Health Assessment - ePortfolio of Sarah E. Wild
advertisement

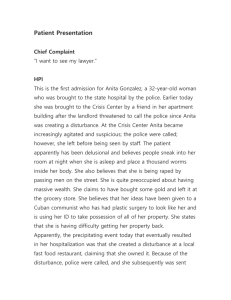
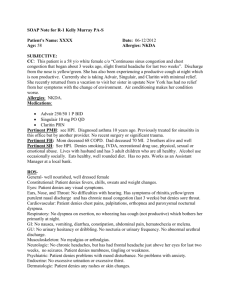
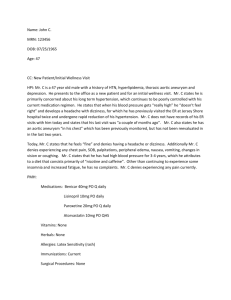
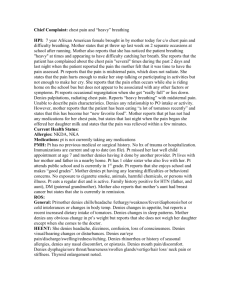
Health Assessment System being assessed: Respiratory Chief Complaint: Shortness of breath History of present illness: The patient has been experiencing shortness of breath for about a week now but it got worse today. She has a dry nonproductive cough that causes tightening in her chest. She has noticed that her peak flow levels have decreased. When she sittings she is okay but her shortness of breath increases with activity. She used Proventil about an hour ago but it did not help her symptoms. She rates her shortness of breath a 9/10 and has a hard time speaking full sentences. This patient has been to the ER twice in that past week for asthma exacerbations. She denies fever and chills. Medications: Beclomethasone 80mcg inhaled PO twice a day (last taken at 0600), Serevent Diskus 50mcg inhaled PO twice a day (last taken at 0800), Proventil 2mg inhaled PO twice a day (last taken at 1000), Ibuprofen 400mg PO every 6 hours PRN (last taken 0900), denies use of herbal medications and other OTC medications, Doesn’t used O2 at home. Allergies: Denies allergies to any medications, has environmental allergies (she gets a runny nose) Past Medical History: Asthma, denies TB, Cancer, emphysema, and pneumonia. Had a chest Xray, PFT, and Bronchoscopy Past Surgical History: Denies any surgery on chest, ears, nose, and throat. States “I had a bronchoscopy several years ago” Family History: Denies family history of respiratory problems, cancer TB, emphysema, cystic fibrosis, asthma, COPD Social History: Denies Smoking, recreational drugs, and alcohol. Lives at home with husband and 3 children. Does not have any pets. Has not traveled out of the US except to Sweden 4 months ago. Has forced air heat. General Survey: This is a 33 year old female appears stated age, dressed appropriate for weather, well groomed with appropriate makeup. Sitting upright in chair appears short of breath, makes eye contract, mood happy, affect is congruent to mood. Follows commands. Is alert and oriented to person, place, time, and situation. PERRL. Speech clear, speaks in sentences but needs frequent breaks for air. Temperature 98.4 degrees Fahrenheit, Pulse 90 and regular, BP 140/70, respiration 24 and labored, O2 saturation 94%. Review of Systems: Skin is pink, dry, and warm. Lips pink with moist mucus membranes. No rash, lesions, sores, bruises, or wounds noted. Nail beds are pink with capillary refill <2 seconds. No clubbing of nails noted. Denies headaches, vertigo, or syncope. Denies head trauma. Denies stiffness and any limitation of movement in the neck. Eyes are blue with 5mm pupils that are equal, round, and reactive to light. Denies any vision changes and problems with her eyes. Conjunctivae pink. Denies any pain, ringing, or discharge form the ears. Denies any nose bleeds, states “I have allergies that cause my nose to be runny”. No JVD or lymph node enlargement noted. Breasts are free of pain, discharge, masses, lumps, and edema. There are rhonchi in the right upper lobe with wheezes throughout bilaterally, with apparent shortness of breath. Has a dry nonproductive cough. Heart sounds are regular with s1 and s2 sounds present. Denies palpitations. Abdomen is soft, flat, non-distended, without tenderness. Bowel sounds present in all four quadrants. States last BM was last night, soft, brown, and formed. Denies any nausea or vomiting. Denies any pain, burning, or difficulty voiding. States last menses was 2 weeks ago. Denies any pain, redness, or discharge from the genitalia. Denies any muscle twitching, pain, weakness, or cramping. Joints are free of swelling and edema. Moves all four extremities without pain. Steady gait. Neurological system is intact. Denies any paresthesis, pain, and cognitive changes.