Melissa Morris Level III Project Lit Review DNAR Lock-and
advertisement

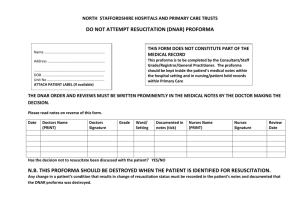
Melissa Morris Level III Project Lit Review DNAR Lock-and-Key Language Literature Review: DNAR Lock-and-Key Language Title of Article And Citation Conflicting Perspectives Compromising Discussions On Cardiopulmonary Resuscitation (Groark, Gallagher, & McGovern, 2010). LOE 6 Take Away Points and Quotations Groarke, J., Gallagher, J., & McGovern, R. (2010). Conflicting perspectives compromising discussions on cardiopulmonary resuscitation. The Irish Medical Journal 103(8), 233-235. LOE 6. Nurses’ perceptions of attempting cardiopulmonary resuscitation on oldest old patients (Sævareid & Balandin, 2011) Sævareid, J.T. & Balandin, S. (2011). Nurses’ perceptions of attempting cardiopulmonary resuscitation on oldest old patients. 6 Only 16% of patient will survive to discharge following an in-hospital resuscitation from cardiopulmonary arrest. “An observational study was carried out to examine the knowledge and opinions of doctors, nurses and the general public on various aspects of resuscitation”. “70% of doctors, only 24% of nurses and no person from the general public group correctly estimated survival to discharge after in-hospital cardiopulmonary resuscitation attempts at less than 20%”. Of questions answered by the general public, 67% incorrectly equated cardiopulmonary arrest to a heart attack; 42% did not think drugs or intubation were used in resuscitation attempts; and 58% cited TV medical dramas as their primary source of information regarding resuscitation attempts. “The general public significantly overestimate the success of CPR attempts while nurses and doctors also do so, but to a lesser extent”. “Doctors and nurses must be definite on the ethics involved before embarking on resuscitation discussions. Doctors can be deficient in initiating resuscitation discussions and decisions. Training in areas such as survival, ethics, and communication is needed. Failure to address these deficiencies will violate an ethical and legal responsibility to ensure patients a dignified and comfortable death”. Usually, nurses are the healthcare professionals who find patients in cardiac arrest, and are the ones who start CPR, but physicians are responsible for writing DNAR orders. Because nurses want to participate in DNAR decisionmaking, but do not want to take full responsibility in the decision-making process, interdisciplinary collaboration should be used for decisions about end-of-life treatment. Laws about DNAR status vary from country to country. The Norwegian Nurses Organization states that nurses are responsible for providing care that alleviates suffering and contributes to ensuring a dignified death. Because of this, many nurses experience ethical dilemmas if no DNAR is in place, but the patient is perceived to be suffering or at risk of an undignified death. Melissa Morris Level III Project Lit Review DNAR Lock-and-Key Language Journal of Advanced Nursing 67(8), 1739-1748. LOE 6. http://www.colorado.gov/ 8 cs/Satellite/CDPHEEM/CBON/125158973863 6 (LOE 8) 6 Do not attempt resuscitation: the importance of consensual decisions (Imhofa, MahrerImhofa, Janischb, Kesselringc, & Zuercher Zenklusend, 2011). Imhofa, L., Mahrer-Imhofa, R., Janischb, Kesselringc, A., & Zuercher Zenklusend, R. (2011). Do not attempt resuscitation: the importance of consensual decisions. Swiss Medical Weekly, 141, w13157. LOE 6. Junior physicians also experience stress while attending cardiac arrests. “Slow codes” can occur because of pressure by patients’ families, failure to have a written DNAR order, fear of litigation, and fear of harming patients by discussing code status; this may increase nurses’ anxiety about end-of-life decisions. “Physicians may follow a disease-centered method of treating patients and experience more difficulty in adapting to a palliative or patient-centered approach than nurses.” “The aim of the study was to explore nurses’ thoughts and attitudes about CPR of the oldest old patients”. “The participants perceived that the amount and quality of information given to patients and family [caregivers] about CPR and DNAR varied across different physicians”. “All participants stressed that they wanted to respect their patients’ wishes. When reflecting on what is important in determining DNAR, nine of the ten participants mentioned autonomy and noted that often the patients would not want to be resuscitated… Nevertheless, respect for patient autonomy was one reason for not wanting an age limit for CPR”. Limitation to study was that it was conducted in Norway, where patients cannot decide against CPR unless they are dying. Information from the Colorado Department of Public Health and Environment: Emergency Medical and Trauma Services (CPR Directives) “Yet, in daily clinical practice, patient involvement, specific professional responsibilities and communication between professionals regarding DNAR orders remain a major challenge”. DNAR discussions can be difficult because everything is based on hypothetical facts and scenarios; informed consent for DNAR orders can be difficult. “International guidelines further state that DNAR orders should include the coordinated expertise of interdisciplinary teams. Observations by nurses may be crucial and the importance of their input in the decisionmaking process is increasingly recognized. However, nurses still report frequent exclusion from CPR decisions”. Participant physicians reported DNAR discussions should be held by chief physicians; and participant nurses reported that nurses should be able to participate, but a lot of clinical experience would be required to do so. Melissa Morris Level III Project Lit Review DNAR Lock-and-Key Language “The descriptions by the participants showed that CPR/DNAR decisions are the product of three distinct decisional phases: 1) the phase of implicit decision, 2) the phase of explicit decision, and 3) the phase of reconsidering decisions”. “Whereas CPR/DNAR orders were discussed on a daily basis in most intensive care units, reluctance to consider new orders was remarkable on surgical wards” “Well-accepted decisions typically combined profound, mutually respected medical and nursing expertise, communication and negotiation skills, common sense and life experience coupled with empathy for patients and colleagues”. “A consensus did not mean that all team members had to share the same opinion, but that the expertise and perspectives of different members of the team had become part of the decision”. References Groarke, J., Gallagher, J., & McGovern, R. (2010). Conflicting perspectives compromising discussions on cardiopulmonary resuscitation. The Irish Medical Journal 103(8), 233-235. LOE 6. http://www.colorado.gov/cs/Satellite/CDPHE-EM/CBON/1251589738636. LOE 8 Imhofa, L., Mahrer-Imhofa, R., Janischb, Kesselringc, A., & Zuercher Zenklusend, R. (2011). Do not attempt resuscitation: the importance of consensual decisions . Swiss Medical Weekly, 141, w13157. LOE 6. Sævareid, J.T. & Balandin, S. (2011). Nurses’ perceptions of attempting cardiopulmonary resuscitation on oldest old patients. Journal of Advanced Nursing 67(8), 1739-1748. LOE 6.