POC-Varnier
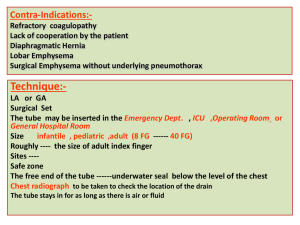
advertisement
Running Head: PLANNING THE CARE Planning the care of a patient with alteration in comfort related to chest tube removal and pain Laura M. Varnier Duke University School of Nursing 1 Planning the care Varnier 2 Clinical Database De-identified Patient Information: E. G. Patient's Age: 59 LOS: A&O X 4 Gender: F Reason for Admission: Five days s/p mechanical fall with right axillary pain; per pt, she attempted to get out of bed 5 days ago (6/24/2011) and “did not have her feet underneath her” and landed with a direct blow to her right axilla. ED report states pain and ecchymosis over the right axilla area and mild SOB with deep inspiration. Admitted 6/29/2011 with a hemopneumothorax approximately 40% with no airway compromise (I cared for pt on 7/4/2011). A pleural chest tube was placed into the rt pleural space and checked with chest xray. Past Medical History: Renal failure secondary to antineutrophilic cytoplasmic antibodies with positive membranous glomerulonephritis, HTN, migraine, diverticulosis, hyperlipidemia, anemia, and irritable bowel with colon polyps. Unique Code: Student Initials: L. V. Week: 5 Name of Agency: Duke 2300 Past/Recent Surgical Procedure: Chest tube placement (6/29/2011) checked with x-ray. Tonsillectomy at age 15 (February, 1967). Bone marrow transplant at 45 for sister with leukemia (November, 1997). Treatments: Chest tube placed in rt pleural space; TEDs and SCDs; fall precaution plan implemented; incentive spirometer. Assistive Devices: Bedside commode while hospitalized, no mobility device assistance needed. Advance Directives: Living Will: Yes Healthcare Power of Attorney: Yes Copy of AD in chart: Yes DNR Status: Full Code Source of Information: Patient Pertinent Diagnostic Tests--- Chest x-ray for tube placement (6/29/2011) and removal (7/4/2011). Pertinent labs (as of 7/4/2011): Calcium 8.2 (Normal 8.5-10.5 mg/dL), Hemoglobin 9.5 (Normal 12.0-15.5 g/dL for females), Hematocrit 0.29 (Normal 0.35-0.45 for females), RBC 2.73 (Normal 4.7-6.1 million/cu mm ), MCH 34.8 (Normal 26-34 pg), MCV 105 (Normal 80-100 fL ), BUN 41 (Normal 8-20 mg/dL), Creatinine 3.0 (Normal 0.6-1.2 mg/dL), Platelets 149,000 (Normal 150,000-450,000/cu mm). Pathology Report: negative for MRSA (6/30/2011), negative for VRE (6/30/2011). Infection Control: Standard precautions Allergies – food, environmental, mediations (indicate response for allergies): Erythromycin (stomach cramps), penicillin (swelling), shellfish (blotches and anaphylaxis) and sulfa/sulfonamides (rash). Medications: azathioprine (Imuran) (immunosuppressant for renal transplant candidates) 0.5mcg PO q DAY; calcitriol (calcium supplement for hypocalcemia related to renal failure) 50mg PO Q day; calcium carbonate (Tums Antacid) (calcium supplement for hypocalcemia due to renal failure) 1500 mg PO q DAY; clonazepam (Klonopin) (benzodiazepine for seizures prevention and anxiety management) 2 mg PO q HR; Planning the care Varnier 3 Lidocaine patch (topical analgesia for localized pain relief) 1 patch applied to site of pain (can be cut to fit), 12 hours on, 12 hours off; oxycodone (OxyContin) (moderate to moderately severe pain relief) 30mg PO BID; paroxetine hydrochloride (Paxil) (reduce anxiety and relieve depression) 30mg PO q DAY; temazepam (insomnia relief) 30mg PO q DAY; amlodipine/ hydrochlorothiazide/valsartan (hypertension) 40 mg PO q HR; docusate calcium (Senna) (stool softener for constipation with pain medication) 2 tabs PO BID; Lipitor (hyperlipidemia) 20mg PO q DAY; morphine (analgesia for moderate to severe pain during chest tube removal) PRN 4 mg IV. Activities of Daily Living/Level of independence: Prior to admission, pt denies any mobility restrictions or need for assistive devices; Pt states prior to admission that she completed ADLs independently; pt states that with her glasses she is able to see clearly; pt is able to hear and respond to verbal communication adequately. Pt reports a balanced vegetarian diet with a daily multivitamin, Calcium and Vitamin D supplementation. Psychosocial/ Cultural/ Spiritual Assessment: Prior to admission, pt was a very active veterinarian; Pt states she swims a mile each day and walks a mile every morning and night. Pt reports a strict vegetarian diet. Pt lives alone in a one story house with three dogs and five cats. Pt states that all other family members live in Texas, but that she has a “close knit group of friends and colleagues at work”. States that she adequately handles stressors and that her primary concern now is receiving new kidneys due to current renal failure. Pt denies dialysis for renal failure and stresses that her kidneys are not “in that bad of shape yet”. Pt enjoys reading, crossword puzzles, playing the piano and taking walks at night. Pt states that she is largely involved in her Methodist church community and arranges summer vacation Bible school activities. Pt states she spends about 20 hours a week involved with church activities. Risk Assessment: Low pressure ulcer risk with Braden score 22 and currently absent of pressures ulcers; High falls risk according to the Morse falls risk scale (score 75). Low risk for elopement according to Elopement Risk Assessment Scale. Low risk for nutritional deficiencies due to pt eating full meal, consuming nutritious snacks, active lifestyle, vegetarian diet and BMI of 18.9. Planning the care Varnier 4 Physical Assessment Findings Pt: E. G. Chief Complaints (subjective data): “I am in a lot of pain and I do not know why I need a chest tube.” Current Level of Independence: Full independence; pt states that with glasses she sees clearly; able to hear and respond to verbal commands; pt self turns Q 2 hours. Activity Order: OOB to walking; remove chest tube and get a follow up in 6 hours to monitor for spontaneous pneumothorax chest x-ray. Cardiovascular System Cap refill < 3 sec bilaterally in all extremities, nail bed color pink; S1, S2 audible, no audible S3 or S4 or murmurs; no edema; all pulses intact bilaterally in all extremities 2+. No audible bruits; No JVD at 45 degrees. Apical pulse RRR; no pulsations, lifts, or thrills. Gastrointestinal System No N/V. Flat contour; soft, nontender abdomen, active bowel sounds in all 4 quadrants; no guarding upon palpation; active flatus; last BM 7/4/2011; Vegetarian diet, feeds by mouth. Genitourinary System Frequently voids clear, yellow urine; output 200 mL at 0800 in bedside commode (at 0400 nurse stated she emptied 450mL from bedside commode). I=1400 mL, O=950 mL over 12 hour shift. Integumentary System Skin color appropriate for race, Braden score of 22 (low risk for pressure ulcers); Skin dry, intact, warm, no tenting or tenderness. No clubbing in nail beds. 20cm X 14 cm ecchymosis on right axilla noted; pain and guarding upon light palpation. IV Therapy (type/size, site/assessment, infusion) #1 18G Antecubital, saline-locked; patent. Student Nurse: Laura Varnier Height:_5’11’’ Weight: adm 135 Vital Signs: B/P 118/57 T 36.6 current 135 P 82 BMI: 18.9 R 20 Time: 0800 Respiratory System SpO2= 94% RA; Lt lobes CTA, Rt upper and middle lobes clear, diminished at right base; no cough, natural airway, relaxed depth, symmetric chest movement, breathing RRR; chest tube in rt pleural lateral space covered by a transparent dressing producing scant amount of pink thin watery serosangunious drainage, dressing CDI with no air leak, continuous wall suction and water sealed; Inspiration to expiration ratio 1:1; AP: Transverse 2:1. Neurological System A&OX4; awake, alert, calm, cooperative, follows tiered commands; CN 2-12 motor and sensory intact in all extremities; speech/voice clear. PERRL. Musculoskeletal System Active ROM in all extremities with no discomfort noted; L=R medium handgrips (2+), L=R strong dorsiflexion (3+); active movement, steady gait. EENT System Pt. wears glasses; PERRL, peripheral vision intact; no tearing; no vision lesions. Ears contained intact outer structures, no lesions or excess cerumen; conversational hearing intact. Nose mucosa pink and clear, no lesions or excess mucus, both nostrils patent. Lips pink and dry with no cracking. Mouth moist and pink, no lesions, good tonsillary pillar movement, no erythema. Teeth intact without dental caries, gums pink and moist, no tongue lesions; uvula midline; no dentures or hearing aids. Planning the care Varnier 5 Plan of Care- Physical COLLABORATIVE PROBLEM LIST Renal failure secondary to antineutrophilic cytoplasmic antibodies with positive membranous glomerulonephritis; HTN; migraine; diverticulosis; hyperlipidemia; anemia; irritable bowel with colon polyps; alteration in comfort related to chest tube removal and pain; ineffective pain management related to opioid use prior to admission; risk for falls related to previous hx of falls, opioid use and polypharmacology; impaired gas exchange related to decreased function of lung tissue; risk for injury related to chest tube movement limitations; alteration in nutrition related to ineffective pain management; risk for impaired skin integrity related to immobility and presence of chest tube; risk for osteoporosis related to postmenopause loss of estrogen; anxiety related to discharge. PRIORITY OF CARE Key Problem / Nursing Diagnosis (from Nursing Problem List): Alteration in comfort related to chest tube removal and pain. Supporting Subjective and Objective Data: “It hurts when I breathe. This tube is so annoying.” BP 118/57, pulse 87, RR 20, O2 sat 94% and pt reports an 8/10 pain rating. Patient is 10 days status post mechanical fall, 5 days status post chest tube placement; history of hemopneumothorax with chest tube placement. Pt respirations elevated above baseline data and patient appears in acute distress. GOALS General Goal to achieve through Nursing Interventions: E. G.’s pain will be effectively managed based on a patient-determined tolerance level; Pt pain will be adequately managed pre, intra, and post chest tube removal without respiratory compromise. Patient Behavioral Outcome Objective(s): The patient will report pain as tolerable on a 0-10 rating scale post chest tube removal; Pt will express satisfaction with pain management techniques; Pt will be able to participate in activities of daily living pre-intra-and-post-chest tube removal. The patient will remain free of signs of respiratory distress pre, intra, and, post chest tube removal, by observing respiration >12 per minute and O2 saturation level >90%. Patient Educational Needs: Pt. needs to be educated on the rational for a chest tube and the importance of the tube draining her pleural space posthemopneumothorax; pt education on importance of alerting medical staff at the onset of pain, not when the pain is unbearable; pt education on medication purpose, intended effects and side effects; pt education on chest tube removal procedure. Nursing Interventions (include frequency and specificity) Question the patient at beginning of the shift to establish a tolerable pain level goal according to the patient. PLAN AND INTERVENTIONS Scientific Rationale “The pain rating that allows the client to have comfort and appropriate function should be determined because this allows a tangible way to measure outcomes of pain management” (Griffie, 2003). Patient Response/Evaluation Patient established a tolerable pain level of 4/10. Pt reported pain fluctuated throughout the day from 2-10 out of 10. The highest pain reported occurred immediately after chest tube removal (reported at 10/10). Planning the care Assess and interpret vital signs Q 4 and PRN indicating an increase in pain, including increased heart rate, increased respirations, increased blood pressure, and physical signs of acute distress. Assess pain pre, intra, and post chest tube removal. Administer 30mg PO oxycodone PRN, according to MAR, for pain greater than 6/10 throughout chest tube placement and post-removal. Utilize a variety of complementary pain management techniques, such as repositioning. Administer PRN 4mg IV morphine, according to MAR, for analgesia prior to chest tube removal. Assess pt respiratory rate and O2 saturation 30 minutes and one hour post medication administration. Varnier 6 “The client’s report of the pain is considered the single most reliable indicator of pain” (JCAHO, 2010). “Pain measurements are determined by closely monitoring the patient’s other vital signs (heart rate, respiration, pulse, and temperature) as well as behaviors such as their level of agitation, irritation, and restlessness” (JCAHO, 2010). “Pain assessment is as important as taking vital signs, and the APS suggest applying the concept of pain assessment as the ‘fifth vital sign’” (APS, 2004). “Pharmacologic interventions are the cornerstone of management of moderate to severe pain” (APS, 2004). “Opioid analgesics are indicated for the treatment of moderate to severe pain” (APS, 2004). “Physical medicine approaches, such as the application of heat or cold, massage, exercise, and repositioning, may also be helpful in pain management” (Yates, Edwards & Nash, 2002). “Provide adequate analgesia prior to removal of chest tube” (Duke Nursing Process Standards, 2007). “If used correctly, either an opioid (morphine) or a nonsteroidal anti-inflammatory (ketorolac) can substantially reduce pain during chest tube removal without causing adverse sedative effects. Thus, clinicians may choose among several safe and effective analgesic interventions during chest tube removal” (Puntillo & Ley, 2004). At 0800, RR 20, BP 118/57, pulse 87 were all elevated above pt baseline. Pt reported highest pain of the day 8/10 (other than immediately post chest tube removal0. At 1200, RR 16, BP 110/60, pulse 62. At 1600, RR 16, BP 109/59, pulse 66 (immediately pre-chest tube removal). At 1800, RR 14, BP 115/72, pulse 62. Pt reports 8/10 pain at 0800, related to chest tube. Pt reports pain decline to 3/10 pain one hour after receiving 30mg oxycodone PO. Pt satisfied with pain management. Patient reported of pain of 6/10 1400; After repositioning patient to a side-lying position with the bed elevated to 30 degrees, patient reported pain at a reduced level of 4/10 at 1500. Pt provided with 4 mg IV morphine prior to chest tube removal. Pt reported pain 10/10 with chest tube removal (at 1600) but expressed approval of pre-medication regimen. At 1630, RR16, O2 saturation 95%. At 1700, RR 16, O2 saturation 96%. Planning the care Varnier 7 “… administering opioids or nonsteroidal antiinflammatory drugs based on the time of the peak effect of the analgesic medication has been a factor in reducing pain ratings immediately after and 20 minutes after CTR” (Friesner, Curry, & Moddeman, 2006). “An oxygen saturation level of less than 90% or a PaO2 of less than 80mm Hg indicates significant oxygenation problems” (Clark, Giuliano, & Chen, 2006). Instruct patient on the importance of notifying Return demonstration is one way to evaluate Patient return demonstrated use of call bell nurse of pain during onset of pain: Provided learning related to a psychomotor skill appropriately. Pt reported pain during first verbal instruction and demonstrated use call (Bastable, 2008). onset of symptoms and expressed approval at bell and asked for return demonstration. “It is easier to control pain when you prevent prompt nurse response time. it from gaining a foothold in the first place” (Stanik-Hutt, 2003). SUMMARY OF PATIENT PROGRESS/OVERALL EVALUATION OF GOALS What is your impression of your patient's progress toward goal from your nursing care? How might you change the plan of care to improve patient outcomes? E. G. mostly maintained effective pain management throughout pre, intra and post chest tube removal assessments. Pt expressed satisfaction with pain management throughout different employed techniques Patient positively progressed through each nursing goal and complied with suggestions, initiating her steps towards a successful recovery. To improve my plan of care, I would like to incorporate deep breathing techniques when appropriate into the chest tube removal process, to ease pain and anxiety experienced by my patient. Furthermore, a wider range of pain management strategies, throughout my shift, would have been beneficial to incorporate in my patient care, such as listening to music and incorporating distractions. Furthermore, if my patient’s pain remained inadequately managed throughout the day, I could have collaborated with the team and requested a pain consult, as well. Planning the care Varnier 8 Psychosocial COLLABORATIVE PROBLEM LIST Renal failure secondary to antineutrophilic cytoplasmic antibodies with positive membranous glomerulonephritis; HTN; migraine; diverticulosis; hyperlipidemia; anemia; irritable bowel with colon polyps; alteration in comfort related to chest tube removal and pain; ineffective pain management related to opioid use prior to admission; risk for falls related to previous hx of falls, opioid use and polypharmacology; impaired gas exchange related to decreased function of lung tissue; risk for injury related to chest tube movement limitations; alteration in nutrition related to ineffective pain management; risk for impaired skin integrity related to immobility and presence of chest tube; risk for osteoporosis related to postmenopause loss of estrogen; anxiety related to discharge. PRIORITY OF CARE Key Problem / Nursing Diagnosis (from Nursing Problem List): Anxiety related to discharge planning. Supporting Subjective and Objective Data: “I am nervous about going home. I am do not know who will take care of me when I go home.” Patient is 10 days status post mechanical fall, 5 days status post chest tube placement; history of hemopneumothorax with chest tube placement. Pt appears anxious and pre-occupied prior to discharge teaching. GOALS General Goal to achieve through Nursing Interventions: Demonstrate significant decrease in physiologic, cognitive, behavioral and emotional symptoms of anxiety. Patient will report that anxiety is reduced to a manageable level. Patient Behavioral Outcome Objective(s): The patient will verbalize specific fears and apprehensions about going home by herself in order for these areas to be addressed. The patient will demonstrate an understanding of discharge instructions. Pt will identify methods of anxiety management specific to her. Pt will identify support system for care throughout beginning days of discharge. Patient Educational Needs: Education on support groups in the area for other transplant candidates; education on who needs to be contacted in case she has questions, including the chain of command to follow in the event of an emergency; Educate patient on role and function of social worker in discharge planning. PLAN AND INTERVENTIONS Nursing Interventions Scientific Rationale Patient Response/Evaluation (include frequency and specificity) Assess client’s worries and apprehensions “Specific labeling helps the client to isolate Pt states prior to discharge that she is worried surrounding discharge by questioning, preanxiety as a feeling that the client can begin to about going home by herself, although she will and-post discharge teaching. understand and manage” (Fortinash & be having friends check on her throughout her Holoday-Worret, 1999). discharge. Pt states she is concerned about caring for her animals at home and returning to her job. Pt states she is worried about how much her hospital stay will cost and expresses Planning the care Varnier 9 Collaborate with the social worker to address specific needs regarding parking tickets and paying for other hospital services, upon request from the patient. “Findings show that the involvement of a discharge planning case manager is related to a significant reduction in unmet treatment needs…” (Mamon, Steinwachs & Fahey, 1992). Assess client’s verbal and non-verbal anxiety cues surrounding anxiety, both pre-and-post discharge teaching. “Early recognition of anxiety is critical to prevent escalation of symptoms and loss of control” (Fortinash & Holoday-Worret, 1999). “The client’s knowledge of his or her typical responses to anxiety-producing stimuli assists the client to begin to manage them” (Fortinash & Holoday-Worret, 1999). Assess patient’s support system outside of the hospital by questioning, as well as assistance for follow up care, prior to discharge. “Three main barriers to discharge were found: having an unstable or complex medical condition, lacking family or social support, and being unable to obtain suitable housing. Intervention staff advocated on the behalf of clients, encouraged clients to build skills toward independent living and contributed extensive knowledge of local resources to advance client goals. Cases of successful transition suggest that a person-centered approach from intervention staff combined with a flexible organizational structure is a promising model for future interventions” (Meador, Chen, & Schultz, 2011). concern regarding the payment of 6 parking tickets for the last 6 days she has been in the hospital. Post-discharge, patient states that she is “less worried about being at home by herself and taking care of herself.” Pt expressed satisfaction in meeting with the social worker and getting her parking and payment questions answered. Pt also requested follow up contact information in order to remain in touch with the social worker after she is discharged. Client seemed consistently distracted, preoccupied and avoidant until receiving clear answers to her question. Student nurse identified these non-verbal anxiety cues to the patient and the patient recognized the cues. Student nurse and patient collaborated ideas to verbally request information and answers to allow for less distraction and avoidance and enable focus on discharge planning and teaching. Pt states that that she has a group of colleagues from work, friends in her neighborhood and members of her church which can check on her throughout her first days after discharge. Pt colleague from work also attends discharge teaching and expresses interest in helping her friend after discharge. Pt states that her friend will be with her at all follow up doctor appointments. Planning the care Varnier 10 “Different types of activities including Pt expressed stress relief with physical activity domestic (housework and gardening), walking including swimming and walking. Pt states that and sports were all independently associated she will incorporate these activities into her with lower odds of psychological distress” discharge to help relieve anxiety. (Hamer, Stamatakis & Steptoe, 2009). SUMMARY OF PATIENT PROGRESS/OVERALL EVALUATION OF GOALS What is your impression of your patient's progress toward goal from your nursing care? How might you change the plan of care to improve patient outcomes? Discuss activities the patient may incorporate post-discharge, as needed, to help ease patient tension and anxiety. When I began working with my patient, I could not effectively implement my care due to her preoccupation with discharge planning. I feel that by addressing her anxiety/fears and allow for verbalization and acknowledgement of these concerns, together, we were able to begin effective discharge planning. I feel that my patient did progress to meet the goals that we collaboratively set. To change this plan of care, I would hope to be involved in the discharge process earlier. My patient’s initial concerns were not brought up until the doctor had placed the discharge orders and her departure was set to occur within the hour. I would like to have spoken more comprehensively about her concerns, but I feel that we did address a majority of anxieties she had and put a plan in place to manage each concern effectively. Planning the care Varnier 11 Chest Tube Removal: Can anything other than opioids effectively manage pain? One of the most reported stressors when a patient undergoes placement of a chest tube is how painful the experience will be when the tube must be removed (Puntillo & Ley, 2004). Within the Duke Protocol it is recommended that nurses “provide adequate analgesia to the patient prior to removal of the chest tube” (Duke Nursing Process Standards, 2007). The Duke University protocol does not specify the type, amount or form in which the analgesia should be prescribed; this is determined by the health care practioners licensed to prescribe medical therapy (2007). Regarding my patient, a standing order for 4 mg IV morphine with chest tube removal (CTR) was prescribed. However, as highlighted by Friesner, Curry and Moddeman, “although opioids are traditionally used to treat acute pain, they are not associated with optimal pain control during CTR” (2006). In a randomized control study of 40 hospitalized patients conducted by Friesner, Curry, and Moddeman, effectiveness of opioid-only management in 21 participants versus an opioid paired with focused breathing exercises in 19 participants was evaluated to determine the differences in pain levels throughout chest tube removal (2006). The focused breathing exercises directly preceding chest tube removal involved five minutes of inhaling through the nose and pursed-lip exhalation. Pain levels were assessed in the treatment and control groups pre-CTR, immediately following CTR and 15 minutes following CTR using the vertical Visual Analog Scale (VAS). Before CTR, the mean VAS pain rating, on a 0-10 scale for the treatment group was 5.05 (SD 2.86) and 5.04 for the control group (SD 2.44). Immediately after CTR, the mean rating was 6.57 (SD 2.61) for the treatment group and 8.61 (SD 2.96) for the control group. Fifteen minutes post-CTR, the mean rating for the treatment group was 3.07 (SD 2.45) and 5.57 for the control group (SD 2.96) (Friesner, Curry & Moddeman, 2006). The researchers Planning the care Varnier 12 determined that pain intensity ratings were consistently lower for patients receiving focused breathing exercises and opioids compared to the control group receiving opioids only. As an active member watching the chest tube removal procedure and as an advocate for my patient, I would like to encourage prescribers and hospital authorities to investigate the evidence regarding focused breathing techniques to assist in managing pain levels throughout the chest tube removal process. To provide the best care for our patients, we need to investigate the most appropriate, evidenced-based information for pain management during CTR and begin implementing comprehensive pain management techniques into hospital-wide policy. Planning the care Varnier 13 References Ackley, B. & Ladwig, G. (2008). Nursing diagnostic handbook: an evidence-based guide to planning care. St. Louis, MO: Mosby, Inc. American Pain Society. (2004) Pain: current understanding of assessment, management and treatments. Accessed 7/12/2011. Retrieved from www.ampainsoc.org/ce/npc. Bastable, S. B. (2008). Nurse as educator: principles of teaching and learning for nursing practice. Sudbury, MA: Jones and Bartlett Publishers. Clark, A. P., Giuliano, K., Chen, H. M. (2006). Pulse oximetry revisited: “but his O (2) sat was normal!” Clinical Nurse Specialist, 20, 268-272. Duke Nursing Process Standards (2007). Chest tube procedure and protocol. Durham, NC: Duke University Health System. Fortinash, K. & Holoday-Worret, P. (1999). Psychiatric nursing care plans. St. Louis, MO: Mosby, Inc. Friesner, S. A., Curry, D. M., & Moddeman, G. R. (2006). Comparison of two pain-management strategies during chest tube removal: Relaxation exercise with opioids and opioids alone. Heart & Lung, 35, 269-276. Retrieved from http://www.consensusconference.org/data/Upload/Consensus/1/pdf/799.pdf. Griffie, J. (2003). Pain control: addressing inadequate pain relief. American Journal of Nursing, 103, 61-63. Planning the care Varnier 14 Hamer, M., Stamatakis, E., & Steptoe, A. (2009). Dose-response relationship between physical activity and mental health: the Scottish Health Survey [Abstract]. British Journal of Sports Medicine, 43, 1111-1114. Retrieved from http://web.ebscohost.com.proxy.lib.duke.edu/ehost/detail?vid=3&hid=107&sid=ab5bdc5 2-cfff-4644-ab7afa75c2c86ae3%40sessionmgr12&bdata=JnNpdGU9ZWhvc3QtbGl2ZQ%3d%3d#db=rzh &AN=2010495944. The Joint Commission on Accreditation of Healthcare Organizations (2010). Approaches to pain management: an essential guide for clinical leaders. Oakbrook Terrace, IL: Joint Commission Resources, Inc. Mamon, J., Steinwachs, D. M., & Fahey, M. (1992). Impact of hospital discharge planning on meeting patient needs after returning home. Health Services Research Journal, 27, 155175. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1069871/. Meador, R., Chen, E., & Schultz, L. (2011). Going home: identifying and overcoming barriers to nursing home discharge. Care Management Journals, 12, 208-213. Retrieved from http://pm6mt7vg3j.search.serialssolutions.com/OpenURL_local?sid=Entrez:PubMed&id =pmid:21413534. Puntillo, K. & Ley, S. J. (2004). Appropriately timed analgesics control pain due to chest tube removal. American Journal of Critical Care, 13, 292-302. Retrieved from http://ajcc.aacnjournals.org/content/13/4/292.abstract. Stanik-Hutt, J. A. (2003). Pain management in the critically ill. Critical Care Nurse, 23, 99-103. Retrieved from http://ccn.aacnjournals.org/content/23/2/99.short. Planning the care Varnier 15 Yates, P., Edwards, H., & Nash, R. (2002). Barriers to effective cancer pain management: a survey of hospitalized cancer patients in Australia. Journal of Pain and Symptom Management, 23, 393-405. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12007757.