File - Nitija Tiwari
advertisement

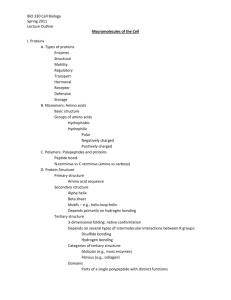
Nitija Tiwari CHEM 335 INTRODUCTION: Metabolism of the biomolecules is very essential for the normal functioning of our body. Any disturbance in the normal functioning of the metabolic pathway causes disorders in our body. These disorders may be genetic or may develop in an individual over time. The genetic diseases caused due to the errors in steps of metabolism are called inborn errors of metabolism. Among the inborn errors of metabolism, those caused by the errors in fatty acid metabolism are called Fatty Acid Oxidation Disorder or Lipid Storage Disorders. These genetic disorders are caused by enzyme defect which affects the ability of the body to oxidize fatty acids to produce energy within muscles, liver and other cells. Medium-Chain Acyl-coenzyme A Dehydrogenase deficiency, which is known as MCAD Deficiency is an example of the fatty acid oxidation disorder. As mentioned earlier, apart from the genetic disorders due to malfunctioning of the enzymes, the metabolism is also affected by other factors. The disease I propose, CAD (Coenzyme A Deficiency) leads to the disruption of the fatty acid oxidation but unlike the genetic disorder, individuals with this disorder develop the symptoms in adulthood. Before going into the details of the causes of this disorder, it is very important to have a strong knowledge of the Fatty Acid Oxidation pathway to identify some key regulatory steps in it. Fatty Acid Oxidation Pathway: Fatty acid oxidation occurs in three major steps. In a first energy consuming step, the fatty acid is activated by forming a high energy thioester bond with HS-CoA. These activated fatty acid units can be used for the synthesis of phospholipids and fats (triglycerides). Second, the activated acyl- CoA is oxidized and C2 units removed in the form of Acetyl-CoA in a cyclic process called betaoxidation. β- Oxidation takes place by recurring four steps: Oxidation of carbon-carbon double bond, addition of H2O to the double bond, with the formation of a hydroxyl group on one carbon, oxidation of the hydroxyl group by NAD+ to produce keto group and carbon-carbon bond cleavage releasing acetyl CoA. Third, acetyl-CoA moieties are funneled into the citric acid cycle for a final round of decarboxylation-oxidation reactions. This pathway is located in the mitochondrial matrix directly coupling the reducing equivalents in the form of NADH and H+ to oxidative phosphorylation and thus ATP synthesis. Key enzymes and substrate responsible for the Fatty Acid Oxidation: Enzymes Substrates 1. Acyl- CoA synthetase 1. HS-CoA 2. Pyrophosphatase Carnitine acyltransferase I 2. Carnitine 3. Cartinine acyltranferase II 4. Acyl-CoA dehydrogenase 5. Enoyl-CoA hydratase 6. Hydroxyacyl-CoA dehydrogenase 7. β – Ketothiolase The deficiency or malfunctioning of the enzymes and substrates listed above effect the process of fatty acid oxidation and as a result body faces disorders due to excessive accumulation of the fatty acids. A comparative analysis of the pre-existing disease known as MCAD Deficiency and the newly proposed disease called CAD is as follows: CAUSE: Medium-Chain Acyl-coenzyme A Dehydrogenase Deficiency (MCAD Deficiency): Medium-chain acyl-CoA dehydrogenase (MCAD), acts on fatty acyl-CoA molecules that range in size from 12 down to 4 carbons in length. Deficiency in MCAD is the most common inborn error of fatty acid metabolism and effects mitochondrial β-oxidation of fatty acids. MCAD Deficiency is inherited in autosomal recessive pattern and is a condition that prevents the body from converting certain fats to energy, particularly during periods without food (fasting). Symptoms of MCAD deficiency generally begin to occur between the second month and second year of life. It is very rare that the symptoms start in adulthood. Mutations in the ACADM gene cause MCAD deficiency. By far, at least 340 mutations in the ACADM gene have been identified and the most prevalent mutation i.e. 89% found in MCAD deficiency patients is a single nucleotide substitution at position 985. This substitution is A for G change that converts amino acid 329 from a lysine to a glutamic acid (K329E), thus changing the enzyme structure. This gene provides instructions for making an enzyme called medium-chain acyl-coenzyme A dehydrogenase, which is required to break down (metabolize) a group of fats called mediumchain fatty acids. These fatty acids are found in foods and the body's fat tissues. Fatty acids are a major source of energy for the heart and muscles. During periods of fasting, fatty acids are also an important energy source for the liver and other tissues. Hence due to the deficiency of the MCAD enzyme, the fatty acids cannot be broken down which stops the production of energy leading to the signs and symptoms of MCAD deficiency lack of energy (lethargy), and low blood sugar (hypoglycemia). Also, the medium- chain fatty acids which cannot be catabolized accumulate in the body cells causing other serious problems like seizures, breathing difficulties, liver problems, brain damage, coma, and sudden death. CAD (Co-enzyme A Deficiency) This newly proposed disease has the similar symptoms as the individual with the MCAD deficiency because the body is unable to oxidize fatty acid in both the cases. But the difference is that in this case, the individual develops the symptoms in adulthood rather than soon after birth. In contrast to the MCAD Deficiency, the appearance of the symptoms soon after birth in this case is very rare. The CAD is caused by the deficiency of the Co-enzyme A in the cytoplasm (intermembrane space). As a result, the fatty acid synthesis cannot be initiated by activating the fatty acid with the thioester bond. The deficiency of Co-enzyme A is caused by the deficiency of Vitamin-B5 (Pantothenic Acid) in the individual. Hence, along with the symptoms common to MCAD, the individuals with this deficiency also develop numbness, muscle cramps, sleep disturbances and abdominal cramps associated with Vitamin- B5 deficiency. DIAGNOSIS: The differential diagnosis of the MCAD Deficiency from other Fatty Acid Oxidation Deficiencies is difficult to achieve with a single test. Hence, a number of integrated tests are to be carried out and interpreted for the proper diagnosis of this disease. Looking at the person’s family history can be the first step to suggest whether or not the disorder is a genetic disorder. The further tests include: - Plasma acylcarnitines analysis, plasma fatty acid (free or total) profile, urine organic acids, and urine acylglycines analysis. The biochemical test of the MCAD Deficiency can be confirmed by measurement of MCAD enzyme activity in fibroblasts or other tissues and/or by molecular genetic testing of the ACADM gene. The acylcarnitine profile of individuals with MCAD deficiency is characterized by accumulation of C6 to C10 species, with prominent octanoylcarnitine. Also, in the plasma fatty acid test, the total fatty acid concentrations in the plasma are analyzed. Similarly, in the urine analyses, the urine of MCAD patients has been found to have high levels of medium-chain dicarboxylic acids and very low level of ketones. The problem associated with using just one test for diagnosis also holds true for the diagnosis of CAD. Various tests are required to confirm CAD. As the individual will have normal MCAD, the tests for the mutation of MCAD will be negative. Another, diagnosis method which can distinguish this new disease from MCAD Deficiency is looking at the individual’s family history. If no one in his family has this problem, then that is a sign that the disorder is probably not a genetic disorder. Similarly, the tests for other enzymes involved in fatty acid synthesis will also be normal. But the result of other tests mentioned for the MCAD Deficiency will be similar to that of MCAD Deficiency results. The symptoms related to Vitamin- B deficiencies can also be used as the signs of this disease. TREATMENT: Treatment for MCAD deficiency is simple. The treatment consists of avoiding fasting for more than 2-6 hours in an infant. After infancy, overnight fasts of longer than 12 hours should be avoided. These values may vary from person to person. A high carbohydrate diet with restriction of fats and supplemental carnitine is recommended, especially during illness. It is important that the treatment process followed throughout the lifetime of the affected individual. If an individual is unable to keep down fluids, has diarrhea or a fever, he or she should be evaluated promptly and given intravenous glucose immediately following blood chemistry sampling. It is seen that some doctors prescribe a drug called L-Carnitine to children. This drug helps the child's blood sugar from getting low when they have infections or when they do not eat. L-Carnitine is a substance made by the body that carries wastes out of body cells and into the urine. Individuals with MCAD make more toxic wastes than normal individuals so they need more L-Carnitine to carry out this process. As CAD is caused by the deficiency of Vitamin B5, intake of Vitamin B5 substituents will easily cure this disease. The sources of Vitamin B5 include meat, whole grains like rice, wheat barns, condensed fish solutions, and multivitamin tablets. Bibliography: Boyer, Rodney. Concepts in Biochemistry. John Wiley and sons Inc., 2006. http://www.whatislife.com/reader2/Metabolism/pathway/fattyacids.html http://ghr.nlm.nih.gov/condition/medium-chain-acyl-coenzyme-a-dehydrogenase-deficiency http://www.ncbi.nlm.nih.gov/books/NBK1424/ http://www.hgen.pitt.edu/counseling/public_health/mcad.htm http://themedicalbiochemistrypage.org/mcad.html www.lifeclinic.com/focus/nutrition/vitamin-b5.asp