SpecNeeds.Test
advertisement
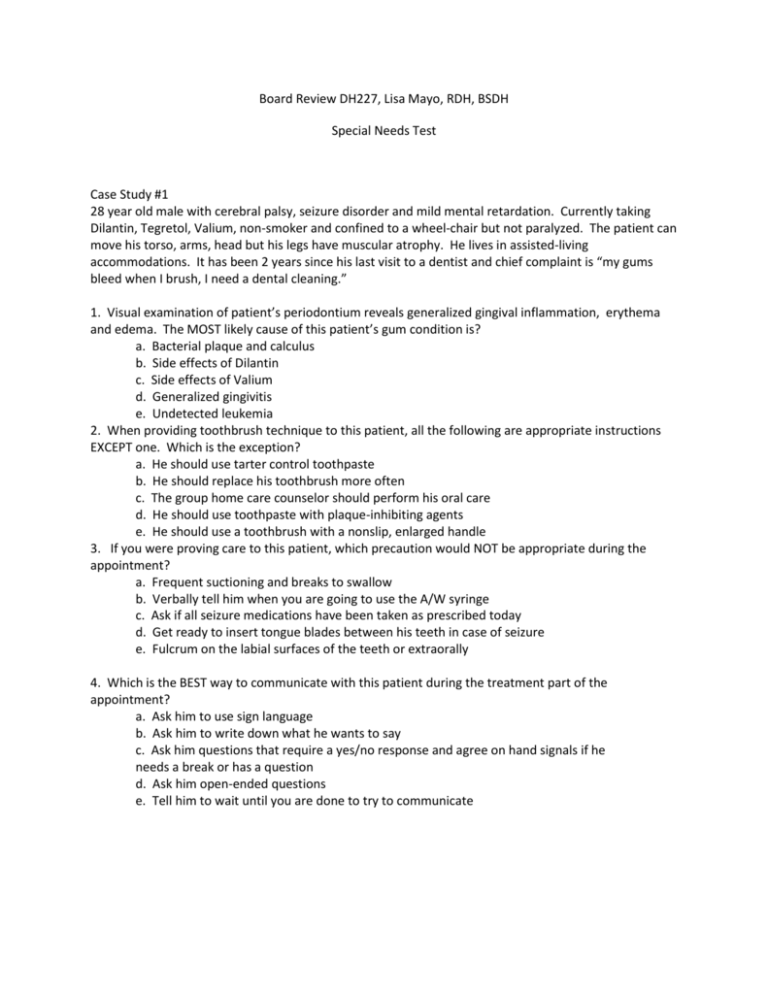
Board Review DH227, Lisa Mayo, RDH, BSDH Special Needs Test Case Study #1 28 year old male with cerebral palsy, seizure disorder and mild mental retardation. Currently taking Dilantin, Tegretol, Valium, non-smoker and confined to a wheel-chair but not paralyzed. The patient can move his torso, arms, head but his legs have muscular atrophy. He lives in assisted-living accommodations. It has been 2 years since his last visit to a dentist and chief complaint is “my gums bleed when I brush, I need a dental cleaning.” 1. Visual examination of patient’s periodontium reveals generalized gingival inflammation, erythema and edema. The MOST likely cause of this patient’s gum condition is? a. Bacterial plaque and calculus b. Side effects of Dilantin c. Side effects of Valium d. Generalized gingivitis e. Undetected leukemia 2. When providing toothbrush technique to this patient, all the following are appropriate instructions EXCEPT one. Which is the exception? a. He should use tarter control toothpaste b. He should replace his toothbrush more often c. The group home care counselor should perform his oral care d. He should use toothpaste with plaque-inhibiting agents e. He should use a toothbrush with a nonslip, enlarged handle 3. If you were proving care to this patient, which precaution would NOT be appropriate during the appointment? a. Frequent suctioning and breaks to swallow b. Verbally tell him when you are going to use the A/W syringe c. Ask if all seizure medications have been taken as prescribed today d. Get ready to insert tongue blades between his teeth in case of seizure e. Fulcrum on the labial surfaces of the teeth or extraorally 4. Which is the BEST way to communicate with this patient during the treatment part of the appointment? a. Ask him to use sign language b. Ask him to write down what he wants to say c. Ask him questions that require a yes/no response and agree on hand signals if he needs a break or has a question d. Ask him open-ended questions e. Tell him to wait until you are done to try to communicate 5. When providing health education, which is the BEST approach for his needs and abilities? a. Teach toothbrushing using a typodont b. Give him a pamphlet to take home c. Ask him to assess his progress after his teeth have been professionally cleaned by checking for blood on his toothbrush d. Ask him to assess his progress by checking the visual appearance of his gingiva e. Ask him to assess his progress by using a disclosing tablet 6. Which is the best radiographic option at his initial dental appointment? a. Panoramic b. 2 horizontal bitewings c. No radiographs d. Complete radiographic survey e. 4 regular bitewings 7. An office that would refer to schedule an appointment for this patient “because he has cerebral palsy” is demonstrating which of the following? a. A legal right of the practitioner based in the patient’s condition b. Discrimination according to the American with Disabilities Act c. Discrimination according to the Equal rights Amendment d. A personal preference that is not an instance of discrimination e. An uncommon reaction among primary care dentists in the USA Case Study #2 72 year old female with severe rheumatoid arthritis and Type II diabetes. Has had a hip replacement in the last 2 years. Uses a walker and is a smoker and takes motrin and metformin. She moved into a nursing home 2 years ago after her husband died. Her chief complaint is “I have toothaches in my jaw and I can’t hold my toothbrush very well. I cannot open my mouth very wide.” 1. The most likely cause of this patient jaw pain is: a. Dental abscess b. Periodontal abscess c. Arthritic involvement of the joints d. Bruxism e. Undetected multiple sclerosis 2. Any of the following factors may be affecting her need for insulin and therefore, aggravating her diabetes, EXCEPT for which one? a. Depression b. Food served at the nursing home c. Periodontal disease d. Restricted mobility e. Orofacial pain 3. All of the following could present problems in dental treatment planning EXCEPT for which one. a. Diabetes b. Limited oral opening c. Hip replacement d. Joint deformities in fingers and hands e. Inability of patient to walk on her own without a walker 4. Given this patients conditions, which radiographs would be the BEST option for her to determine her needs? a. Complete radiographic survey b. Selected periapicals c. 4 bitewings and selected periapicals d. Panoramic and 2 bitewings e. Panoramic alone 5. What is the BEST home care options for this patient? a. More frequent brushing using her current techniques b. Start flossing c. Antimicrobial rinses d. Purchase an electric toothbrush e. Use tarter control toothpaste 6. Which of the following conditions is NOT associated with diabetes? a. Cataracts b. Delayed healing c. Rapidly progressing periodontal disease d. Motor and sensory neuropathies e. Mucosal bleeding NON-CASE-BASED QUESTIONS 1. Individuals with all but one of the following conditions may be on a special diet. Which one is the EXCEPTION? a. cystic fibrosis b. End stage renal disease c. Diabetes d. Mild cardiac arrhythmia e. Congestive heart failure 2. Secondary hypertension is seen MOST often in which one of the following conditions? a. Cerebral palsy b. Kidney disease c. Viral hepatitis d. Parkinson disease e. Facioscapulohumoral muscular dystrophy 3. If a 200-pound patient arrived for an appointment in a wheelchair with his attendant, which of the following is NOT an option for performing a wheelchair transfer to the dental chair? a. Asking him if he can transfer with someone’s help b. Asking the attendant to transfer him c. Transferring him yourself using a one person transfer technique d. Ask the dental assistant or dentist to help perform a two person transfer technique e. Use a transfer board 4. All but one of the following may be a problems for an 85-yr old woman with a vision problem. Which one is the EXCEPTION? a. Glare from the dental light b. Heavy shag rug in the waiting room c. Changes in color between the tile floor and the carpet d. Raised door thresholds e. Signs on the receptionist’s desk 5. When taking a medical history about a seizure disorder, all the following are critical questions EXCEPT one. Which is the exception? a. What medications are you taking and did you take them today? b. Did you bring your medications to this appointment? c. What behaviors do you exhibit during a seizure? d. How long do the seizures last? e. Do you know when you’re going to have a seizure, ie: aura or sensations? 6. All the following may present problems with Alzheimer’s disease. Which one is LEAST likely to occur during toothbrushing? a. Doesn’t brush all areas of the mouth b. Cannot follow a recommended sequence c. Brushes for the amount of time that is set on an electric timer with a buzzer d. forgetting which is his toothbrush e. Wandering from the bathroom into the kitchen and putting the toothbrush in the fridge 7. Which of the following is NOT an important reason to identify risk factors for oral disease in each patient? a. To maximize positive health behaviors b. To eliminate or reduce risk factors c. To eliminate or stabilize oral disease caused by risk factors d. To prevent behaviors that may become risk factors e. To minimize positive health behaviors 8. Which of the following is a medical emergency? a. Acute adrenal insufficiency b. A bronchial asthma patient who is wheezing c. Tremors in an alcoholic d. Complete partial seizure e. Tremors in a patient with Parkinson’s 9. Which of the following g is NOT true about osteoporosis? a. It is common in postmenopausal females b. It is common in young women c. Women with reduced estrogen levels are at risk d. Osteoporosis is characterized by loss of bone density e. Women with osteoporosis experience more bone fractures 10. Chest pain is associated with all the following EXCEPT? a. Emphysema b. Angina c. Cardiac arrhythmia d. Hemophilia A e. Chronic obstructive pulmonary disease 11. A patient with severe hand arthritis and deformation of knuckles has poor oral hygiene. What would you suggest? a. Flossing instructions b. electric toothbrush c. Interproximal aids d. Use of mouthrinse e. Fluoride toothpaste 12. Medical conditions requiring special diets include all the following EXCEPT one. a. Diabetes b. Congestive heart failure c. Bradycardia d. Alcoholism e. Bulemia 13. Oral manifestations of sickle cell anemia include all the following EXCEPT one. a. Pallor of tissues b. Mucosal redness c. Hypoplastic enamel d. Delayed tooth eruption 14. Low blood pressure, extreme weakness, skin pigmentation, susceptibility to infections, and destruction of adrenocortical tissue are symptoms of a. DeQuervain’s disease b. Chron’s disease c. Cushing’s disease d. Addison’s disease e. Peutz-Jegher syndrome 15. The immunological indication that signifies a patient has AIDS is a. Suppression of humoral immunity b. Suppression of cellular immunity c. Loss of neutrophil production d. Loss on monocytes 16. All the following are characteristic traits of Sjogren’s syndrome except one. a. Coexists with Paget’s b. Dry eyes and mouth c. Joint pain d. Fatigue and lethargy e. Body attacks its moisture-laden glands 17. The AIDS virus attaches to which of the following cells? a. B-Lymphocytes b. Suppressor T-Lymphocytes c. Helper T-Lymphocytes d. Neutrophils e. Platelets 18. Radiation therapy such as brachytherapy or linear accelerator therapy can have serious side effects, the MOST serious of which is: a. Xerostomia b. Carious lesions c. Trismus d. Dysgeusia e. Osteoradionecrosis 19. A characteristic trait of von Recklinghausen’s disease is a. Café-au-lait macules b. Dwarfism c. Buffalo hump and moon face d. Hemorrhage 20. Polycythemia is a stem-cell disorder that over-produces RBC. All the following are symptoms of polycythemia except which one? a. Bleeding gingiva b. Epistaxis c. Active blood flow d. Thrombosis e. GI bleeds 21. Your patient constantly waves his hands in your op. He also reports that he brushes his teeth at least 10 times per day and flosses at least 4 times a day. This patient suffers from: a. Obsessive-compulsive disorder b. Panic attacks c. Psychotic disorder d. Anxiety disorder 22. Which of the following disorders is characterized by periods of active symptoms, then remission when toxins that damage nerve fibers and replace the myelin sheath with sclerotic tissues? a. Muscular dystrophy b. Multiple sclerosis c. Myasthenia gravis d. Parkinson’s disease 23. Which of the following special needs patients do NOT need to be premedicated with an antibiotic prior to dental treatment? a. Uncontrolled diabetes b. Spina bifida c. End-stage renal failure d. Inflammatory rheumatoid arthritis e. Mitral valve prolapse 24. A patient with pernicious anemia will suffer from all of the following symptoms EXCEPT which one? a. Glossitis b. Cheilosis c. Severe gingivitis d. Burning mucosa 25. Asperger syndrome occurs in individuals who seem of normal intelligence and communicate well with others, but suffer from a. AD/HD b. Alzheimer’s disease c. Autism d. Bipolar disorder e. Cerebral palsy 26. A patient with mild Alzheimer’s presented with high plaque levels and calculus. He lives in a nursing home, but is visited often by his family. What is the most important aspect of good home care for this patient? a. Chlorehexidine rinses b. Help with flossing technique c. Use of electric toothbrush d. Fluoride rinses e. Gearing the home-care instructions to the family members 27. Patients with visual impairments are often on topical medications, that contain a pharmaceutical which can be absorbed into the bloodstream. That medication is: a. Calcium channel blockers b. Beta blockers c. Depolarizing agents d. Adrenergic blockers e. Both adrenergic and beta blocking agents 28. If a patient has tight lips and skin and cannot open wide enough, he likely has: a. Bell’s palsy b. Scleroderma c. Trigeminal neuralgia d. Cystic fibrosis 29. Which of the following indicates a PRO in blood that mediates platelet cohesiveness when endothelium is injured? a. Stuart factor b. Thalassemia c. Von Willerbrand factor d. Prothrombin deficiency e. Agranulocytosis 30. Which of the following disorders is characterized by blinking, arm thrusting, kicking, shoulder-shrug, ging, twirling, sniffing, grunting and/or jumping? a. Anxiety disorder b. Brief psychotic disorder c. Post-traumatic stress disorder d. Tourette syndrome 31. Which of the following disorders features a “butterfly” on the bridge of the nose that can be raised, bright red, edematous though with time, the center becomes depressed as the color fades? a. Epidermis bullosa b. Pemphigoid c. Lupus erythematosus d. Pemphigus e. Behcet’s syndrome 32. All the following are symptoms of myasthenia gravis EXCEPT which one. a. Slurred speech with nasal tones b. Difficulty in breathing c. Difficulty swallowing food d. Drooling e. Steady gait 33. When planning oral health care education for a geriatric patient, which of the following is the MOST important consideration? a. Insurance b. Income level c. Functional ability d. Number of existing teeth 34. Which of the following is NOT a symptom of cocaine abuse? a. Bradycardia b. Hypertension c. Dilated pupils d. Cardiac arrhythmias 35. Which of the following is a treatment consideration for a patient with Alzheimer’s? a. Premedicate b. Do not provide oral health education c. Schedule long appointments to eliminate number of visits’ d. Schedule short appointments due to problems with corporation 36. Which of the following would indicate a contraindication for nitrous oxide/oxygen sedation? a. Asthma b. Emphysema c. Hypertension d. Myocardial infarction 37. If you next patient is a child with Autism, you should: a. Premedicate b. Scheduling long appointments c. Schedule short, frequent appointments d. Explain the purpose of everything you do 38. A 75 year old patient who is suffering from dehydration may give the appearance of: a. Dementia b. Pneumonia c. Bell’s palsy d. Basal cell carcinoma 39. Clara is a 75 year old mentally retarded female. She resides in a long-term care facility. Her mother, who has Alzheimer’s, resides in the same facility. Clara’s cousin visits on a regular basis. Oral health care instructions for Clara should be: a. Provided to her mother b. Provided to the cousin c. Provided to Clara in writing d. Oral care instructions would not be beneficial 40. Which of the following medical conditions does not progressively get worse? a. Xerostomia b. Cerebral palsy c. Parkinsons d. Basal cell carcinoma 41. Which of the following is NOT a disease? a. Hepatitis b. Cerebral palsy c. Parkinsons d. Lupus erythematous 42. Your patient has an angina attack in the middle of your recall appointment. Order the steps for the procedure to follow a. Call 911 b. Wait 5 minutes and dissolve nitroglycerine tablet under the tongue c. Have the patient dissolve a nitroglycerine under the tongue d. After 10min have the patient have the patient dissolve a nitroglycerine tablet under the tongue 43. You have a patient who has experiences spinal cord damage at C-5. What implications would this have for oral care? a. The patient would need to use a floss holder b. The patient would need to use an electric toothbrush c. The patient would have to have oral care by a caregiver d. The patient would need a modified handle for the toothbrush 44. Mr. Smith is 90 years old and wears a hearing aid. Which of the following will be important when communicating with Mr.Smith? a. Speak as loud as you can b. Speak slowly and ennunicate c. Don’t communicate with him d. Communicate only with his spouse 45. You are providing care to Danny, a child with ADHD. Which of the following is NOT a good idea during patient treatment? a. Tell,show,do b. Give the child several breaks c. Have the child hold the suction d. Maintain eye contact during the appointment 46. Which of the following could you expect to observe with fetal alcohol syndrome? a. Gingivitis b. Abnormal tooth eruption c. Decreased mental ability d. All the above 47. You have a patient with Chronic Renal Failure. When should you schedule their appointment? a. The day after dialysis b. In the afternoon right after dialysis c. In the morning right after dialysis 48. Which of the following is NOT true of scoliosis? a. Cause is idiopathic b. There is a genetic link c. There is no treatment for the condition d. Treatment should be started when you are very young 49. Which of the following is appropriate for management of pediatric patients? a. Control through restraints b. Use age appropriate terms c. Have the mother give directions d. Always give nitrous oxide sedation 50. Which of the following is contraindicated for a recovering alcoholic? a. Epinephrine b. Local anesthesia c. Three month recall d. Nitrous oxide/oxygen sedation 51. Which of the following 2 items are not symptoms of Down’s syndrome? a. Xerostomia b. Increased caries c. Flat facial profile d. Decreased resistance to infection 52. Which of the following is NOT a symptom of Parkinson’s disease? a. Drooling b. Unblinking eyes c. Difficulty swallowing d. Slow and shuffling gait 53. Which is NOT a symptom of congestive heart failure? a. Blue bloater b. Difficulty breathing c. Swelling in the extremities d. Nausea from the medication 54. Which of the following conditions is associated with the Buffalo Hump? a. Hyperthyroidism b. Hypothyroidism c. Addison’s disease d. Cushing’s syndrome 55. Your patient has Addison’s disease. Which of the following is an oral manifestation you would expect to observe? a. Herpes b. Candida c. Hemangioma d. Pigmented gingiva 56. You have finished providing preventive oral care to a 90 year old man. Which of the following is your number one responsibility? a. Speak slowly b. Involve a caregiver c. Assess the patient’s ability to understand d. Determine how the treatment will influence their active life 57. Which of the following is NOT a condition associated with scleroderma? a. Xerostomia b. Raynaud’s phenomenon c. Tightening of the skin and lips d. Narrowing of the periodontal ligament space 58. Your next patient has seizures 2-3 times per week. Which of the following occurs prior to the seizure? a. An aura b. Difficulty breathing c. Sharp pain in the left arm d. Swelling of the extremities 59. Your patient has Hep B. What treatment modifications would you make? a. Double glove b. Universal precautions c. Sterilize instruments wisely d. Appoint at the end of the day 60. Which of the following oral conditions are manifested in TB? a. Herpes b. Candidiasis c. Hemangioma d. Ulcerative lesion of the mucosa 61. Match the following symptoms to the condition with which they are associated. 1.Dilated pupils a. Heroin addict 2.Kaposi’s Sarcoma b. Parkinson’s disease 3.Goiter c. Addison’s disease 4.Pin point pupils d. Cocaine addict 5.Nonblinking eyes e. HIV/AIDS 6.Bronzing f. Grave’s disease 62. Which of the following 3 items are symptoms of insulin shock? a. Fruity smelling breath b. Hypoglycemia c. Weakness d. Sweating e. Lowered heart rate 63. There is a vaccine for which 2 of the following? a. Hep A b. Hep B c. Hep C d. Hep D e. Hep E 64. Which of the following 3 procedures would be appropriate for a person with a motor disability: a. Wider doorways b. Automatic opening doors c. Rounded metallic door knobs d. Non-skid flooring material 65. Identify the location to take the pulse of a conscious adult a. Radial pulse b. Popiteal pulse c. Femoral pulse d. Abdominal pulse 66. Your patient has a BP 166/100mmHg. This sage of hypertension would be classified as: a. Normal b. Mild c. Moderate d. Severe 67. The course of action to take for the patient in the previous question would be: a. Delay all dental tx until BP readings are consistent b. Re-check pressure in 5 min and consult the patients physician c. Observe the patient during dental tx and re-eval at 6mo recare d. Immediate referral to the ER 68. Identify 4 clinical manifestations of a patient experiencing insulin shock: a. Sudden headache b. Tachycardia c. Sweating d. Polyuria e. Blurred vision f. Drowsiness g. Decreased pulse rate 69. Your patient is a 70 year old man who has smoked all his adult life. Tooth #19 was recently extracted Identify a reason why an implant would NOT be a good choice for this patient: a. He is an older patient b. He is a smoker c. He should not experience teeth drifting ay this age d. Healing is much slower after age 70 70. Which of the following appointment modifications would be appropriate for a blind patient: a. Speaking louder than normal b. Removing your mask to speak c. Allowing the seeing eye dog into the treatment room d. Explaining every procedure in detail 71. What oral physiotherapy aid is recommended for a patient with Parkinson’s disease: a. Oral irrigator b. Electric toothbrush c. Daily flossing d. Stimudent 72. Your patient is hypertensive, which of the following should NOT be used: a. Ultrasonic scaler b. Air polisher c. Rubber cup polisher d. Oral irrigator 73. Identify the therapeutic effect of nitroglycerine: a. Increases heart rate b. Constricts capillaries c. Relaxes smooth vascular tissue d. Opens the valves of the heart 74. Which of the following is contraindicated for a patient with asthma: a. Aspirin b. Prednisone c. Medical inhaler d. Nitrous oxide, oxygen sedation 75. Identify a symptom of congestive heart failure: a. High blood pressure b. High cholesterol c. Edema d. Bradykinesia 76. Which of the following is not contagious: a. Cerebral palsy b. Hepatitis c. Tuberculosis d. Legionnaire’s disease 77. Your patient has a spinal cord injury at level C-4, how would you instruct the patient to brush: a. Modified toothbrush handle b. Electric toothbrush c. Caregiver would brush teeth d. None of the above 78. Identify a procedure used when treating HIV/AIDS patients: a. Double glove b. Disposable barriers c. Appoint as the last patient of the day d. Sterilize instruments then clean in ultrasonic and sterilize again 79. Identify 2 symptoms that are associated with emphysema: a. High BP b. Difficulty breathing c. Chronic coughing d. Weight gain e. Hyperthermia 80. Which of the following is related to the potential for myocardial infarction? a. Low blood pressure b. History of ischemia c. Asthma d. None of the above 81. Which cell in the immune system is changed, replicated and destroyed in HIV/AIDS? a. T-4 (T-helper lymphocytes) b. T-8(T-supressor lymphocytes) c. HTLV-III d. Retrovirus 82. Your patient has a spinal cord injury, what would be the most common interference of dental hygiene care? a. Uncooperation b. Inability to give informed consent c. Spasticity of the patient d. None of the above 83. Which of the following devises would you recommend for an arthritis patient? a. Flossing instruction b. Oral irrigator c. Manual toothbrush d. Electric toothbrush 84. Your patient has been diagnosed with hypertension and arthritis. As you are putting the chair back, you also notice swollen ankles. What other diseases is this patient experiencing? a. Myocardial infarction b. Angina pectoris c. Congestive heart failure ANSWERS CASE #1 1. 2. 3. 4. 5. 6. 7. ANSWERS CASE #2 A C D C C A B 1. 2. 3. 4. 5. 6. B B E E C E NON-CASE-BASED QUESTIONS 1.D 2.B 3.C 4.C 5.B 6.C 7.E 8.A 9.B 10.D 11.D 12.C 13.B 14.D 15.B 16.A 17.C 18.E 19.A 20.C 21.A 22.B 23.E 24.C 25.C 26.E 27.B 28.B 29.C 30.D 31.C 32.E 33.C 34.A 35.D 36.B 37.C 38.A 39.B 40.B 41.B 42.C,B,D,A 43.C 44.B 45.B 46.D 47.A 48.C 49.B 50.D 51.A,B 52.C 53.A 54.D 55.D 56.D 57.D 58.A 59.B 60.D 61.D,E,F,A,B,C 62.B,C,D 63.A,B 64.A,B,D 65.A 66.C 67.B 68.A,B,C,E 69.B 70.C 71.B 72.B 73.C 74.A 75.C 76.A 77.C 78.B 79.B,C 80.B 81.A 82.C 83.D 84.C 85.