Thyroid Cancer
advertisement

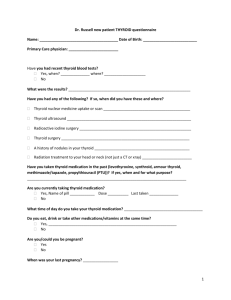
Thyroid Cancer ( for residents and specialists) Introduction Thyroid cancer is the most common endocrine malignancy, accounting for more than 95% of all endocrine cancers.The spectrum of thyroid cancer ranges from occult papillary thyroid carcinoma, which has a relatively benign course, to aggressive anaplastic thyroid carcinoma. Fortunately, more than 90% of all thyroid cancers are well differentiated, and individuals with these tumors have a good long-term prognosis. Clinical Presentation and Diagnosis Most thyroid cancer patients present clinically with a palpable thyroid nodule. These are usually asymptomatic. In rare cases, patients present with hoarseness, pain, dysphagia, dyspnea, coughing, or choking spells. Pain associated with a malignant thyroid lesion should raise the suspicion for medullary thyroid carcinoma, anaplastic carcinoma, or lymphoma. In evaluating patients for thyroid cancers, clinical history and physical examination remain the cornerstone of appropriate management. historical factors predicting malignancy include a history of head and neck irradiation; total body irradiation for bone marrow transplantation; a family history of thyroid cancer; and rapid growth or hoarseness. Children, men, and adults older than 60 years have an increased risk of malignancy. Personal and family history of other endocrine disorders, specifically hyperparathyroidism, pituitary adenomas, pancreatic islet cell tumors, adrenal tumors, and breast cancer increase the risk of thyroid cancer. A family history of papillary or medullary carcinoma (multiple endocrine neoplasia [MEN] syndromes), familial polyposis also risk factors for thyroid cancer. With the discovery of a thyroid nodule, a physical examination focusing on the thyroid gland and adjacent cervical lymph nodes should be performed. physical findings suggesting possible malignancy include a “hard texture” of the thyroid nodule, cervical lymphadenopathy, vocal cord paralysis, and fixation of the nodule to surrounding tissue. Patients presenting with hoarseness or patients planned for reoperation should have a direct laryngoscopy before any surgical intervention to document the function of the vocal cords. High-resolution thyroid ultrasonography has become an extension of the physical examination in the evaluation of thyroid disease. Recent investigations have documented that three sonographic features were significant independent risk factors for malignancy: irregular margins, intranodular vascular pattern, and microcalcifications. FNA biopsy (FNAB) is the most reliable and cost-efficient method for evaluating thyroid nodules. These should now routinely be performed under ultrasound guidance for small or difficult-to-palpate or complex nodules to reduce failure rates. FNAB is not as accurate in radiation-induced thyroid cancer or in patients with a family history of thyroid cancer; these patients should undergo surgical resection if there is clinical suspicion of malignancy. Preoperatively, all patients should therefore undergo ultrasound examination of the thyroid gland and cervical lymph nodes, as well as thyroid function tests, serum thyroglobulin, and antithyroglobulin antibody levels and blood calcium levels. In the case of medullary thyroid cancer, serum calcitonin, CEA, and calcium levels should be obtained. All patients with medullary thyroid cancer should also be tested for the RET proto-oncogene and evaluated for pheochromocytoma and hyperparathyroidism before surgery. Well-Differentiated Thyroid Carcinoma 1) Papillary Thyroid Carcinoma PapillaryThyroid Carcinoma accounts for approximatel 70% of all thyroid malignancies, it is has best prognosis.Papillary thyroid cancer is twice as common in women as men and has a peak age of presentation of 38 to 45 years. This tumor also accounts for 90% of radiationinduced thyroid cancer and is familial in 5% of patients. Patients can be separated into low- and high-risk groups on the basis of patient age, grade of tumor, and extent and size of tumor (AGES); age, metastases, extent, and size (AMES); . Unfortunately, all the classification systems are based on postoperative findings. These classifications help predict tumor behavior, and the risk of death from thyroid cancer ( 5% in the low-risk group, versus 40% in the high-risk group ) Table :Classification of Low-versus High-Risk Patients Using the AGES System Variable Low Risk High Risk Age Women <50 years Women > 50 years Men <40 years Men > 40 years Poorly differentiated Grade Well differentiated Fibrous struma Insular, mucoid, columnar, and tall-cell variant Extent Confined to the thyroid Invasive to adjacent tissues or distant metastases Tumor with maximal diameter <4 Tumor with maximal diameter >4 cm cm AGES, Patient age and grade, extent, and size of tumor. Size Treatment : The recommendations is total or near total thyroidectomy when postoperative treatment with iodine-131 (I-131) is considered. Low-risk patients, who have papillary thyroid cancer of less than 1 cm, can be treated by thyroid lobectomy and isthmectomy; However, the benefits of total thyroidectomy include (1) the thyroid tissue is removed so that postoperative radioiodine scanning and ablative therapy can be effective, (2) serum thyroglobulin levels are more sensitive for detecting recurrent or persistent disease, (3) intrathyroidal cancer that is present in more than 50% of patients is removed, and (4) the small risk of a differentiated thyroid cancer becoming an undifferentiated cancer is decreased. Functional neck dissection ( lymph node dissection ) should generally be performed only in patients has clinical or sonographic evidence of lymph node involvement. Intraoperative enlarged lymph nodes in the central and lateral neck should be removed and submitted for frozen section. If positive, a formal lymph node dissection should be undertaken.Recurrence of papillary thyroid cancer can occur anytime during the patients' lifetime, thus lifelong surveillance is required. Unfortunately approximately one third of patients who develop recurrent thyroid cancer eventually die from it. 2) Follicular Thyroid Carcinoma Follicular cancer accounts for approximately 10% of all thyroid malignancies. Although follicular thyroid cancer can occur in any age group, these patients are typically older than are patients with papillary thyroid cancer group, usually in the sixth decade of life. As with papillary thyroid cancer, the female-to-male ratio is between 2:1 and 5:1. Follicular thyroid cancer usually presents as a slowly growing solitary thyroid nodule. Occasionally it has local symptoms. Rarely patients with follicular cancer present with symptoms of distant metastasis to the bone, lung, brain, and liver because these tumors, unlike papillary cancers, have a tendency to spread hematogenously. Less than 6% of follicular thyroid cancers metastasize to the cervical lymph nodes. The prognosis of follicular cancer is slightly worse than that for papillary cancer. Depending on the stage of the patient at presentation, overall survival ranges from 43% to 95% at 10 years. However, unlike patients with papillary thyroid cancers, those with follicular thyroid cancer who have not experienced recurrence within 12 years of their initial operation are usually cured. Therefore lifelong surveillance is not necessary. The important prognostic factors include the following: (1) presence of metastatic disease (2) older age (usually >40 years), (3) degree of invasion (microcapsular vs. angioinvasion with or without capsular and widely invasive), and (4) degree of tumor differentiation. FNAB is unable to distinguish benign from malignant follicular neoplasms because this technique evaluates cellular features. To distinguish benign from malignant follicular neoplasm, the whole specimen must be evaluated for vascular and capsular invasion. Because the diagnosis of follicular cancer cannot be made on FNAB, the recommendation isinitial operation is lobectomy and isthmectomy. Frozen sections are usually of limited utility in determination of malignancy. If the tumor has evidence of vascular invasion or is widely invasive on final pathology, the patient should undergo a completion thyroidectomy. some centers will and others will not perform a completion thyroidectomy if the patient has minimal capsular invasion. 3) Hurthle Cell Carcinoma Hurthle cell cancer accounts for approximately 3% of all thyroid cancers. As with follicular cancer, it has a peak incidence in the fifth and sixth decades. The female-to-male ratios range from 2:1 to 10:1. Radiation exposure, age, and familial Hurthle cell tumors are associated with an increased risk of these neoplasms. The 10-year survival of Hurthle cell carcinoma is 70%. Prognosis generally depends on extent of disease at the initial diagnosis and the extent of resection. Most patients with Hurthle cell neoplasms present with a solitary nodule. FNAB can reliably diagnose these neoplasms, but similar to follicular neoplasms, it cannot determine malignancy, which occurs in 35% of patients. Malignancy is determined by capsular or vascular invasion. In patients presenting with malignant lesions, 70% to 80% are confined to the gland, 10% to 20% have lymph node metastasis, and 15% have distant metastasis, most commonly to bone or lung. Careful surgical exploration should always be undertaken to detect the presence of obvious malignant disease. In patients with obvious malignant disease or contralateral nodular disease, or in patients with a history of childhood head and neck radiation, a one-stage total thyroidectomy is the preferred approach. For the routine patient with a solitary nodule, surgical management should consist of lobectomy and isthmectomy. Frozen section is unreliable in Hurthle cell neoplasm, similar to follicular neoplasm, and should be used judiciously. Lymph node dissection is indicated only for clinically or sonographically evident disease. 4) Medullary Thyroid Carcinoma Medullary thyroid cancer (MTC) accounts for 7% of thyroid cancers . Approximately 75% of the cases are sporadic, and 25% are hereditary. These tumors originate from c cells or parafollicular cells and may be associated with c-cell hyperplasia. Because of the location of the parafollicular cells, these tumors are almost always located laterally at the junction of the upper two thirds of the thyroid gland at approximately the level of the cricoid cartilage. In the sporadic form, there is usually a single focus of malignancy and unilateral disease in 85% of cases, compared with the hereditary form, in which the disease is multifocal and bilateral in 90% of cases and there is c-cell hyperplasia. MTC is associated with the RET proto-oncogene mutation. The hereditary forms of MTC are MEN 2A, MEN 2B, and familial MTC (FMTC). These causes of MTC all have point mutations in the RET proto-oncogene. A diagnosis of isolated FMTC is made when three or more cases are identified in a family without other associated endocrinopathies. Thus all patients with MTC should be RET proto-oncogene tested. Genetic testing and surgical treatment should begin no later than 5 years of age in MEN 2A and soon after birth in MEN 2B. The diagnosis is usually suspected on the basis of characteristic cytological features and the presence of immunostaining for calcitonin on FNAB specimen. Blood testing for calcitonin and CEA may also be informative. After the diagnosis of MTC is made, it is important to screen the patients for pheochromocytoma and hyperparathyroidism because 20% of patients have these associated conditions. Lymph node metastases are positive in 70% of patients with palpable disease. Serum markers for calcitonin support the diagnosis and correlate with tumor bulk, nodal, and distant metastasis. A calcitonin level greater than 1000 pg/ml after total thyroidectomy with no evidence of recurrence in the neck invariably indicates the presence of distant metastases (usually micrometastases in the liver). MTC can also metastasize to the lung and bone. High CEA levels correlate with a poorer prognosis. Prevention and cure of MTC is by surgery, Therefore surgeries for MTC should be performed in RET-positive patients with familial disease before age 6. A prophylactic central neck dissection is not necessary. Children with MEN 2B is classified as high risk and should have their thyroidectomy and central node dissection before 1 year of age or at diagnosis in those with an increased calcitonin. Children with MEN 2A and familial MTC without other endocrinopathies should have a total thyroidectomy and central node dissection by age 5. In sporadic MTC, a routine ipsilateral central and lateral functional lymph node dissection should be performed. MTC is not sensitive to radioiodine therapy. 5) Anaplastic Thyroid Carcinoma Fortunately anaplastic thyroid cancer (ATC) is a rare tumor, accounting for 1% to 2% of thyroid malignancies. Unlike well-differentiated thyroid cancer, ATC is invariably lethal and Survival is measured in months. ATC occurs most commonly within well-differentiated thyroid cancer; this transformation occurs in approximately 1% of patients with differentiated cancers. ATC occurs most commonly in patients older than 60 years and usually presents as a rapidly expanding thyroid mass that is firm to hard and frequently fixed. The tumor may compress the trachea and infiltrate the skin, causing overlying necrosis. Lymph node enlargement is frequent (84%) and early. Local tumor extension can cause fixation of the larynx, esophagus, and carotid vessels. Patients can present with hoarseness because of vocal cord paralysis resulting from direct extension. Symptoms such as dysphagia, dysphonia, and dyspnea are common. Systemic metastases occur in 75% of patients, usually involving the lungs, bone, brain, and adrenal glands. The diagnosis of ATC can be established by FNAB. The diagnosis of ATC must be differentiated from that of lymphoma and poorly differentiated medullary carcinoma. The standard form of treatment of thyroid cancer has been complete tumor removal, but in ATC, this maneuver is usually not curative because many patients present with distant metastases. Multimodality treatment consisting of radiation, chemotherapy, and then surgery, followed by further radiation and chemotherapy, provides the best results. Besides tumor resection, tracheostomy may be indicated for advanced disease. Unfortunately, the current treatments still have a limited role in the management of ATC because the majority of patients die within months of their diagnosis from local invasion or distant metastases. 6) Lymphoma Primary lymphomas of the thyroid are rare, accounting for only 1% to 2% of thyroid malignancies and less than 2% of extranodal lymphomas. Most thyroid lymphomas are non– Hodgkin's B-cell lymphomas. Thyroid lymphomas are predominantly associated with Hashimoto's thyroiditis and may be histologically difficult to distinguish from this chronic lymphocytic disease. The relative risk of lymphoma in these patients is 70 to 80 times higher than general population control individuals. Most patients present with a several-week history of a rapidly enlarging goiter and respiratory difficulty. Typically the patients are female in their seventh decade of life with a long-standing history of Hashimoto's thyroiditis. It is usually painless and often associated with hoarseness and dysphagia. Less commonly patients may present with tracheal compression. On physical examination, patients usually have a firm thyroid either unilateral or bilateral with possible fixation to adjacent structures. Lymphadenopathy is common. Clinically primary lymphoma poses a diagnostic and therapeutic challenge because it can present in a fashion similar to ATC. As a result, it is essential to distinguish these two entities because they have different therapeutic and prognostic implications. FNAB has helped distinguish these two conditions preoperatively and has decreased the need for open biopsy. Up to 88% of thyroid lymphomas are diagnosed on FNA alone, although core needle biopsy or open surgical biopsy may be warranted. Table : Staging for Thyroid Lymphoma Stage IE Localized disease within the thyroid Stage IIE Disease confined to thyroid and regional lymph nodes Stage IIIE Disease on both sides of diaphragm Stage IVE Disseminated disease Surgery plays a limited role in thyroid lymphoma unless the diagnosis is not established. Thyroid lymphomas have been shown to be both radiosensitive and chemosensitive; therefore most current recommendations are to treat these tumors with a combined modality therapy. Doxorubicin-based combination chemotherapy deceases the chance of distant metastasis. In B-cell lymphoma of mucosa-associated lymphoid tissue (MALT) of the thyroid, radiation alone has resulted in a 96% complete response, with only a 30% relapse rate. Advanced stage of the tumor, size greater than 10 cm, mediastinal involvement, and the presence of dysphagia are poor prognostic factors. Most recurrences occur within the first 4 years. The overall survival for primary thyroid lymphoma is 50% to 70%, ranging from 80% in stage IE to less than 36% in stage IIE and IVE source Current Surgical Therapy , J. L. Cameron, 9 th eddition, 2008 DR. S. ALDAQAL