could access the electronic patient record. The logistics of this were onerous and unsuccessful. A survey of medical students confirmed this. The Trust is looking into providing a RIO reader for second opinion approved doctors (SOADs) and may consider this option for medical students too. We do not plan to repeat the attempt to get RIO access next academic year. Conclusion AWP has undergone a major re-design of services in the second part of the academic year. Despite this, there has been ongoing development in education provided by AWP. The biggest challenge facing us is in the next academic year is to provide good and standardised clinical teaching. Dr Geoff Van Der Linden, Associate Director of Medical Education (undergraduates), AWP NHS Partnership Annual Report for Somerset Academy This year we have had 30 students. There are no major problems to report. The students have had a variable interest in Psychiatry. All have succeeded in passing the unit. As usual, some have engaged better with the subject than others. As is frequently the case for this unit, students are somewhat wary of a psychiatric placement at the start but often say they have enjoyed it at the end and will consider Psychiatry as a career. 11 The students are based in Taunton where they live in the Canonsgrove Hall of Residence and have at least around one day a week in Taunton. They start with an induction which includes learning on the RIO computer system in the first week. They then have seven weeks’ medical practice being placed in Taunton, Bridgwater, Wells or Yeovil. During the placement they spend one day a week in Taunton with weekly case presentations, some formal instruction, OSCE practice, expert patient led sessions, and Ethics teaching. Some of the required activities are delivered through the timetable, for example instruction and experience of ECT, Learning Difficulties and Child & Adolescent Psychiatry. Some of the teaching days in Taunton involve the use of expert patients and carers which this year have included patients with schizophrenia, bipolar disorder, anorexia and learning difficulties and carers. This placement concentrates as required on Adult Psychiatry but all students have experience of Old Age Psychiatry and Child & Adolescent Psychiatry through timetabled clinics. The placement feedback from formal teaching and tutor support is generally good. Students tend to appreciate the opportunity of having formal instruction on what they should learn and opportunities to practise OSCE-type scenarios. They also enjoy seeing the patients. The students’ perceptions of their educational supervisors on the clinical placement have been somewhat varied. Some of the educational supervisors are highly rated and seen as very supportive but others were less well rated. Problems delivered in the clinical component of the course include: (1) The shrinking number of inpatient beds. Inpatient treatment is now provided on three sites – Wells, Yeovil and Taunton. Students naturally would prefer to be based in Taunton but it has not been possible and some have therefore been involved in travelling long distances. (2) An additional complication this year, and particularly for the last group of students, has been that the inpatient facility for adults was closed in Taunton and moved to Bridgwater, only moving back in May, causing a great deal of disruption. (3) Most psychiatry care is delivered in the community. Students always find it difficult to travel, particularly to the outlying units. (4) Many of our Consultant colleagues have changed jobs this year with retirements and reorganisation, often disrupting student placements. The overall number of Consultants has declined but the workload has not and some Consultants are less keen to prioritise time for teaching. 12 (5) It is very difficult for students on a short placement to find their “way around” particularly as care is delivered in a multidisciplinary ways by different people in different locations and at different stages of care. Many staff are also part-time which is an added difficulty. I have been trying over time to improve the quality of placements but this has meant chasing educational supervisors based outside of Taunton. Attempts to get colleagues to commit to have students in their clinics in advance are difficult to arrange as people find it difficult to plan ahead. The Consultant involved in Drugs & Alcohol is on long term sick leave. I am trying to timetable more and more of the activities with some success. I have also started to ensure that case presentations are done formally on days of teaching in Taunton so everybody gets the chance to present once or twice and also I have started to allow time to ensure that I observe all the students interviewing patients rather than relying on the Consultant supervisors to do these tasks. This ensures that all students give at least one or two case presentations and are observed interviewing patients. Parts of the students’ assessments involve presentation of a topic of interest allied to Psychiatry to an audience. Students say they generally enjoy this and the topics are usually well presented and interesting. Students have a chance to present initially to the Post Graduate Educational Meeting and they can use the feedback from this to improve their presentation which usually is a few days later. A student this year has failed their SSC presentation which are often of a good standard and variable content. Dr Jackie Rossiter, Unit Co-ordinator for Somerset Academy Student Feedback 2011-2012 Written end of placement feedback was received from 242 of 248 students (97.6%). The feedback questionnaire was reviewed and shortened from previous years, and an important new addition was the inclusion of comment boxes for students to capture experiences not covered by the multiple choice feedback questions. Students in the first three units completed this revised version of the paper-based feedback administered in previous years. A new medical school feedback policy was introduced towards the end of the academic year, requiring units to administer centralized web-based feedback, and amend existing questionnaires to include mandatory questions for the General Medical Council. Consequently, the Unit 4 feedback was not directly comparable to the previous units in the academic year. The quantitative summary in this report therefore summarizes feedback collected from Units 1 to 3 of the academic year (reported by 184 of 186 students). Unit 4 feedback is not included in the quantitative summaries below 13 due to a different methodology and wording of questions. However, the qualitative themes at the end of this report include those received from all units including Unit 4. As in previous years, four endpoints have been used to compare performance across units and sites. A fifth qualitative section is included at the end of this report, reflecting themes arising out of student comments in free text responses to the new questionnaires in all units. 1) Average Score for ‘Supervision and Monitoring by Consultant’ (Rated as 1=Poor, 2=Satisfactory, 3=Good, 4=Very Good, 5=Excellent). The average score for 184 students completing the feedback was 3.6, which corresponds to an average rating of Good to Very Good, and comparable to previous years (2010-11 3.8; 2009-10 3.8). The highest average scores at individual sites were achieved by Weston (4.2, 16 students), Gloucester (3.9, 35 students) and Southmead (3.7, 20 students). As in recent years all 8 sites achieved an overall average score of 3.0 or more, compared with seven out of eight in 2006-7 and four of eight in 2004-5. There was one instances of an average score for a unit at Taunton dropping below the minimum standard target of an average score of 2.0 (compared to no instances in past 3 years). The scores for individual sites were consistent across the units. 2) Average Score for ‘Overall Quality of Clinical Attachment’ (Rated as 1=Poor, 2=Satisfactory, 3=Good, 4=Very Good, 5=Excellent). The average score for 184 students in 2011-12 was 3.6, similar to the previous year’s average of 3.8. This also lies between ratings of Good and Very Good. Weston led the scores, achieving an overall average of 4.1 followed by Taunton (3.9, 24 students) and Callington Road (3.8, 30 students). As in each of the last 4 years, all 8 sites achieved an overall average score greater than the predetermined ‘standard’ of 3.0. There were 3 occasions where sites dropped below this minimum standard target for an individual unit (in 2010-11 and 2009-10 there were also 3 such instances). A declining trend in ratings was noted for Devizes and Bath. 3) Percentage availability of twelve predetermined ‘essential’ activities /opportunities. Twelve activities/opportunities have been judged as essential. The ‘opportunity’ to participate rather than actual participation is assessed, in order that a site’s feedback would not be adversely affected should students choose not to attend a particular activity offered. Two items from previous years have been 14 revised for the current year. Overall in 2011-12, 89.6% of these essential activities were offered. This is comparable to 2010-11 (90.9%), 2009-10 (90.6%) and 2007-8 (90.8%), and higher than in 2008-9 (89.5%) and 2006-7(85.0%). Based upon the above feedback from the first three units, two sites, Bath (81.4%) and Devizes (80.8%) did not meet the 85% target (all 8 sites averaged above these criteria over past three academic years). The best overall score was achieved by Southmead (94.9%), Taunton (94.4%) and Gloucester (93.7%). There were seven instances of failing to meet the 85% target in a Unit – compared with two and five in the past two academic years respectively. A decline in ratings with each passing unit was observed for Devizes, an improving trend for Bath, and a hint of a declining trend was noted for Callington Road. Other sites were consistent. 4) Percentage availability of all twenty-eight predetermined activities /opportunities. This endpoint refers to a range of twenty-eight activities/opportunities, including the twelve ‘essential’ activities/opportunities listed above. Overall, 85.3% of these activities were offered (c.f 84% in 2010-11, 82.6% in 2009-10, 80.0% in 2008-09, and 80.2% in 2007-8), with all sites scoring over the pre determined target of 70%. There was only one specific unit where a site failed to meet the 70% target (Devizes Unit 3, 63.1%), the same as occurred in the past 4 years. The highest scores were at Taunton (92.7%) and Gloucester (90.2%). 5) Themes arising from qualitative feedback received from students Qualitative written feedback was received from all Units and the main themes arising are summarized below. Verbatim feedback has been passed on to site tutors for actioning specific issues. The points below are an attempt to thematically summarise issues raised by two or more students independently: Students have consistently stating enjoying the theory and clinical practice of Psychiatry, especially when teaching was inspiring, and based in clinical situations. Consistently excellent feedback has been received for providing Psychiatry PRN textbook and its content and readability has been highly rated. Students at all sites have praised their site tutors for the support but some students have found it difficult to contact educational supervisors and site tutors. Some specialist placements e.g. Liaison Psychiatry, Learning Disability Day and Eating Disorders have received positive feedback from multiple students. Clinically orientated teaching and experiences have received most positive feedback, and most complaints are about the lack or not having enough of these. Related to this, some students have felt they had a lot of free time and consequently felt the Psychiatry placement should be shorter. 15 Students at almost all sites stated they would like more clinical experiences, and would like more day to day contact with clinicians. They would like more exam practice nearer the end of the placement. Several students across sites have been made feel unwelcome by psychiatrists as well as other clinicians, and felt discouraged and left uninspired by this. Some chronic issues seem to be: a) access to wards and patients in Southmead hospital wards b) Unwelcoming and unpleasant experiences have been reported by several students throughout the year placed with the Bath Crisis Team c) In Devizes, several students felt unable to access specialist clinics or teams such as Drug and Alcohol Services/Forensic unlike their peers in Bristol. Problems with organization such as incorrect timetables and repeated rearranging of teaching sessions has been highlighted for some placements, and has come up on several occasions at Callington Road. RIO cards to access clinical notes arrived too late or not at all for several students on AWP placements at Southmead, Blackberry Hill Hospital, Bath and other AWP sites. Internet access has been an issue at some sites (Bath, Devizes). Community based work and long distances and driving has been raised as an issue for out of Bristol placements. Although the overwhelming majority of students reported enjoying psychiatry, the above qualitative feedback provides a rich resource of ideas for improvement of individual sites and the organisation of the block to ensure our students’ time in Psychiatry is a positive and enjoyable learning experience. Final Site by Site Totals, Units 1-3, 2011/12 In total 184 of 186 students completed the feedback questionnaires in Units 1-3. A further 58 out of 62 students completed a new online questionnaire in Unit 4 but since the questions were not identical, summary scores below include only unit 1-3. Tables 1 & 2 are based on ratings of 1-5, where 1=poor, 2=satisfactory, 3=good, 4=very good and 5=excellent. 16 Table 1: Average score for “supervision and monitoring by consultant” (min standard 2.0) Rank Site Unit 1 Unit 2 Unit 3 AVERAGE 2011-12 Average 2010-11 Average 2009-10 Average 2008-9 1 Rank 201011 8 Weston 4.2 4.3 4.2 4.2 3.2 4.1 3.9 2 7 Gloucester 3.9 3.9 3.8 3.9 3.6 3.6 4.1 3 2 Southmead 4.0 3.6 3.5 3.7 4.0 3.7 3.4 4 1 Callington 3.9 3.5 3.6 3.7 4.2 3.8 3.4 5 3 BBH/Fromeside 3.6 3.4 3.6 3.5 3.9 3.2 3.2 6 6 Taunton 3.5 1.9 4.1 3.2 3.7 4.1 3.7 7 4 Devizes 3.7 2.8 2.8 3.1 3.8 4.2 4.1 8 5 Bath 2.8 2.5 3.7 3.0 3.7 3.9 3.9 Table 2: Average score for “overall quality of clinical attachment (min standard 3.0) Rank Rank 201011 Site Unit 1 Unit 2 Unit 3 AVERAGE Average Average Average 2011-12 2010-11 2009-10 2008-9 1 8 Weston 4.5 3.8 3.8 4.1 3.3 4.1 4.2 2 3 Taunton 3.9 3.8 4.1 3.9 3.8 4.1 3.6 3 1 Callington 4.3 3.3 3.9 3.8 4.3 3.5 3.1 4 7 Southmead 3.8 3.4 4.2 3.8 3.5 3.9 3.6 5 4 BBH/Fromeside 3.9 3.2 3.9 3.6 3.7 3.4 3.3 6 2 Gloucester 3.5 3.9 3.3 3.6 3.9 3.6 3.7 7 5 Bath 3.5 2.8 2.8 3.1 3.7 4.1 3.7 8 6 Devizes 4.2 3.0 1.8 3.0 3.6 3.4 3.7 17 Table 3: Percentage saying yes as to whether each of 12 essential activities took place during their attachment. (Predetermined target 85%) Rank Rank 201011 Site Unit 1 Unit 2 Unit 3 AVERAG E 201112 Averag e 201011 Averag e 200910 Averag e 20089 1 6 Southmead 97.1 96.9 90.3 94.9 90.7 88.1 87.8 2 2 Taunton 93.8 95.8 93.8 94.4 93.4 93.8 88.1 3 4 Gloucester 88.2 95.1 97.2 93.7 91.5 91.3 93.8 4 3 Callington 92.4 89.0 87.5 89.6 92.4 90.9 88.4 5 8 BBH/Fromeside 91.7 92.6 80.7 88.7 87.5 86.6 88.6 6 1 Weston 95.8 91.7 76.4 87.5 93.5 96.1 89.2 7 7 Bath 77.8 81.9 84.5 81.4 87.7 87.7 89.9 8 5 Devizes 91.5 83.1 68.1 80.8 91.5 90.3 89.2 Table 4: Percentage saying yes as to whether each of all specified activities took place during their attachment (Predetermined target 70%) Rank Rank 201011 Site Unit 1 Unit 2 Unit 3 AVERAG E 201112 Averag e 201011 Averag e 200910 Averag e 20089 1 1 Taunton 92.0 94.1 91.9 92.7 88.3 87.0 80.2 2 6 Gloucester 90.6 86.6 93.4 90.2 81.9 81.5 83.5 3 3 Callington 89.6 84.9 85.7 86.7 85.7 82.5 77.2 4 5 BBH/Fromeside 87.8 87.3 81.0 85.5 82.5 78.4 77.3 5 2 Southmead 87.1 83.0 85.1 84.9 86.3 83.9 81.5 6 8 Weston 86.9 94.6 73.8 83.9 80.6 91.2 84.6 7 4 Bath 75.0 73.2 81.4 76.5 84.1 79.3 80.3 8 7 Devizes 83.2 74.8 63.1 73.7 81.2 79.0 73.1 Dr Dheeraj Rai, Feedback/Quality Monitoring Lead 18 Site Teaching Timetables for 2011-12 Topic Bath Phen/Classification Week 1 Week 1 Callington Road Week 1 MSE/History Taking Week 1 Week 1 Week 1 Week 2 Intro Substance Misuse Intro Affective Disorders Intro Anxiety Disorders Intro Old Age/Dementia Intro Schizophrenia (2) Substance Misuse (2) Affective Disorders (2) Anxiety Disorders (2) Old Age/Dementia (2) Schizophrenia Week 7 Week 1 Varies between wks 3-8 Weeks 4/5/6/7 Within 1st 2 weeks Within 1st 2 weeks Within 1st 2 weeks Within 1st 2 weeks Within 1st 2 weeks Within 1st 2 weeks Weeks 4/5/6/7 Week 2 Tutorial wk 5 Roleplay Wk 2 Within 1st 2 weeks Within 1st 2 weeks Within 1st 2 weeks Within 1st 2 weeks Within 1st 2 weeks Within 1st 2 weeks Weeks 4/5/6/7 Weeks 4/5/6/7 Weeks 4/5/6/7 Week 3 Tutorial wk 3 Roleplay Wk 2 Weeks 4/5/6/7 Weeks 4/5/6/7 Weeks 4/5/6/7 Week 5 Week 5/6 Weeks 4/5/6/7 Weeks 4/5/6/7 Weeks 4/5/6/7 Week 4 Roleplay Wk 3 Weeks 4/5/6/7 Week 3 Week 3 Week 6 Week 4 Weeks 4/5/6/7 BBH Week 1 Week 1 Week 2 Week 1 Devizes Gloucester Southmead Taunton Weston Week 1 Week 1 Week 1 Week 1 WEEK 2 Week 1 & Roleplay Weeks 2 & 3 Week 1 Week 1 Week 1 WEEK 1 PLUS VIDEO Week 1 Week 2 or 3 Week 2 Week 3 Week 2 Week 3 Week 1 Week 1 Week 1 Week 1 Week 1 & Wk 6 19 WEEK 4 Week 1 WEEK 2 Week 1 WEEK 3 Week 1 WEEK 3 Week 1 Week 5 & revision Week 2 & revision Week 3 & revision Week 4 & revision Week 1 WEEK 2 In supervision In supervision In supervision WEEK 7 WORKSHOP WEEK 7 – Risk Assessment Weeks5 Week 1 Week 2 Week 3 Week 1 Week 1 Exam Prep/Revision Weeks 7 On going On going Covered with Clinical Tutor Week 6 On going Mental Health Act Week 3 By the end of Week 3 Covered with Clinical Tutor On going Week 2 (varies) Week 1 Pharmacology By the end of Week 3 Week 3 (varies) Week 4 & 5 Week 1 & throughout Week 8 Week 3 Tutorial within 1st 4 weeks Week 2 2 students a wk over 3 wks Video available and advised to visit ECT suite Tutorial within 1st 4 weeks Week 3 Specialist subjects User perspective Therapies week 3 Learning Disability – ½ day on week 5 User perspective Throughout Rethink sessions Learning difficulties Week 4 & 5 Learning Disabilities – students attend in two’s CAMHS Extra tutorials ongoing Child & Family – Students attend individually Clinical Psychologist – wk 5 20 Every Monday course tutor WEEK 4 Week 7 ECT DSH – allocated day with Liaison Team WORKSHOP WEEK 5 Rethink sessions CAMHS Video in the first weekadvised to visit ECT suite and make contact with Ben Ford Wk 3 – Eating Disorders Wk 4 – Early Intervention Psychosis Wk 4 – Learning Disabilities’ Day Wk 5 – CBT Wk 6 – Personality Disorder Workshop Perinatal wk 5 PTSD wk 4 Additional Lectures Eating Disorders/Child & Family Suicide & Deliberate Self Harm 21