Good Morning
advertisement
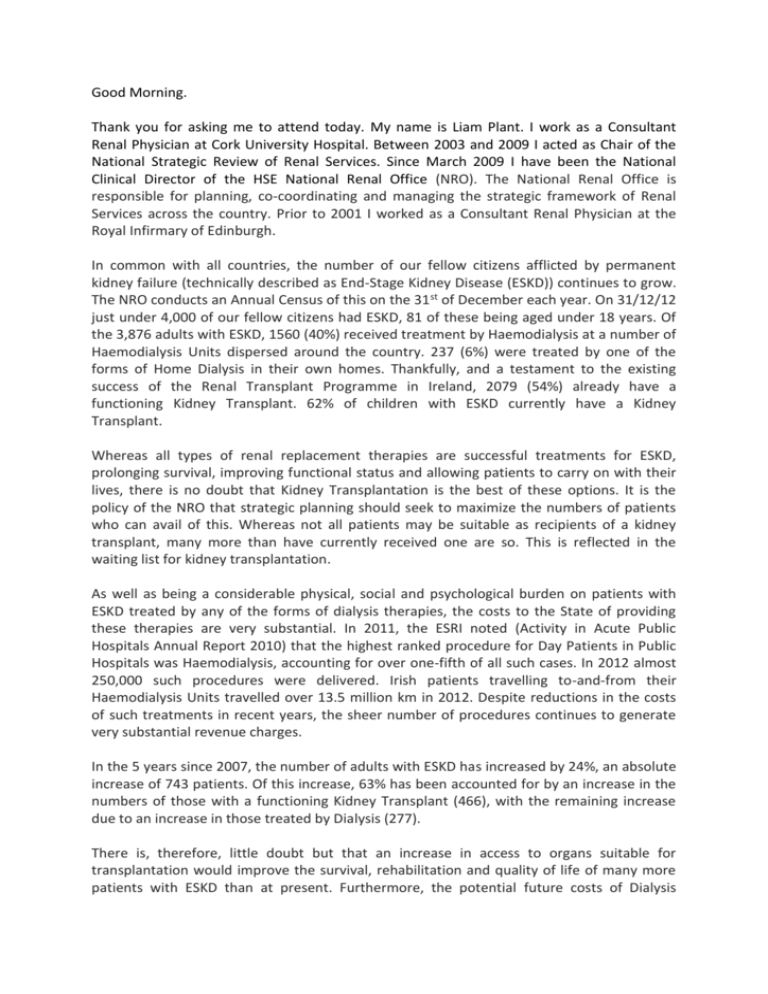
Good Morning. Thank you for asking me to attend today. My name is Liam Plant. I work as a Consultant Renal Physician at Cork University Hospital. Between 2003 and 2009 I acted as Chair of the National Strategic Review of Renal Services. Since March 2009 I have been the National Clinical Director of the HSE National Renal Office (NRO). The National Renal Office is responsible for planning, co-coordinating and managing the strategic framework of Renal Services across the country. Prior to 2001 I worked as a Consultant Renal Physician at the Royal Infirmary of Edinburgh. In common with all countries, the number of our fellow citizens afflicted by permanent kidney failure (technically described as End-Stage Kidney Disease (ESKD)) continues to grow. The NRO conducts an Annual Census of this on the 31 st of December each year. On 31/12/12 just under 4,000 of our fellow citizens had ESKD, 81 of these being aged under 18 years. Of the 3,876 adults with ESKD, 1560 (40%) received treatment by Haemodialysis at a number of Haemodialysis Units dispersed around the country. 237 (6%) were treated by one of the forms of Home Dialysis in their own homes. Thankfully, and a testament to the existing success of the Renal Transplant Programme in Ireland, 2079 (54%) already have a functioning Kidney Transplant. 62% of children with ESKD currently have a Kidney Transplant. Whereas all types of renal replacement therapies are successful treatments for ESKD, prolonging survival, improving functional status and allowing patients to carry on with their lives, there is no doubt that Kidney Transplantation is the best of these options. It is the policy of the NRO that strategic planning should seek to maximize the numbers of patients who can avail of this. Whereas not all patients may be suitable as recipients of a kidney transplant, many more than have currently received one are so. This is reflected in the waiting list for kidney transplantation. As well as being a considerable physical, social and psychological burden on patients with ESKD treated by any of the forms of dialysis therapies, the costs to the State of providing these therapies are very substantial. In 2011, the ESRI noted (Activity in Acute Public Hospitals Annual Report 2010) that the highest ranked procedure for Day Patients in Public Hospitals was Haemodialysis, accounting for over one-fifth of all such cases. In 2012 almost 250,000 such procedures were delivered. Irish patients travelling to-and-from their Haemodialysis Units travelled over 13.5 million km in 2012. Despite reductions in the costs of such treatments in recent years, the sheer number of procedures continues to generate very substantial revenue charges. In the 5 years since 2007, the number of adults with ESKD has increased by 24%, an absolute increase of 743 patients. Of this increase, 63% has been accounted for by an increase in the numbers of those with a functioning Kidney Transplant (466), with the remaining increase due to an increase in those treated by Dialysis (277). There is, therefore, little doubt but that an increase in access to organs suitable for transplantation would improve the survival, rehabilitation and quality of life of many more patients with ESKD than at present. Furthermore, the potential future costs of Dialysis therapies foregone as a consequence of an increase in the transplantation rate would benefit the Renal Programme, the Health Service as a whole and the Irish taxpayer. The principal question that needs to be addressed is: how is this best achieved? A variety of potential solutions have been advanced by a variety of individuals, organizations and health care systems. I am happy to offer my own observations on those elements that I think are likely to increase transplantation, whilst preserving the confidence of the wider citizenry in the organization of this activity. Undoubtedly, increasing the resources available to support Living Donor transplantation is a key element. But what of Deceased Donor transplantation? As has been highlighted in a UK Health Technology Assessment (Health Technology Assessment 2009; 13:26), a number of elements contribute to the variation in rates of organ donation between countries. These include: 1. The national wealth and the investment made in Health Care Services. 2. The legislative framework that underpins donation (particularly as this applies to questions of ‘presumed’ or ‘informed’ consent). 3. The availability of potential donors 4. Public attitudes to, knowledge of, and education about organ donation and transplantation. 5. The organization and infrastructure provided to deliver organ donation and transplantation services. Much commentary has focused on Item 2 and it is of great importance. However, I would strongly associate myself with the views expressed by others that in the absence of a robust organization and infrastructure to support this endeavor, any legislative framework is unlikely to achieve its maximum potential in increasing donation. Similarly, robust engagement with the public to minimize anxiety, misunderstanding and fear regarding any potential legislative changes must also be of the highest importance. Thank you.