Cerebral Arterial Gas Embolism Patients Treated with Hyperbaric
advertisement

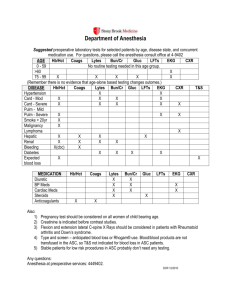
Cerebral Arterial Gas Embolism Patients Treated with Hyperbaric Oxygen at Hennepin County Medical Center Hyperbaric Oxygen Chamber from 1987-2010: Data table # 1 2 Age 57 73 Sex M M A/V V A Cause of embolism Right CVC catheter removal Pneumothorax related to lung biopsy 3 days prior to CAGE, colonoscopy done 1 day prior to CAGE (air entry could be due to either of two events) Colonoscopy 1 day back, lung biopsy with Pneumothorax 3 days back, Metastatic Rectal CA, COPD, lung nodule bx positive for CA , carotid stenosis , IDDM, HTN, CAD, previous CVAs, DVT, OSA, IBD Unresponsiveness with decerebrate posturing, brain stem reflexes present. CT scan showing air/infarct/ edema in R MCA territory Cardiac catheterization 2 days prior for Congenital heart disease L hemiplegia with incontinence CT head showing air in R MCA distribution, MRI with acute infarct in R MCA territory Multiple HBO2 sessions for treatment of soft tissue radiation injury to mandible, emphysema. R sided hemiplegia upon ascent during 28th treatment DM2, pain meds abuse, hypothyroidism, hyperlipidemia Severe right sided headache,photophobia, blurring vision 60 M A 5 50 F V Self-exploration of porta-cath 6 7 55 56 F M M V Diagnostic imaging before HBO2 Tachypnea, SOB, stool incontinence, right gaze preference, L sided paralysis, and complete L sided neglect. 4 3 Initial Sign and Symptoms of CAGE R side 15% TBSA burn,history of alcohol abuse, pancreatic CA s/p resection &esophagectomy, depression Cardiac catheterization Pulmonary overpressure accident with CAGE during HBO2 treatment for soft tissue radiation injury 3 Medical comorbidities V 30-55 cc of air introduced during dialysis for ESRD CAD s/p CABG s/p PCI, HTN, DM2, polysubstance abuse including EtOH A Percutaneous closure of ASD ASD, NIDDM, OSA, HTN LOC during dialysis for ESRD,Chest pain,dyspnea, nausea, headache, R sided focal weakness with paresthesia in R leg LUE paralysis and L facial droop and LLE weakness and confusion, altered mental status CT head showing air in R MCA territory Not done CT head showed air in L jugular vein, cavernous sinus, sup ophthalmic veins and cervicomedullary junction Time to HBO2 Other diagnostic tests& treatments 3 hrs Myringotomy BL, intubation, IV rt-PA loading dose. Unremarkable EKG changes, negative troponins, CXR: no pneumothorax, LLL opacity consistent with atelectasis and small pleural effusion 13hrs 20 mins Intubation, chest tube for recent pneumothorax, elevated troponins, EKG showing anterior wall MI. 13 hrs 53 mins ECHO showing air in R ventricle shunting to left & thrombus in IVC, CXR with left hilar infiltrate, Myringotomy BL, intubation 1 hrs 12 mins None CT head with no air in vasculature 3 hrs EKG: Sinus rhythm with mild inferior ST-T wave changes ASA, NTG, Bedside ECHO likely ASD,EKG:LVH and non-diagnostic ST segment changes, CXR: chronic L pleural effusion and apparent atelectasis, bilateral myringotomy CT head with air embolus in right frontal lobe 4hrs 48 mins EKG:sinus tachycardia with no ST elevations. ~ 13 hrs HBO2 sessions Treatment table 3 USN Table 6 x 1 and table 5x2 1 2 USN Table 6 USN Table 6x2 Complication during HBO2 Final Outcome None Improved. Completely recovered LUE motor function, LLE strength 3/5. f/u CT with evolving infarct, no air none Died (Diffuse brain injury). F/U head CT : massive right MCA/ACA infarct/edema & smaller amount or scattered air in R MCA distribution. none Died. F/U head CT Massive right MCA infarct, cerebral edema, air foci. 1 USN Table 6 none Resolution. Follow up MRI showed mild ischemia in L perirolandic and ant parietal lobes 1 USN Table 6 none Resolution of vision blurriness but persistent HA. F/U head CT: no air none Resolution of symptoms and neurologic deficits. F/U head CT infarct left frontal lobe none Improved. Follow up CT head showing small R anterior frontal infarct with no residual air. 1 1 USN Table 6 USN Table 6 Cerebral Arterial Gas Embolism Patients Treated with Hyperbaric Oxygen at Hennepin County Medical Center Hyperbaric Oxygen Chamber from 1987-2010: Data table 8 9 10 11 53 72 53 66 M M M M A V V A Cardiac ablation procedure for Chronic Afib Chronic afib, TBI w/ L sided weakness, seizure disorder Confusion, hypotension,bradycardia, chest and back pain w/ third deg heart block Hickman catheter disconnected HTN, Diabetes s/p laser for retinopathy, COPD and CRF AMS, acute bilateral blindness,subjective weakness, SOB,hypotension, hypoxemia cardiac radioablation CAD with coronary artery stents, atrial fib/ flutter, SVT Severe L facial droop, left visual field cut with slurred speech Carotid and Innominate stenting CAD, large vessel atherosclerotic dis, COPD, obesity, dyslipidemia, 12 41 F A Lung biopsy spindle cell CA, R hip and leg amputation, 13 41 F V CVC removal ESRD s/p renal transplant, HTN, cholecysectomy CT head with gas embolism in the brain. AMS, not moving extremities Head CT wit BL cerebellar and pontine infarcts thought to be metastatic emboli initially, no air seen > 30 hrs Seizures, coma(GCS 45, responding to pain) CT head: normal, MRA: normal 3.5hrs CT head with diffusely low attenuation, no air 28hrs EKG:sinus rhythm, poor R wave progression, lateral ST depression, CXR: hilar congestion, Swanganz catheter and three chest tubes, myringotomy BL CT head: normal 6.5hrs Not done 5.25hrs F A Aortic valve replacement CAD, CHF, severe AS, Afib, COPD 15 40 F V CVC cap off s/p ventral hernia repair with ileus, IBS, migraine, malnutrition Seizures after anesthesia wore off, unresponsiveness Sudden right hemiparesis, numbness, headache, and aphasia when she sat up CVC removal Guillain-Barre syndrome w/ neurological motor deficits in BL LE 3/5 strength, also decreased sensation Sudden hypotension, tachycardia, hypoxia, chest pain, seizure F V Unknown but likely less than 12 hrs Left sided facial, arm and leg paralysis, right gaze preference 86 17 CT head – right occipital infarct CT head with air in cerebral vasculature (R MCA dist) 10 hrs 10 mins Heparin,Myringotomy BL, EKG: long QT, PVCs and BBB Intra-arterial rt-PA prior to diagnosis of CAGE, followed by CT head showing gas embolism ,intubation, sedation, myringotomy, EKG: new lateral ST depression Cardiac ECHO: decreased EF, elevated trops 7.4, CK 778, EKG: sinus tach, anterolateral T wave changes. CXR: left lower lobe atelectasis. Myringotomies Cardiac ECHO showing ASD w/ R-->L shunt. Elevated trops, lactate, CK. EKG: nonspecific ST-T changes, CXR: normal 14 16 None Cardiac angiographyshowed occluded LAD with air in L ventricle. TTE – LAE, mod TR, elevated trops, ST elevation. CXR: bibasilar atelectasis with no infiltrates. CXR: air in pulmonary artery and right ventricle,pulmonary edema, EKG: peaked T-waves, left ant fascicular block, potassium was 6, elevated troponins Likely ~ 12 hrs 4-6 hrs CXR: normal,myringotomy, EKG: normal CXR vascular congestion, ABG – hypoxia, EKG w/ sinus tachy. Cardiac ECHO showed no air, EKG w/ sinus tachy 1 USN Table 6 none Resolution Unchanged. F/u MRI right occipital infarct. EEG: R posterior quadrant epileptogenicity. DNR/DNI >hospice care 1 USN Table 6 aborted d/t seizures and respiratory distress 1 USN Table 6 with ext at 60ft and 30ft none Improved. Follow up CT with infarct in R MCA territory. 1 USN Table 6, aborted due to Cushing's reflex. Brady-asystolic event, declining neurological status Died. F/U head CT with massive R basal ganglia ICH with edema & midline shift, loss of brain stem reflexes > Comfort care. 1 USN Table Table 6 none Unchanged. Bilat cerebellar and pons infarcts on f/u MRI 1 USN Table 6 – aborted due to seizures Continued seizures during HBO2 Improved. 2 Table 6, Table 5 Continued to seize sometimes during HBO2 Unchanged 1 USN Table 6 None Improved 1 USN Table 6A Bilat pleural effusion, SOB Improved Two seizure episodes during HBO2 treatment with headache Cerebral Arterial Gas Embolism Patients Treated with Hyperbaric Oxygen at Hennepin County Medical Center Hyperbaric Oxygen Chamber from 1987-2010: Data table 17 18 70 49 F F V V Abdominal insufflation after resection of lung cancer CV catheter leak Lung cancer, COPD, HTN, PFO ESRD, IDDM, CABG, Gastroparesis CVA, CHF with pulm edema hypothyroid, migraine HA 19 38 F V R Internal jugular catheter accidentally came out in clinic 20 42 M V Subclavian CVC line removed HIV, pancreatitis with sepsis ESRD on dialysis, AIDS, HTN s/p tongue CA resection radical neck dissection, pulm mets, partial pneumonectomy Arthritis, Lupus, central line for chemotherapy 21 42 M V 22 56 M V End of dialysis quinton fell off, when rolled over in bed catheter noted bleeding. HBO2 Rx for osteoradionecrosis 16th treatment during ascent V L Subclavian CVC line removal. Patient coughed during removal Ulcerative Colitis, Migraine HA V Patient heard air rush into neck when SwanGanz removed, cordis left in place GI Bleed, aortojejunal fistula, AAA, CABG V Dialysis tubing disconnected while on dialysis. Venous line of Quinton ESRD on dialysis. Afib DM, Hyperkalemia, Dementia, Breast CA 23 24 25 17 73 80 M M F Acute hypotension (SBP 70 mmHg), coma Day 1: CP, trop 1.1. Day 3: CP, nausea, SOB, R neck and jaw pain, R parietal HA . Day 4 R neck and jaw pain ,confusion, anxiety HA, stiff LUE, new cardiac rub. Day 5 sudden deterioration, worse CP SOB irritability, somnolent, LUE weakness Abrupt Loss of Consciousness, decrease mental status, dizziness. Progressing ARDS, disorientation fluctuating mental status Cardiopulmonary arrest s/p CPR sedated and paralyzed. Seizures after resuscitation, GCS 3 Heard woosh of air, felt dizzy R sided heaviness, decreased R arm movement, R leg heavy &weak, R lower facial weakness &"numbness" speech disturbance. Weakness R arm and leg without neglect Sudden SOB, near syncope during CXR, questionable seizure activity, obtundation, decreased vision Reduced level of consciousness , obtunded, posturing Respiratory then cardiac arrest,resuscitated to afibwith rapid vent response, eyes open, unresponsive, no CT head: 2 hrs after event showing small foci of air in post parasagittal left frontal lobe 7 hrs CT head: air, multiple small infarcts. HCT 2 days prior: normal. MRI 2 days prior: multiple bilateral infarcts. CXR: air under diaphragm, subcutaneous emphysema. Normal trops, CK 836, EKG: inverted T waves. Two chest tubes, Myringotomy BL. 1 USN Table 6 none Died. Withdrawal of care on day 2. MRI day after admission: bihemispheric infarcts. CT head: normal 28 hrs CT head: normal 10.75 hrs TTE: air in RV, no shunt, dec LV Fxn, inf LVWMA. EKG: Q wave inferiror leads,,LVH. CXR:mild cardiac, pulm edema. TEE - no air, no shunt poss AV malform Myringotomy BL, LP normal, CXR - BL infiltrates, Echo: normal, no air.Chest CT – diffuse BL infiltrateswith pulm edema. EKG: sinus tachy. Intubated. Chest CT/ Angio: normal.EKG: sinus tachy perihilar infiltrates, pulm edema Not done 6 hrs EKG: NSR, LVH. CXR interstitial pulm edema, cardiomegaly. EEG: normal 1 USN Table 6 none Resolved Not done 0immed N/A 1 USN Table 6 none Resolved CT head: with air in cerebral vasculature ~ 4.45 hrs 1 USN Table 6 none Resolved. F/U head CT no air or infarct CT head: no acute infarct or air ~ 9hrs EKG: incr voltage. CXR: interstitial changes Cardiac Echo: air in BL A+V. Loud cardiac murmur. CXR - no free air cordis removed, repeat echo - no air. EKG: sinus tachy, LVH CXR: BL infiltrates, pulm edema, intubated, aline radial cutdown 1 USN Table 6 Unstable BP ~ 5 hrs CXR: BL pleural effusion, R interstitial pattern pulm edema. Intubated 1 USN Table 6 none 5 days Not done 1 USN Table 6A fever 103.4 Improved. Speech and motor activity on R arm/leg improved, Dec spasticity on Left 1 USN Table 6 none Resolved 1 USN Table 6 none Unchanged. Anoxic brain Injury, DNR/DNI to nursing home Resolved. Unchanged. Family withdrew support & pt passed away two weeks later due to worsening from probable aspiration Cerebral Arterial Gas Embolism Patients Treated with Hyperbaric Oxygen at Hennepin County Medical Center Hyperbaric Oxygen Chamber from 1987-2010: Data table spontaneous movement absent pupillary and corneal reflexes, +gag, triple flexion. 26 27 28 29 30 31 32 33 34 67 7 81 26 48 24 34 43 50 F F M F F F F F F V A CT guided transthoracic needle biopsy of pulm mass Repair ASD, cardiac bypass, ventilator malfunction allowed air into arterial system via ASD pneumonia and septicemia. F/U imaging diffuse edema/ bilateral infarct. Pulmonary mass Confusion becoming more obtunded, R decorticate posturing, R Babinski, L gaze preference, dysarthria MRI brain: negative for bleed or air 22 hrs Cardiomegaly from ASD Not awakening from anesthesia, GCS 3 CT head: attenuation on the R parietal area, no air. 3.25 hrs EEG diffuse delta activity in L, EKG: NSR, CXR: focal LLL edema vs. atelectasis V CT guided biopsy of pulmonary mass Prostate CA, Colon CA, Pulm Fibrosis, CAD, AS porcine aortic valve replacement A Catheter placement in R femoral artery for L carotid injection Recalcitrant epilepsy Became deeply unresponsive during procedure, GCS 3, Seizure First inappropriate giggling,R hemiparesis (facial and RUE), aphasia, R sided neglect, seizures for 90 seconds. Mitral Valve Plasty CRF. Mitral Stenosis, Aortic valve Insufficiency Arrested, bypass, aortic balloon pump, GCS 3, Ventricular tachy x 2 in ED. Not done ~ 8 hrs EKG: NSR Cardiac Echo: Large air in L CVC, air in R ventricle shunting to L through septal defect. Chest tube.Myringotomy WADA Study Intractable Seizure Disorder Depressed mental status, dysarthria, R sided weakness > 20 min. CT head: no abnormality, no air 6.25 hrs Myringotomies V A Left internal carotid Injection A L common carotid angiogram,10cc air injected Neck laceration zone, needing carotid angiogram Decreased mental status, not responding to voice or sternal rub, pupils reactive, withdraws to pain all extremities,RUE toes up V Open heart surgery for removal of infected right atrial thrombus. Air introduced into R ventricle, found in LV. Surgery proven PFO Sepsis due to positive blood cult Staph epidemidis from long term indwelling Hickman catheter Did not recover normal mental statusafter surgery. Obtunded, not following commands. Pupils reactive, DTR intact, Clonus lower extremities, MV replacement 1981, TIA's Decerebrate- decorticate posturing, pupils fixed/dilated, deep coma, improving over 24 hrsto spont moving all extr and opening eyes. Hyperreflexic, sustained clonus, BL Babinski. A Mitral Valve Replacement air introduced canalizing aorta CT head: air in cerebral circulation ~4.5 hrs Not done 5.5 hrs Not done Not done CT head: no abnormality EKG: NSR, CXR: small rightpneumothorax. R chest tube 1 USN Table 6 none Improved 1 USN Table 6a none Improved 1 USN Table 6a Status epilepticus during HBO2 (no response to dilantin & phenobarbital) Improved. Family withdrew care later on and died. F/u CT diffuse cerebral edema, loss of sulci. 1 USN Table 6 None Resolved 1 USN Table 6a balloon pump stopped at 60' patient tolerated, no consequences Unchanged. Withdrawal of support and passed away 1 USN Table 6a Improved. MRI L middle temp lobe abnormality (old), No infact/edema 1.5 hrs EKG: diff ST-T depression, sinus tachy, no infiltrates 1 USN Table 6a Sinus squeeze Status epilepticus during HBO2 for about 2hrs. Seizures due to illness did not stop with air break ~ 6 hrs Air aspirated at time of surgery from both ventricles. EKG: NSR, ST elevation inferior and lateral. BL chest tubes. CXR: no infiltrates or effusion. 1 USN Table 6a None Improved. Aphasic, slow speech, R hemiparesis, ambulates independently, lives at home with health aide Improved. At d/c answering questions sometimes inappropriate, follows commands, not speaking spont, LEs > UEs spont extremity movement. F/U head CT: no acute changes 30 hrs CXR: no infiltrate, cardiac ECHO: NSR, EEG improving response,deep coma. Intubated, BL chest tubes placed, CVC line USN Table 6A extended by USN Table 4 Post HBO2consolidatio n in LLL, progressed and prevented further HBO2 (O2toxicity) Improved. F/U CT with cerebral edema consistent with past air embolism. 1 Cerebral Arterial Gas Embolism Patients Treated with Hyperbaric Oxygen at Hennepin County Medical Center Hyperbaric Oxygen Chamber from 1987-2010: Data table Intubated, ventilator L CV line, R removed Acute SOB, dyspnea, CT head: ICH increase pulm edema 35 49 M V tachycardia, confusion improving, no air ~ 4.5 hrs NSR 1 6a None Improved Chest pain, SOB, headache when stood up.Noted wetness and L side decreased bubbling from Hickman pin prick and light Hickman catheter Idiopathic site, split in it, was EKG: diffuse T wave touch and mild Resolved. F/U head CT 36 25 F V split dysautonomia, TPN playing with dog. CT head : normal ~ 5.5 hrs inversions 1 USN Table 6a motor weakness no change. Abbreviations used: #= number, CAGE = cerebral arterial gas embolism, A/V= arterial/venous, CVC= central venous catheter, HBO2 = hyperbaric oxygen, F/U =follow up, TBSA=total body surface area, s/p=status post, rt-PA= recombinant tissue plasminogen activator, CXR: chest x-ray, LLL= left lower lobe, CAGE= cerebral arterial gas embolism, CA= cancer, MCA=middle cerebral artery, BL=bilateral, CAD= coronary artery disease, CABG= coronary artery bypass graft, PCI=percutaneous coronary intervention, EtOH= alcohol, LOC=loss of consciousness, ESRD= end stage renal disease, Afib= atrial fibrillation, TBI=traumatic brain injury, AMS=altered mental status, ICH=intracerebral hemorrhage, CRF= chronic renal failure, ASD= atrial septal defect, USN= United States Navy. Patient cut subclavian CVC ICH, left hosp. AMA w/ CVP line