File
advertisement
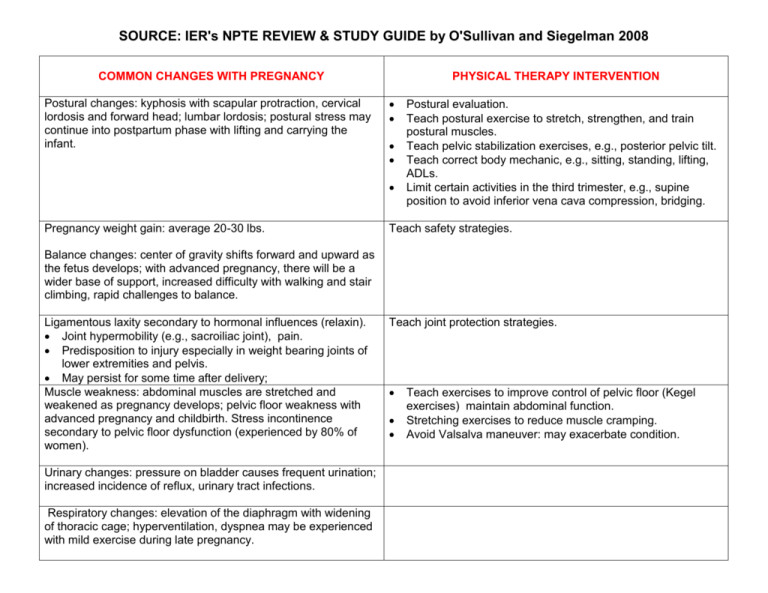
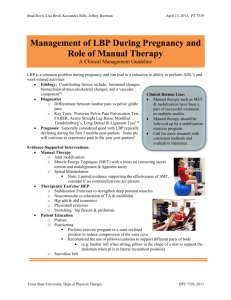
SOURCE: IER's NPTE REVIEW & STUDY GUIDE by O'Sullivan and Siegelman 2008 COMMON CHANGES WITH PREGNANCY Postural changes: kyphosis with scapular protraction, cervical lordosis and forward head; lumbar lordosis; postural stress may continue into postpartum phase with lifting and carrying the infant. PHYSICAL THERAPY INTERVENTION Pregnancy weight gain: average 20-30 lbs. Postural evaluation. Teach postural exercise to stretch, strengthen, and train postural muscles. Teach pelvic stabilization exercises, e.g., posterior pelvic tilt. Teach correct body mechanic, e.g., sitting, standing, lifting, ADLs. Limit certain activities in the third trimester, e.g., supine position to avoid inferior vena cava compression, bridging. Teach safety strategies. Balance changes: center of gravity shifts forward and upward as the fetus develops; with advanced pregnancy, there will be a wider base of support, increased difficulty with walking and stair climbing, rapid challenges to balance. Ligamentous laxity secondary to hormonal influences (relaxin). Joint hypermobility (e.g., sacroiliac joint), pain. Predisposition to injury especially in weight bearing joints of lower extremities and pelvis. May persist for some time after delivery; Muscle weakness: abdominal muscles are stretched and weakened as pregnancy develops; pelvic floor weakness with advanced pregnancy and childbirth. Stress incontinence secondary to pelvic floor dysfunction (experienced by 80% of women). Urinary changes: pressure on bladder causes frequent urination; increased incidence of reflux, urinary tract infections. Respiratory changes: elevation of the diaphragm with widening of thoracic cage; hyperventilation, dyspnea may be experienced with mild exercise during late pregnancy. Teach joint protection strategies. Teach exercises to improve control of pelvic floor (Kegel exercises) maintain abdominal function. Stretching exercises to reduce muscle cramping. Avoid Valsalva maneuver: may exacerbate condition. Cardiovascular changes: increased blood volume; increased venous pressure in the lower extremities; increased heart rate and cardiac output, decreased blood pressure due to venous distensibility. Teach safe progression of aerobic exercises. o Exercise in moderation, with frequent rests. o Stress use of familiar activities; avoidance of unfamiliar. o Postpartum: emphasize gradual return to previous level of activity. Stress gentle stretching, adequate warm-ups and cooldowns. Teach ankle pumps for lower extremity edema (late stage pregnancy); elevate legs to assist in venous return. Wear loose, comfortable clothing. Altered thermoregulation: increased basal metabolic rate; increased heat production. PREGNANCY-RELATED PATHOLOGIES PHYSICAL THERAPY INTERVENTION Diastasis recti abdominis. Lateral separation or split of the rectus abdominis; separation from mid-line (linea alba) greater than 2 cm is significant; associated with loss of abdominal wall support, increased back pain. . Pelvic floor disorders: the result of weakening of pelvic floor muscles (pubococcygeal muscles, PC). a. PC muscles normally function to support the vagina, urinary bladder, and rectum and help maintain continence of the urethra and rectum. b. Weakness or laxity of PC muscles typically results from overstretching during pregnancy and childbirth. Further loss of elasticity and muscle tone during later life can result in partial or total organ prolapse. Examples include. Cystocele: the herniation of the bladder into the vagina. Rectocele: the herniation of the rectum into the vagina. Surgical correction is often required, depending on degree of prolapse. Teach protection of abdominal musculature: avoid abdominal exercises, e.g., full sit-ups or bilateral straight leg raising. Resume abdominal exercises when separation is less than 2 cm: teach safe abdominal strengthening exercises, e.g., partial sit-ups (knees bent), pelvic tilts; utilize hands to support abdominal wall Observe for: urinary frequency and urgency, painful urination, painful defecation; low back and perineal pain with prolapse. Teach pelvic floor exercises (Kegel exercises) to strengthen the PC muscles is indicated. Postural education and muscle reeducation, pelvic mobilization, and stretching of tight LE muscles are also important components. Uterine prolapse: the bulging of the uterus into the vagina. c. PC muscles can also go into spasm. d. Symptoms include pelvic pain (perivaginal, perirectal, lower abdominal quadrant), urinary incontinence, and pain with sexual intercourse. Red Flag: Pain can radiate down the posterior thigh. Low back and pelvic pain. Teach proper body mechanics. Balance rest with activity. Emphasize use of a fIfm mattress. Massage, modalities for pain (no deep heat). Sacroiliac dysfunction secondary to postural changes, ligamentous laxity. a. Symptoms include posterior pelvic pain; pain in buttocks, may radiate into posterior thigh or knee. b. Associated with prolonged sitting, standing, or walking. Physical therapy interventions. External stabilization, e.g., sacroiliac support belt, may help reduce pain. Avoid single limb weight-bearing: may aggravate sacroiliac dysfunction. Varicose veins: may produce discomfort or pain. Physical therapy interventions. Elevate extremities; avoid crossing legs which may press on veins. Use of elastic support stockings may help. Preeclampsia: pregnancy induced, acute hypertension after the 24th week of gestation. a. May be mild or severe. b. Evaluate for symptoms of hypertension, edema, sudden excessive weight gain, headache, visual disturbances, or hyperreflexia. c. Initiate prompt physician referral. Cesarean childbirth Surgical delivery of the fetus by an incision through the abdominal and uterine wall; indicated in pelvic disproportion, failure of the birth process to progress, fetal or mother distress, or other complications. b. Physical therapy interventions. Postoperative TENS can be used for incisional pain; electrodes are placed parallel to the incision. Prevent post-surgical pulmonary complications: assist patient in breathing, coughing. Post-cesarean exercises. o Gentle abdominal exercises; provide incisional support with pillow. o Pelvic floor exercises: labor and pushing is typically present before surgery. o Postural exercises; precautions about heavy lifting for 4-6 weeks. Ambulation. Prevent incisional adhesions: friction massage. Physical therapist may teach childbirth education classes. a. Relaxation training: e.g., Jacobsen's progressive relaxation, relaxation response, mental imagery, yoga. b. Breathing management: slow, deep, diaphragmatic breathing; Lamaze techniques; avoidance of Valsalva. c. Provide information about pregnancy and childbirth.