Conservative Spine and Joint Center Ruben Diaz, MD
advertisement
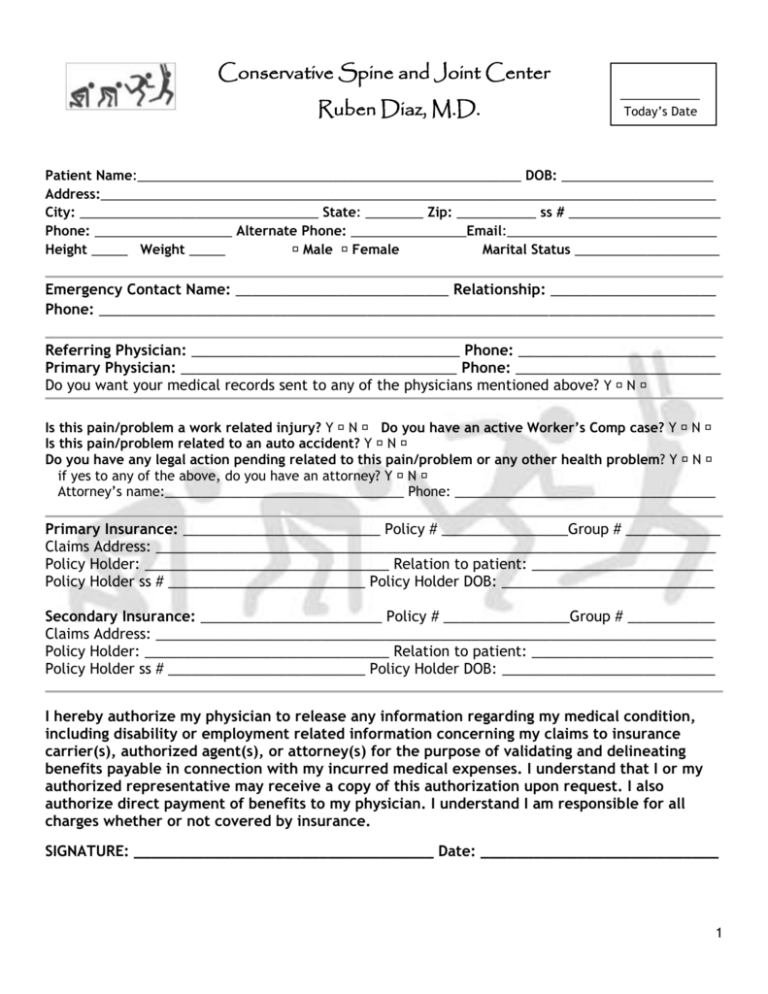
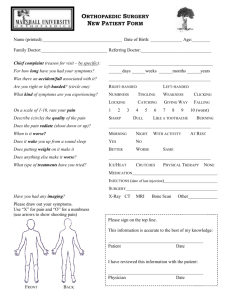
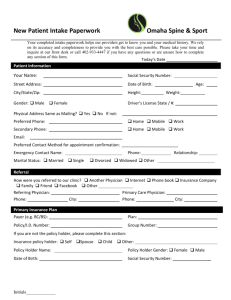
Conservative Spine and Joint Center Ruben Diaz, M.D. ___________ Today’s Date Patient Name:_____________________________________________________ DOB: _____________________ Address:_____________________________________________________________________________________ City: _________________________________ State: ________ Zip: ___________ ss # _____________________ Phone: ___________________ Alternate Phone: ________________Email:_____________________________ Height _____ Weight _____ � Male � Female Marital Status ____________________ Emergency Contact Name: ___________________________ Relationship: _____________________ Phone: ______________________________________________________________________________ Referring Physician: __________________________________ Phone: _________________________ Primary Physician: ___________________________________ Phone: __________________________ Do you want your medical records sent to any of the physicians mentioned above? Y � N � Is this pain/problem a work related injury? Y � N � Do you have an active Worker’s Comp case? Y � N � Is this pain/problem related to an auto accident? Y � N � Do you have any legal action pending related to this pain/problem or any other health problem? Y � N � if yes to any of the above, do you have an attorney? Y � N � Attorney’s name:_________________________________ Phone: ____________________________________ Primary Insurance: _________________________ Policy # ________________Group # ____________ Claims Address: _______________________________________________________________________ Policy Holder: _______________________________ Relation to patient: _______________________ Policy Holder ss # _________________________ Policy Holder DOB: ___________________________ Secondary Insurance: _______________________ Policy # ________________Group # ___________ Claims Address: _______________________________________________________________________ Policy Holder: _______________________________ Relation to patient: _______________________ Policy Holder ss # _________________________ Policy Holder DOB: ___________________________ I hereby authorize my physician to release any information regarding my medical condition, including disability or employment related information concerning my claims to insurance carrier(s), authorized agent(s), or attorney(s) for the purpose of validating and delineating benefits payable in connection with my incurred medical expenses. I understand that I or my authorized representative may receive a copy of this authorization upon request. I also authorize direct payment of benefits to my physician. I understand I am responsible for all charges whether or not covered by insurance. SIGNATURE: __________________________________ Date: ___________________________ 1 Patient Name:_________________________ PRESENT COMPLAINT: Date of injury/Accident/Onset of problem: _________________________ Describe in your own words the pain/problem(s) you would like help with: __________________________ _____________________________________________________________________________________________ Where is your problem located? � Neck � Upper Back � Lower Back � Arm (rt/lft) �Hip �Leg(rt/lft) Circle Pain level TODAY: 0=none 10=worst 0 1 2 3 4 5 6 7 8 9 10 Is the pain? (Circle all that apply): Sharp Dull Stabbing Aching Burning Stiffness Throbbing “Electrical” shooting pain Tingling Pins & needles sensations Is the pain? (Circle one): Constant comes & goes Mention all things that make the pain better: ____________________________________________________ Mention all things that make the pain worst: ____________________________________________________ Have you had any previous treatments (i.e. medications, therapy, injections, surgery) for this pain/problem? If yes, list them all here___________________________________________________________ _____________________________________________________________________________________________ Tests you have had: (circle all that apply): x-ray CT Scan MRI EMG/NCS DEXA Myelogram Discogram Other:_________________ Pain Drawing: (Please mark these drawings according to area(s) that hurt): 2 RIGHT LEFT RIGHT Patient Name:_________________________ OCCUPATIONAL HISTORY: Current work status: �Working full time �Student �Working restricted duty (since ________) �Disabled �Homemaker �Unemployed �Retired Occupation:_______________________________ Employer: _________________________________ Have you missed any time for work due to this pain/problem? Y � N � When? ___________________ Have you had neck pain/arm numbness/arm weakness before this episode? Y � N � When? ____________ Have you had back pain/leg numbness/leg weakness before this episode? Y � N � When? ______________ PAST MEDICAL HISTORY: (Please check below if you have, or have had, any of these medical condition)s: � NO PAST MEDICAL PROBLEMS � Acid reflux � Adverse reaction to anesthesia Type of Reaction:____________ � Alzheimer’s or significant memory loss � Anemia � Angina or chest pain � Asthma � � � � � � � � Coronary artery disease Dental disease Depression Diabetes Emphysema Epilepsy/Seizures Fibromyalgia Gout � � � � � � � � Kidney disease Osteoarthritis Osteoporosis Pneumonia Psychiatric disorder Rheumatoid arthritis Sickle cell Sleep apnea 3 � � � � Artrial fibrillation or erratic heartbeat Bladder problems Bleeding ulcers Blood clot � Legs � Lungs � Cancer Type:_________________ � Congestive heart failure � � � � � � Hemophilia/Excessive bleeding � CPAP machine Hepatitis � Stroke (CVA) High blood pressure/Hypertension � Thyroid disease High cholesterol � Other not listed, explain: HIV or AIDS _______________________ Infections:_______________ _______________________ MRSA? � Yes � No SURGICAL HISTORY: (Please check below if you have had any of these surgeries): � NO PREVIOUS SURGERY � Abdominal surgery Type of surgery:_________ � Aneurysm � Angioplasty/Stents � Artery bypass of arm or leg � Bone /Joint surgery Type of surgery:___________ �Carotid surgery � Spine Surgery (circle one) cervical, thoracic, lumbar Date: _______________ � Cervical spine surgery � Colon surgery � Coronary bypass (CABG) � Gastric bypass surgery � Heart valve replacement � � � � � Hysterectomy Lumbar spine surgery Pacemaker/Defibrillator Prostate surgery Breast surgery Type of surgery:________ �Other not listed, explain: ______________________ FAMILY HISTORY: (Please check below if any of your immediate relatives have had any of the following): � � � � � � NO FAMILY MEDICAL HISTORY TO REPORT Adopted � Yes � No � Cancer Adverse reaction to anesthesia � Osteoarthritis Depression � Bleeding disorders Heart disease � Stroke Blood clots/Pulmonary embolism � Other not listed, explain: � Hypertension � Diabetes � Osteoporosis � Rheumatoid arthritis ________________________ Patient Name:_________________________ SOCIAL HISTORY: Marital Status: � Single � Married � Partner � Divorced � Widow/Widower Hobbies _____________________________________________________________________________________ Smoking: � Never smoked � Former smoker � Current smoker How many packs/day? ___________ Do you dip or chew tobacco? Y � N � If Yes, how much per day? ____________________________________ Do you drink alcoholic beverages? Y � N � If Yes, how many drinks per week? _________________________ Have you ever had a problem with drug dependence or illicit drug use? Y � N � If Yes, please explain: _____________________________________________________________________________________________ REVIEW OF SYSTEMS: (Please circle below if you have any of these symptoms- also, give a brief description.): 1. 2. 3. 4. 5. 6. 7. 8. Constitutional: fever, recent weight gain/loss, appetite problems __________________________________ Eyes: double vision, blurring, difficulty seeing ___________________________________________________ Ears, Nose, Mouth, Throat: deafness, sinusitis, hoarseness, dizziness _______________________________ Cardiovascular: chest pain, palpitations, murmur, extra beats _____________________________________ Respiratory: shortness of breath, wheezing, cough, bloody cough __________________________________ Gastrointestinal: abdominal pain, constipation, diarrhea, rectal bleeding ___________________________ Urologic: pain with urinating, hesitant urination, bleeding, incontinence ____________________________ Gynecologic: breast masses, pain, discharge_____________________________________________________ 4 *Are you sexually active? Y � N � *Birth control used: __________ *Any chance you could be pregnant? Y � N 9. Skin: persistent rashes or lesions, changes in moles ______________________________________________ 10. Neurologic: seizures, loss of balance/coordination, weakness, memory loss_________________________ 11. Psychiatric: depression, anxiety, hallucinations, sleep disturbances _______________________________ 12. Endocrine: excessive thirst, excessive urination, heat/cold intolerance ____________________________ 13. Blood & Lymphatic: anemia, bleeding tendencies, swollen nodes _________________________________ 14. Allergic and Immunologic: hives, eczema, persistent itching _____________________________________ 15. Musculoskeletal: stiffness, joint pain/deformity, muscle wasting, spine pain radiating to arms or legs numbness/tingling _____________________________________________________________________________ 16. Other problems not covered above: _______________________________________________________________ CURRENT MEDICATIONS DOSE 1. 2. 3. 4. 5. 6. 7. ALLERGIES REACTION 1. 2. 3. 4. 5. Are you allergic to latex? � Yes � No If so what is the allergy?__________________________________ Patient signature: ___________________________________ Date: _____________ 5