Headache Referral – Neurology Service
advertisement

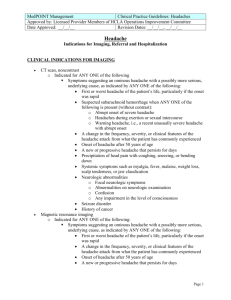
Leeds CCGs Targeted Interventions Referral Form Headache Referral – Neurology Service Referral to: (insert patient’s choice of hospital) Patient Details: Title Surname Forename(s) Address Referrer Details: Referring GP Practice Address Diagnostic guide: (see overleaf for details) Episodic tension type headache Chronic tension type headache Migraine Analgesic overuse headache Cluster headache Suspicious headache (see also 2 week referral guidance) More likely to need referral to specialist More likely to be managed in primary care D.O.B NHS Number Tel (home) Tel (mobile) Gender Ethnicity Age Is an interpreter required Yes No Is transport required Yes No Telephone Fax Practice Code Please select all that apply: Episodic tension type headache Chronic tension type headache Migraine Analgesic overuse headache Cluster headache Suspicious headache (see also 2 week referral guidance) Describe details of headache (duration, site, nature) Include your reasons for wanting a consultant opinion: Describe any accompanying symptoms (visual disturbance, nausea, aura, focal neurological signs) Describe any related or possible causative factors (stress, posture, TMJ dysfunction, sinus problem) Please provide details of previous treatment regimens including doses and durations: Significant past medical history: Review Date: April 2016 Current medication: GP Signature: Date: Headache Symptoms - A symptom based guide to possible diagnosis: (note: more than one type of headache may co-exist) Episodic tension type headache: (affects 80% of the population) Typically bilateral, often band-like or pressure feeling, may have muscle tenderness, may be stress related. (may respond to paracetamol or NSAID) Chronic tension-type headache: (affects 3% of the population) Occurs >15 days a month, may be unremitting and not respond to analgesia. May be related to stress or long standing neck problems (May respond to amitriptyline) Migraine: (affects 10% of the population) Often unilateral, often throbbing, last up to a few days, may be aura, nausea or visual disturbance, or focal neurology such as paraesthesia of hand, arm or face for up to 60 minutes (If this last longer, always refer) Analgesic overuse headache: (affects 5% of the population) Typically daily, oppressive, worse on walking, worse on exertion. Consider if using over 3 tablets a day for over 3 days a week regularly. (Ask patient to keep a headache diary) Cluster headache: (affects <1% of the population) Strictly unilateral, severe/unbearable, around eye, often at night, may have red or watering eye, rhinitis, or blocked nose. Alcohol triggers. (Refer early to specialist) Suspicious headache: (affects <1% of the population) New onset, qualitatively different, unusually severe and not responding to usual measures. Persisting neurological signs Optic disc changes Suspicion of malignancy (see 2 week referral guidance) Meningism, acute neck stiffness Primary closed angle glaucoma Temporal arteritis or raised ESR without cause Suspected carbon monoxide poisoning (Refer Urgently if any of the above are present) Supporting evidence Headache (BMJ 2002; 325:881-886) www.bash.org.uk (The British Association for the Study of Headache) www.prodigy.nhs.uk (several guidelines on managing headaches and migraine) Review Date: April 2016