EPOR Mutation Detection by Sequencing
advertisement
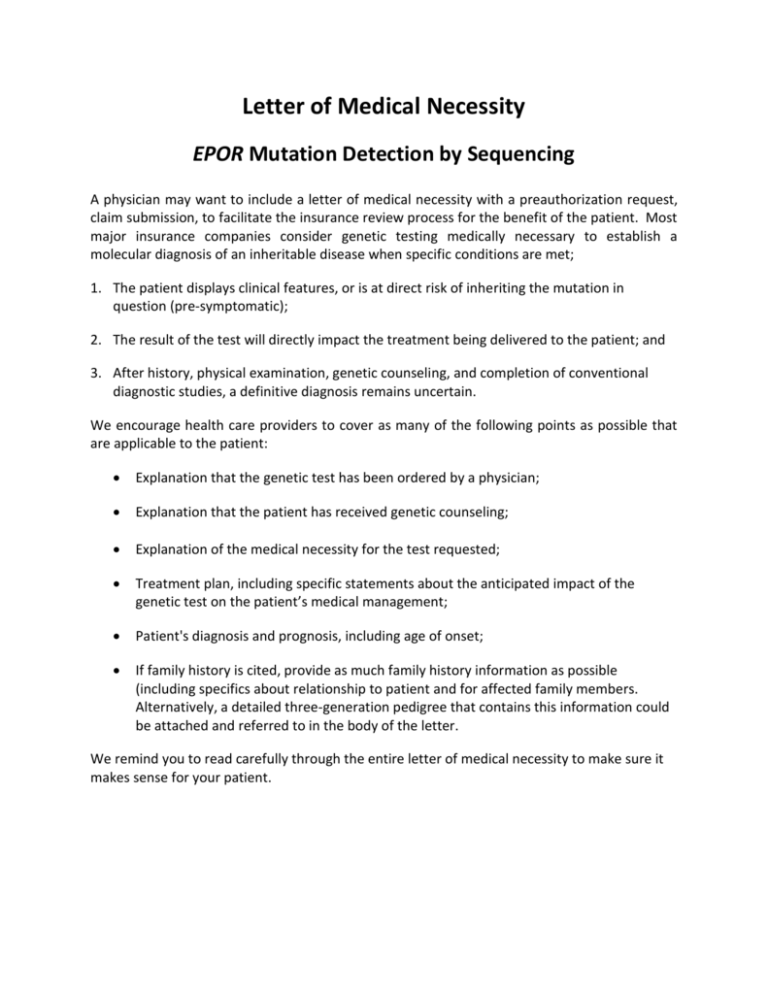
Letter of Medical Necessity EPOR Mutation Detection by Sequencing A physician may want to include a letter of medical necessity with a preauthorization request, claim submission, to facilitate the insurance review process for the benefit of the patient. Most major insurance companies consider genetic testing medically necessary to establish a molecular diagnosis of an inheritable disease when specific conditions are met; 1. The patient displays clinical features, or is at direct risk of inheriting the mutation in question (pre-symptomatic); 2. The result of the test will directly impact the treatment being delivered to the patient; and 3. After history, physical examination, genetic counseling, and completion of conventional diagnostic studies, a definitive diagnosis remains uncertain. We encourage health care providers to cover as many of the following points as possible that are applicable to the patient: Explanation that the genetic test has been ordered by a physician; Explanation that the patient has received genetic counseling; Explanation of the medical necessity for the test requested; Treatment plan, including specific statements about the anticipated impact of the genetic test on the patient’s medical management; Patient's diagnosis and prognosis, including age of onset; If family history is cited, provide as much family history information as possible (including specifics about relationship to patient and for affected family members. Alternatively, a detailed three-generation pedigree that contains this information could be attached and referred to in the body of the letter. We remind you to read carefully through the entire letter of medical necessity to make sure it makes sense for your patient. <On Office Letterhead> <Date> <Insurance Company Name> <Medical Director>, MD <Address 1> <Address 2> <City>, <ST> <ZIP> Re: <Patient Full Name> Member ID: <Enter Member ID> DOB: <MM/DD/YYYY> Group ID: <Enter Group ID> Dear Medical Director: I am writing this letter on behalf of my patient, <Patient Name>, to request coverage for the Erythropoietin Receptor Protein (EPOR) Mutation Detection by Sequencing test. This test is important to confirm a diagnosis of primary familial or congenital polycythemia (PFCP), distinguish inherited polycythemia from acquired polycythemia (eg, polycythemia vera), or to test at-risk relatives for a known familial EPOR mutation. PFCP is due to an autosomal dominant trait and does not necessarily carry an adverse prognosis in early life and most patients have a benign clinical course, but PFCP is associated with an increased risk of thrombotic and vascular mortality in later life. Polycythemia vera (PV), also known as polycythemia rubra vera, is a chronic clonal myleoproliferative disorder characterized by clonal proliferation of myeloid cells. The erythropoietin receptor protein is a cytokine receptor protein which upon binding erythropoietin ligand results in a cascade of signaling events within erythrocytes and other tissues that leads to proliferation and differentiation. The mutations in EPOR gene result in a truncated cytoplasmic domain of the protein that leads to ligand independent activation of the signaling pathways regulating RBC production. PFCP is a benign condition that should be ruled out when considering the diagnosis of PV. EPOR is on located on chromosome 19 encoding a single transcript NM_000121.3. The mutations in exons 7 and 8 that principally result in PFCP are deletion, insertion and point mutations that lead to cytoplasmic domain (C-terminus) truncation up to 70 amino acids. Each amplicon is bi-directionally sequenced. Exons 7 and 8 are in close proximity to each other. Exon 7 is 87 nucleotides in length with a 93 nucleotides intron between it and exon 8. Exon 8 is fairly large consisting of 612 coding nucleotides and 424 non-coding nucleotides. Amplification strategy divides the region into two targets, dividing exon 8 in two parts. The amplified fragments overlap by 90 nucleotides. I am requesting this test for <Patient Name>. This letter documents the medical necessity of this test to assist in the treatment, prognosis and diagnosis of <his/her> primary familial or congenital polycythemia (PFCP). Below is additional information about the patient’s medical history and potential impact of the test resulted for the patient’s medical management. Patient History and Diagnosis: <Patient Name> is a <Age> -year-old <Gender > with a diagnosis of possible primary familial or congenital polycythemia (PFCP), based on the following symptoms and clinical findings: 1. <Symptom/Diagnosis #1 with ICD-9 code> 2. <Symptom/Diagnosis #2 with ICD-9 code> Family History: (if applicable) <Patient Name> also has a family history, including: <Family History> Clinical Impression: The patient’s symptoms and clinical history, in addition to other diagnostic testing is suggestive of primary familial or congenital polycythemia (PFCP). The “EPOR Mutation Detection by Sequencing” test will play an important role in establishing the presence of specific mutations which will guide appropriate medical management of the patient. This test can assist the patient by: Confirmation of primary familial or congenital polycythemia, and rule out polycythemia vera a chronic clonal myleoproliferative disorder, predict clinical behavior of disease, aid in treatment decisions. I recommend that you support this request for coverage of the EPOR Mutation Detection by Sequencing testing for <Patient Name> through ARUP Laboratories test code 2007914, Federal Tax ID# 87-0403206 / NPI# 1376548271 with the following CPT codes 81479, G0452. Please note that this test is performed for clinical management in a laboratory that is CLIA approved for high complexity testing. Please feel free to contact me at <Physician Phone> if you require additional information. Sincerely, <Signature> <Print Name> References 1. [Guideline] Tefferi A, Thiele J, Orazi A, Kvasnicka HM, Barbui T, Hanson CA. Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood. Aug 15 2007;110(4):1092-7. 2. Kralovics R, Indrak K, Stopka T, Berman BW, Prchal JF, Prchal JT. Two new receptor mutations: Truncated EPO receptors are most frequently associated with primary familial and congenital polycythemias. Blood., 90, 1997 pp. 2057‐2061. 3. Arcasoy MO, Karayal AF, Segal HM, Sinning JG, Forget BG. A novel mutation in the erythropoietin receptor gene is associated with familial erythrocytosis. Blood. , 99, 2002, pp. 3066‐3069. 4. Sherry ST, Ward MH, Kholodov M, Baker J, Phan L, Smigielski EM, Sirotkin K. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. 2001 Jan 1;29(1):308‐11. http://www.ncbi.nlm.nih.gov/projects/SNP/ 5. A.A. Komar (ed.), Single Nucleotide Polymorphisms, Methods in Molecular Biology 578, pp95‐111; Humana Press, a part of Springer Science+Business Media, LLC 2003, 2009 6. Streiff MB, Smith B, Spivak JL. The diagnosis and management of polycythemia vera in the era since the Polycythemia Vera Study Group: a survey of American Society of Hematology members' practice patterns. Blood. Feb 15 2002;99(4):1144-9. 7. Adamson JW, Fialkow PJ, Murphy S, et al. Polycythemia vera: stem-cell and probable clonal origin of the disease. New England Journal of Medicine. 1976;295:913-916. 8. Perrotta S, Cucciolla V, Ferraro M, Ronzoni L, Tramontano A, Rossi F, et al. EPO receptor gain-of-function causes hereditary polycythemia, alters CD34 cell differentiation and increases circulating endothelial precursors. PLoS One. Aug 5 2010;5(8):e12015 9. Kralovics R, Prchal JT. Congenital and inherited polycythemia. Curr Opin Pediatr. Feb 2000;12(1):29-34 10. Tefferi A, Vardiman JW. Classification and diagnosis of myeloproliferative neoplasms: the 2008 World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia. Jan 2008;22(1):14-22 11. Winkelmann JC, Penny, LA, Deaven LL, Forget, BG, Jenkins RB. The gene for the human erythropoietin receptor: analysis of the coding sequence and assignment to chromosome 19p. Blood 1990;76:24-30. 12. Arcasoy MO, Karayal AF, Segal HM, Sinning JG, Forget BG. A novel mutation in the erythropoietin receptor gene is associated with familial erythrocytosis. Blood 2002;99:30669