Surveillance Audit Scope (For Non Aged Care Services)
advertisement
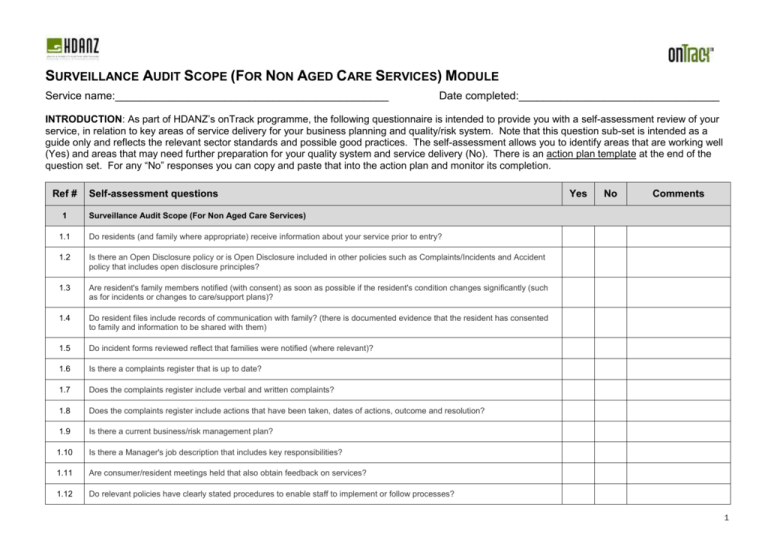
SURVEILLANCE AUDIT SCOPE (FOR NON AGED CARE SERVICES) MODULE Service name:_____________________________________________ Date completed:_________________________________ INTRODUCTION: As part of HDANZ’s onTrack programme, the following questionnaire is intended to provide you with a self-assessment review of your service, in relation to key areas of service delivery for your business planning and quality/risk system. Note that this question sub-set is intended as a guide only and reflects the relevant sector standards and possible good practices. The self-assessment allows you to identify areas that are working well (Yes) and areas that may need further preparation for your quality system and service delivery (No). There is an action plan template at the end of the question set. For any “No” responses you can copy and paste that into the action plan and monitor its completion. Ref # 1 Self-assessment questions Yes No Comments Surveillance Audit Scope (For Non Aged Care Services) 1.1 Do residents (and family where appropriate) receive information about your service prior to entry? 1.2 Is there an Open Disclosure policy or is Open Disclosure included in other policies such as Complaints/Incidents and Accident policy that includes open disclosure principles? 1.3 Are resident's family members notified (with consent) as soon as possible if the resident's condition changes significantly (such as for incidents or changes to care/support plans)? 1.4 Do resident files include records of communication with family? (there is documented evidence that the resident has consented to family and information to be shared with them) 1.5 Do incident forms reviewed reflect that families were notified (where relevant)? 1.6 Is there a complaints register that is up to date? 1.7 Does the complaints register include verbal and written complaints? 1.8 Does the complaints register include actions that have been taken, dates of actions, outcome and resolution? 1.9 Is there a current business/risk management plan? 1.10 Is there a Manager's job description that includes key responsibilities? 1.11 Are consumer/resident meetings held that also obtain feedback on services? 1.12 Do relevant policies have clearly stated procedures to enable staff to implement or follow processes? 1 1.13 Are your policies and procedures dated, approved, indexed and formatted into relevant manual(s) (hard copy or electronic)? 1.14 Are policy and procedure manuals easily accessible by staff and do they reflect current good practice? 1.15 Is there evidence of policy and procedure review? 1.16 Do you have a system for informing staff of any update/changes to policy and procedures? 1.17 Is there a Document Control policy that describes the management and review of policies/procedures? 1.18 Are there adequate clinical policies and procedures related to care provided? 1.19 Have the following been entered into the quality management system: 1. Incidents and accidents reported in resident files, 2. Infections reported/recorded have been entered into infection control monitoring/surveillance system, 3. Complaints (documented in progress notes/communication records or complaints form), 4. Satisfaction surveys, 5. Internal audits, 6. Hazards identified through incidents, accidents, inspection or maintenance have been transferred to the hazard register, and 7. Restraint interventions (if any)? 1.20 Are the results of data gathering communicated to staff and others such as the board of governance (e.g. results of internal audits, incidents and accidents, complaints, satisfaction surveys, infections)? 1.21 Is internal monitoring information collected and used to identify improvement actions and have these been signed off when completed? 1.22 Are there regular staff and management meetings that monitor the quality/risk system? 1.23 Is there a quality plan that includes specific goals that the performance of the service is measured against? 1.24 Do management and staff participate in the service quality and risk management system and does the service enable consumer participation wherever appropriate? 1.25 Is an action plan developed in response to data analysis and other internal monitoring such as internal audits, etc? 1.26 Do the action plans include the changes that need to be made, who by, within what time frames and how these will be monitored and further verified that the actions have been successful? 1.27 Is there a risk plan that identifies risks to the service and how these can be eliminated, isolated or minimised (note: this is more than a hazard analysis)? 1.28 Is there implementation of actions required to address actual and potential risks e.g. security, fire drills, education of staff? 1.29 Are health and safety procedures in place and overseen by a designated health and safety officer? 1.30 Are incidents and accidents analysed and on the basis of this analysis are actions taken to limit future occurrences of incidents or accidents? 2 1.31 Is there a current and update schedule (plan) for staff training and development? 1.32 Is content and attendance documented for staff training/professional development activities? 1.33 Does your training include a system to ensure that staff who miss a scheduled session receive the training and this is documented? 1.34 Is there is a documented rationale for how the service is staffed and this includes a description of how the number of staff is determined? 1.35 Does your roster reflect staff consistent with the documented staffing levels policy? 1.36 Does a suitably qualified/skilled or experienced staff member complete the assessment, planning, provision, evaluation and exit process with residents/ consumers? 1.37 Does a suitably qualified/skilled or experienced staff member complete an assessment of the resident and develop the individual care/support plans? 1.38 Is the suitably qualified staff member involved in re-assessment when the residents condition changes? 1.39 Do records demonstrate that residents and/or family have been involved in all stages of service delivery including assessment, care/support planning and evaluation?? 1.40 Do policies and procedures include time frames for assessment, planning, provision, evaluation, review and exit? (Note: this should align with contractual time frames) 1.41 Do care/support plans include all relevant needs of residents/consumers? 1.42 Are resident/consumer goals or outcomes identified using an assessment process? 1.43 Do care/support plans describe goals or outcomes and the required support required? 1.44 Are short term needs with planned interventions documented? 1.45 Is behavioural support clearly documented where appropriate including management of challenging behavioural? 1.46 Are care/support plans up to date? 1.47 Are evaluations and progress towards meeting desired goals documented by a registered nurse at least 6 monthly? 1.48 Are care/support plans changed (signed and dated) when progress toward outcomes (or goals) is less than expected? 1.49 Is there a programme of activities available that is meaningful to residents/consumers and includes community involvement? 1.50 Do planned activities reflect ordinary patterns of life and include the involvement of family/whanau and community groups (where appropriate)? 3 1.51 Does the service have policies and procedures that are based on recognised good practice for the management of medicine administration? 1.52 Do service policies and procedures identify medicine management responsibilities of staff? 1.53 Are staff that administer medicine trained and are records of their competency in the role completed? 1.54 Are allergies or sensitivities recorded in medication charts and resident files? 1.55 Are there procedures in place for the self-administration of medicines and are they adhered to? 1.56 Are medicines for self-administration safely stored? 1.57 1.58 Are internal audits of the medicine administration system completed? 1.59 Is there an agreement in place with the pharmacy? 1.60 (If relevant) where there is controlled drug medicine use, is there: 1. A controlled drug register, 2. Does regular checking (including weekly register checks) occur, and 3. Is there secure safe storage, and 4. Do signing charts align with controlled drug register? 1.61 Is there clear processes in place for medication reconciliation? 1. On admission a copy of the medication chart or script accompanies the resident, 2. Medication packs are checked against the medication chart on arrival from the pharmacy? 1.62 Are nutritional guidelines and information readily available to the residents and that meets their needs? 1.63 Is there dietitian input available as needed for residents that have been assessed as requiring specialist input? 1.64 Is there a current building warrant of fitness and (where relevant) are other compliances (e.g. for use of gas) met? 1.65 Are fire safety and emergency management procedures in place? 1.66 Are fire drills completed at least 6 monthly? 1.67 Is there is an evacuation scheme approved by the New Zealand Fire Service that meets the requirements of The Fire Service Act 1975? 1.68 Does the Restraint policy include definition of Enablers and clear assessment processes? 1.69 Is the use of enablers voluntary and does documentation reflect this? 1.70 Is the use of enablers the least restrictive option and consistent with the assessment, consent and care plan? 1.71 Has training been provided for staff around prevention of challenging behavior and use of de-escalation techniques? 4 1.72 Does the infection surveillance programme include collection of all infections? 1.73 Is the infection data collected analysed which leads to the development of action plans (where appropriate) to prevent or reduce infections? 1.74 Do staff meeting minutes include infection control surveillance activities? 2 Mental Health and/or Addiction Services (If applicable and note that MHA surveillance audits are unannounced) 2.1 Does the individual plan include involvement of clinicians and significant others? 2.2 Is the individual plan developed collaboratively with each person receiving the service and a copy is provided to them? 2.3 Does the individual plan with the resident / client have a recovery focus? 2.4 Is the identification of early warning signs and relapse prevention included in the individual plan? 2.5 Is the individual plan reviewed on a regular basis with the person receiving the service? 2.6 Does the service have a documented exit, discharge or transfer process for residents/consumers who relocate to another service including emergency transfer? 2.7 Does transfer/discharge documentation provide adequate information including identified risks? 2.8 Does exit, discharge or transfer include liaising with family/whanau of choice, and/or community support services where appropriate and records are maintained? 5 ACTION PLAN: SURVEILLANCE AUDIT SCOPE (FOR NON AGED CARE SERVICES) MODULE Ref # Self-assessment questions (for “No” responses above) Improvement action to be taken Due date Person responsible Date completed (Add additional rows as necessary) 6