marla
advertisement
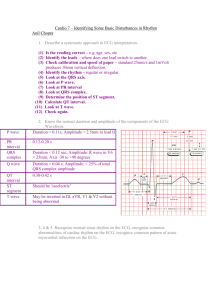
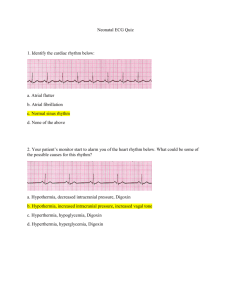
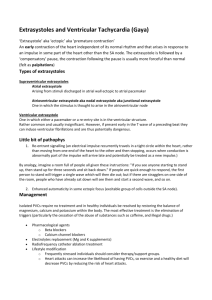
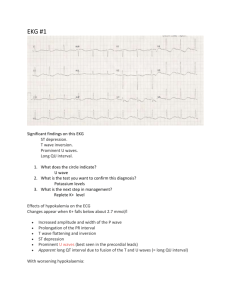
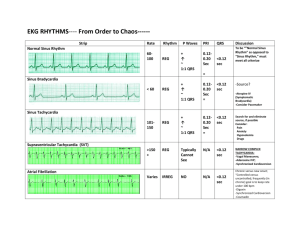
Cardiac and respiratory, read your chapters (which ones) Understand medications (Ca channel blockers) med math(Heparin), think about what’s relevant for heart & lungs. Know tracheostomies, fenestration, when to use a balloon. The respiratory is responsible for ventilation; the cardiac system is responsible for perfusion. Know anemia types, if hemoglobin decreases you have less oxygen, could have an MI because of it. Chest tubes-lung collapses in the case of pneumothorax, hemothorax (blood), the goal of a chest tube is to remove air or fluid out of pleural space. Know purpose of three chest tube chambers (not supposed to see vigorous bubbling, only gentile) Review complications post-op, i.e. why we ambulate, DB+C, move side to side in bed, role ankles, pumping q1h, LMWH, what are you trying to prevent? Pneumonia-an inflammatory process triggered by infections causes excess fluid in the lungs, nosocomial more resistant you need to know when infection occurred (CAP or HAP) Blood thinners(thrombolytics & anticoagulants, antiplatelets, baby asa 81mg, monitor creatinine clearance, Lovenox, Fragmin, Warfarin (antidote vitamin K, new one has no antidote). ‘Pril’- ace inhibitor, ‘lol’ beta blocker, ‘arten/zem’ calcium channel blocker. Gases-the kidneys compensate over time, not right away, look at pH, bicarb, carbon dioxide, pa02<60=hypoxia. Be able to identify main causes that you see. ABGs, K+ moves, acidotic=hyperkalemia. Remember normal cycles of inspiration & expiration, remember basic priniciples. Thin tall guys, smokers (bleb rubture) pneumo/hemothorax. MI, the three main coronary arteries branch off L main, atherosclerosis plaque will crack, body tries to find it, clot causes MI(but not only reason), when we look at ECG… The gold standard is a cardiac catheter, those who have a STEMI are priorities, NSTEMI usually don’t need cath. No labeling but you need to know parts. 6-8 weeks to heal, tissue is very fragile because macrophagues are eating dead tissue. Remember if someone complains of chest pain =Oxygen, PQRST, IV, EKG (ST elevation is the biggest indicator for thrombolytic- a candidate for TMK). ST elevation, and not to of had a recent surgery to become a candidate for TMK. After the first spray call 911, and not to drive themselves to the hospital. Angina is a precursor for heart attack but there is unstable. Unsafe to give Nitro if tachycardic>100, or BP too low<90/60, then consult with DR. Risk factors-consider if their modifiable or nonmodifiable. Statins lower LDL and increase HDL, reduce by 50% if 2 is unrealistic When you are educating a patient make sure they understand, first week impairs learning, make sure family knows patient teaching as well. Smoking cessation is a big deal, moderation is the biggest thing you can teach them, tell them to stop if any of this occurs. HF used to be called CHF. S1 pulse correlates with radial pulse. Left (lung)pulmonic congestion, right systemic congestion. Afterload/preload can happen on R or L side but we focus on L. Be able to connect parts of RAAS system. Usually HF leads to kidney failure, affects GFR, you see urea & creatinine build up. Initially with decreased kidney and creatinine because the HF might be managed by diuretics, they may need hydration. BUN might be elevated, sometimes too much diaphoresis might cause increased creatinine & urea, may need fluid to help. WOB controlled by SNS, cyanosis(late sign), new activity intolerance is a significant finding. S3/S4=how stiff or lacks the ventricle are S3=”rushing in” (more blood had to enter to increase preload), remember location of heart sounds (All, Physicians, Take, Money). S4= ”a stiff wall” I&O nursing discretion, JVP assess on all pts, daily weights, abdominal girth, edema, mental status, GFR. Dig is a + inotrope with a narrow therapeutic index. Electrically K+/Na+ begins depolarization, when it contracts Ca+ enters the cell. If something happens to SA node(60-100) then it travels to AV node which fires at 40-60bmp, bundle of his even lower (30-40). Less than 60 you can have bradycardias sinus rhythm. Automaticity, excitability, conductivity, contractility, Cardiac monitor, a p-wave and t-wave should occur for each, you should be able to determine if intervals are too long it is a block(not tested on degrees of blocks), each block represents 0.04, larger 0.2. Be familiar with numbers, be able to identify intervals. A 12 lead EKG is needed, be able to pick out ST elevation, may lead to antithrombolitic like TNK. Know common dysthymias, you can have VT or Vfib, you’d know whats going on. Know the most common stuff (COPD, asthema), can you identify a HR by looking at a strip PVD know the difference between venous and arterial treatment of the big part. The nurse would assess a client with complaints of chest pain for which of the following clinical manifestations associated with a myocardial infarction (MI)? Nausea, vomiting, flushing, diaphoresis, S3 or S4 heart sounds. During the initial phase of an MI, there is reduced cerebral blood flow causing an increase in sympathetic nervous system (SNS) stimulation. This results in the release of catecholamines (norephinephrine in the adrenal medulla, epinephrine, dopamine) and also in the sweat glands, acetylcholine. The result will be the release of glycogen, diaphoresis (from sweat gland stimulation), and vasoconstriction of peripheral blood vessels. The client's skin may be ashen, cool, and clammy (not flushed) secondary to this response. Nausea and vomiting may result from reflex stimulation of the vomiting center by severe pain as well as from the direct effect of the sympathetic system on intestinal musculature. Ventricular dysfunction resulting from the MI may lead to the presence of the abnormal S3 and S4 heart sounds. 30. When computing a heart rate from the ECG tracing, the nurse counts 15 of the small blocks between the R waves of a client whose rhythm is regular. From these data, the nurse calculates the client's heart rate to be which of the following? 100 beats per minute Since each small block on the ECG paper represents 0.04 seconds, 1500 of these blocks represents 1 minute. By dividing the number of small blocks (15 in this case) into 1500, the nurse can calculate the heart rate in a client whose rhythm is regular (in this case 100). Which of the following statements best describes the electrical activity of the heart represented by measuring the PR interval on the ECG? Correct The length of time for the electrical impulse to travel from the SA node to the Purkinje fibres The length of time it takes to depolarize the atrium The length of time it takes for the electrical impulse to travel from the SA node to the AV node The length of time it takes for the atria to depolarize and repolarize The electrical impulse in the heart must travel from the SA node through the AV node and into the Purkinje fibres of the ventricle in order for synchronous atrial and ventricular contraction to occur. The P-wave represents atrial contraction and the R-wave is part of the QRS complex that represents ventricular contraction. Therefore when measuring the time from the beginning of the P-wave to the beginning of the QRS (PR interval), the nurse is identifying the length of time it takes for the electrical impulse to travel from the SA node to the Purkinje fibres of the ventricle. The nurse is watching the cardiac monitor, and a client's rhythm suddenly changes. There are no P-waves; instead there are wavy lines between the QRS complexes. The QRS complexes measure 0.08 seconds (narrow), but they occur irregularly with a rate of 120 beats per minute. The nurse correctly interprets that this rhythm is which of the following? Atrial fibrillation Sinus tachycardia Ventricular tachycardia Ventricular fibrillation Atrial fibrillation is represented on the cardiac monitor by irregular R-R intervals and small fibrillatory (f) waves. There are no normal P-waves because the atria are not truly contracting; they are just fibrillating. The nurse obtains a 6-second rhythm strip and charts the following analysis: Atrial rate 70 regular, Ventricular rate 40 regular, No relationship between P-waves and QRS complexes; atria and ventricles beating independently of each other, QRS 0.04 sec. Which of the following is a correct interpretation of this rhythm strip? Third-degree heart block Premature ventricular contractions Sinus dysrhythmias Wenckebach phenomenon Third-degree heart block represents a loss of communication between the atrium and ventricles. This is depicted on the rhythm strip as no relationship between the P waves, representing atrial contraction, and QRS complexes, representing ventricular contraction. The atria are beating totally on their own at 70 beats per minute, whereas the ventricles are pacing themselves at 40 beats per minute. A client is experiencing a heart rate of 200 beats/min. If the ECG pattern demonstrates absent P waves and normal and consistent QRS complexes and duration, the nurse should interpret these findings as indicative of which one of the following? Supraventricular tachycardia 1. Ventricular tachycardia 2. Second-degree heart block 4. Premature ventricular contraction Supraventricular tachycardia involves the rapid stimulation of atrial tissue; thus depolarization is stimulated above the ventricular conduction system and is using normal conduction pathways. P waves are obscured by the preceding T waves. Premature ventricular contractions are not associated with rapid heart rate as much as an independent irregular rhythm is with second-degree heart block. Ventricular tachycardia is a medical emergency that involves both left and right ventricles. A narrow pulse pressure, which is the difference between the systolic and diastolic, is an early indication of shock. Look for hypovolemia or decreased cardiac output. Often the systolic pressure will start to fall as cardiac output decreases. A patient who is hypovolemic, or a patient who has decreased cardiac output from an MI, will exhibit a decrease in the systolic pressure. The body’s compensatory mechanism and response to decreased cardiac output is to stimulate the sympathetic nervous system. This will cause vasoconstriction and result in a rise in the diastolic pressure causing a narrowed pulse pressure. Automaticity refers to the ability of cardiac cells to spontaneously and repetitively initiate an impulse. The initiation of an impulse in response to a stimulus refers to excitability. The transmission of electrical impulses that are received refers to the property of conductivity, and the response to a stimulus only after repolarization refers to refractoriness What should the nurse do if a client with heart failure is being treated with digoxin and has developed hypokalemia? Monitor the client for toxic effects that can occur at normal doses. 1. Administer digoxin twice daily. 2. Reduce the digoxin dose to every other day. 3. Administer an IV bolus of potassium. Digoxin exerts its effects by binding to the potassium receptor site (competing with potassium) on the myocardial membrane. When serum potassium levels are below normal, more potassium receptor sites are bound with digoxin, allowing it to exert a greater effect at the same dosage. Using a bolus of potassium is not indicated at this time. Which of the following test results identify that a client with an asthma attack is responding to treatment? A decreased exhaled nitric oxide. Nitric oxide levels are increased in the breath of people with asthma. A decrease in the exhaled nitric oxide concentration suggests that the treatment may be decreasing the lung inflammation associated with asthma. When admitting a client with the diagnosis of asthma exacerbation, the nurse will assess for which of the following potential triggers? Emotional stress Medications for asthmas? Nursing assessment findings of jugular vein distension and pedal edema would be indicative of which of the following complications of emphysema? Fluid volume excess secondary to cor pulmonale. Cor pulmonale is a right-sided heart failure caused by resistance to right ventricular outflow due to lung disease. With failure of the right ventricle, the blood emptying into the right atrium and ventricle would be slowed, leading to jugular venous distension and pedal edema. PR interval =0.12-0.20 sec QRS interval= 0.04-0.12 sec QT interval=<.042 sec tachycardia (>100) flutter (250-400) fibrillation (300-600) Ventricular dysrhythmias most commonly seen as a complication to MI. A Fib PVC VT Torsades de VF point (cardiac arrest) (Polymorphic VT) “Twisting of the points” atrial rate 300600 ventricular rate 120-200, both rhythms irregular no discernible P waves, rather see irregular fibrillatory or “f” waves PR interval cannot be measured many P waves : per 1 QRS No P wave widened, bizarre QRS complex in opposite direction of T wave concern only if x 3 =VT 3 or more PVCs in a row, rate>100 bpm pulseless and unresponsive, and therefore will require defibrillation lethal dysrhythmia A form of VT in which QRS complexes up & down, prolonged QT interval (>.40 sec.) no atrial activity or CO, on EKG see a bizarre, fibrillatory wave, no identifiable p wave, QRS complex, or T wave Atrial Fibrillation Periventricular Contractions Asystole no electrical, mechanical activity, heartbeat, pulse, or respiration initiate CPR IV, intracardiac, or endotracheal epinephrine Ventricular Tachycardia Ventricular Fibrillation Torsade de points (Polymorphic VT)