Cardiovascular system – blood vessels and circulation
advertisement
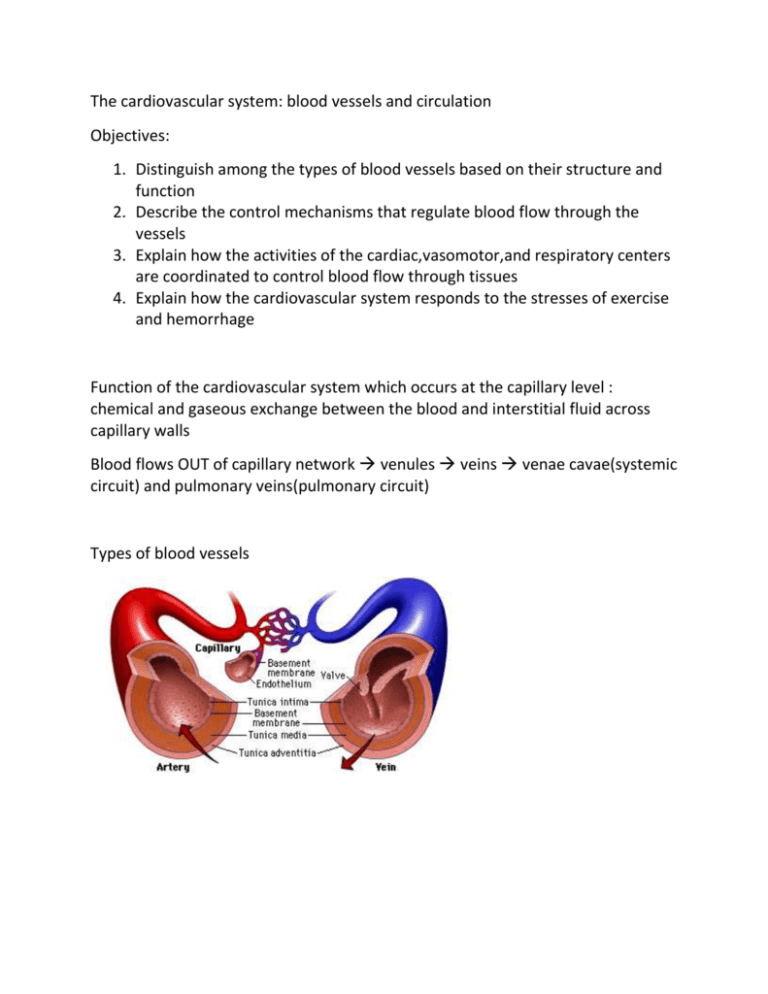
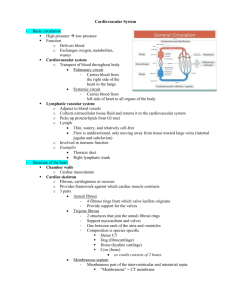
The cardiovascular system: blood vessels and circulation Objectives: 1. Distinguish among the types of blood vessels based on their structure and function 2. Describe the control mechanisms that regulate blood flow through the vessels 3. Explain how the activities of the cardiac,vasomotor,and respiratory centers are coordinated to control blood flow through tissues 4. Explain how the cardiovascular system responds to the stresses of exercise and hemorrhage Function of the cardiovascular system which occurs at the capillary level : chemical and gaseous exchange between the blood and interstitial fluid across capillary walls Blood flows OUT of capillary network venules veins venae cavae(systemic circuit) and pulmonary veins(pulmonary circuit) Types of blood vessels Structure of Vessel walls The walls of arteries and veins: (lumen- open space inside BV) 1. Tunica intima: innermost lining – endothelium and CT with high % of elastic fibers 2. Tunica media – smooth muscle tissue in a framework of collagen and elastic fibers 3. Tunica externa – a sheath of CT around vessel – collagen fibers intertwine with surrounding tissues to “anchor” the BV Vasoconstriction and vasodilation – controlled by Autonomic system – Arteries 1. Elastic arteries – LARGE, RESILIENT – diameters up to 2.5cm Examples: aorta, pulmonary trunk including the aorta and pulmonary trunk branches Tunica media is DOMINATED by ELASTIC FIBERS not smooth muscle Able to absorb the demand of the pressure changes during cardiac cycle Notice all of the elastic fibers! 2. Muscular arteries – medium sized arteries(distribution arteries) – distribute blood to skeletal muscle and internal organs Diameter approximately - .4cm Example: external carotid arteries Less elastic fibers more smooth muscle cells 3 arterioles – internal diameter – 30um Tunica media – 1-2 layers of smooth muscle cells Arteriosclerosis – (skleros = hard) a hardening/thickening of arterial walls Cause – coronary artery disease and strokes 2 forms Focal calcification: loss of smooth muscle in tunica media replaced by calcium deposits – result of aging and complications of diabetes Atherosclerosis – lipid deposits in tunica media due to damage to endothelial lining Cause: increased blood cholesterol (LDL and HDL – both formed in liver – not due to amount of triglycerides! LDL shuttles cholesterol to peripheral tissues from liver; HDL shuttles cholesterol from peripheral tissues to liver for storage. LDL can end up in arterial “plaques” = “bad” cholesterol) Monocytes in blood try to remove the excess cholesterol rich LDL, and “fill-up”, slow down and attach to endothelial wall – vessel thickens = atherosclerosis CARDIOVASCULAR REGULATION INVOLVES AUTOREGULATION, NEURAL MECHANISMS, AND ENDOCRINE RESPONSES 1. AUTOREGULATION: a change in tissue condition activates precapillary sphincters to change pattern of blood flow 2. NEURAL MECHANISMS: respond to arterial pressure or blood gas levels – autonomic CAPILLARIES Allow exchange of materials between blood and interstitial fluids No tunica media; no tunica externa Diameter = diameter of RBC = 8um Water, small solutes, lipid-soluble materials easily diffuse (exception : the capillaries of the choroid plexus of brain, hypothalamus, and glomerulus of kidneys – small pores in wall to allow for protein diffusion) Capillary beds: the functional structure of capillaries – Single arteriole gives rise to dozens of capillaries which become venules Precapillary sphincter – controls amount of blood entering capillary bed at any given time – located at beginning of each capillary in capillary bed Arteriovenous anastomosis – a vessel that connects an arteriole to a venule – bypassing a capillary bed “Insurance policy” – if an artery is blocked or compresses, others can continue to supply blood to capillary bed preventing tissue damage Common in brain, coronary circulation and others VEINS Collect blood from all tissues and organs and return to heart Venules – smallest resemble capillary – very small – no tunica media Medium size veins- resemble muscular arteries – 2mm-9mm diameter Tunica media – layers of smooth muscle Tunica externa – elastic and collagen fibers Limbs – valves to prevent backflow of blood Large veins – 2 venae cavae and their “tributaries” in thoracic and abdominopelvic cavities - Tunica media thinner than tunica externa Thin walls relative to arteries Varicose veins / hemorrhoids = valves weaken, blood pools in vein Blood pressure – arterial pressure Systolic pressure – peak blood pressure(ventricular systole) Diastolic pressure – minimum BP(ventricular diastole) “normal” BP = 120/80 Pulse – rhythmic pressure which accompany each heartbeat Pulse pressure – difference between SP and DP Decreases as distance from heart increases Measures 35mmHg when blood reaches precapillary sphincter Forces acting against capillary walls At anterior end of capillary filtration occurs – near venule, fluid is reabsorbed movement is into and out of the lymphatic vessels 3.6 L of water and solutes flow through peripheral tissues into lymphatic vessels and back into the bloodstream 4 functions of capillary exchange 1. 2. 3. 4. Communication between blood plasma and interstitial fluids Distribute nutrients, hormones, dissolved gases Aid in movement of insoluble lipids and tissue proteins Flush bacterial toxins and other stimuli to lymphoid tissues and organs of immunity Edema: abnormal accumulation of interstitial fluid Pulmonary edema: congestive heart failure – Left ventricle can’t keep pace with right ventricle – blood flow becomes “congested” in pulmonary circuit – results in build up of fluid in lungs “recall of fluids” – during blood loss or extreme dehydration – movement of water from interstitial fluid into blood stream to increase blood volume Shock – acute circulatory crisis marked by low blood pressure – “acute = sudden in onset, severe in intensity, brief in duration” Potentially fatal – as vital tissues are starved for oxygen Circulatory shock – 30% reduction in total blood volume Symptoms: 1. 2. 3. 4. 5. 6. Hypotension BP lower than 90mm Hg Skin = pale, cool, moist Confusion/disorientation – drop in BP in brain Rise in heart rate/rapid, weak pulse Cessation of urination Acidosis – due to lactic acid generation in oxygen deprived tissues Types of: Septic shock, such as toxic shock syndrome, and anaphylactic shock – all due to a widespread uncontrolled vasodilation – similar in effect and consequences to circulatory shock THREE GENERAL FUNCTIONAL PATTERNS OF BV 1. Distribution of arteries and veins on left and right side of body – identical a. Example: right subclavian , axillary, brachial, and radial arteries parallels left subclavian, axillary, brachial and radial arteries 2. BV have multiple name changes as they pass different anatomical boundaries: external iliac artery(trunk) becomes femoral artery(thigh) 3. Tissues and organs usually serviced by several arteries/veins CARDIOVASCULAR REGULATION INVOLVES AUTOREGULATION, NEURAL MECHANISMS, AND ENDOCRINE RESPONSES 1. AUTOREGULATION: a change in tissue condition activates precapillary sphincters to change pattern of blood flow 2. NEURAL MECHANISMS: respond to arterial pressure or blood gas levels – autonomic nervous system(cardiac center and vasomotor center of medulla oblongata) adjust cardiac output and peripheral resistance to maintain adequate blood flow 3. Endocrine mechanisms – release of hormones a. Epinephrine and norepinephrine – suprarenal glands – stimulate cardiac output and vasoconstriction b. ADH – pituitary gland – vasoconstriction, kidneys conserve water as a response to low blood volume c. Angiotensin II – formed in blood activated by renin(enzyme) . in response to low BP – i. stimulates cardiac output and arterial constriction ii. stimulates production of ADH iii. stimulates “thirst” iv. stimulates production of aldosterone – reabsorb water from kidneys d. erythropoietin – hormone in kidneys activates bone marrow to produce RBC e. atrial natriuretic peptide(ANP) – produced by cardiac muscle cells in wall of right atria – reduces blood volume/BP by blocking release of ADH, aldosterone, E, and NE Exercise and cardiovascular system 1. extensive vasodilation – as rate of oxygen consumption in skeletal muscles increases – increasing blood flow into capillaries 2. venous return increases – increased skeletal muscle contractions and increased breathing blood pulled into “respiratory pump” of heart 3. cardiac output rises – due to increased venous return – benefits of modest( jogging 5 miles/week) exercise program: lower blood cholesterol reduction in stress lowers blood pressure slows plaque formation moderate exercise can cut risk of heart attack by 50%