Atypical Haemolytic Uraemic Syndrome associated with a CD46
advertisement
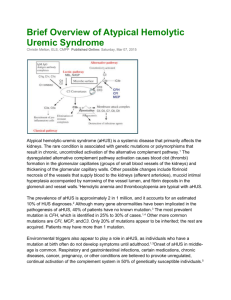
P2 ATYPICAL HAEMOLYTIC URAEMIC SYNDROME ASSOCIATED WITH A CD46 MUTATION UNMASKED BY A SHIGELLA DIARRHOEAL ILLNESS Vicky Brocklebank1, Edwin Wong2, Roy Ward3, Rick Fielding1, Tim Goodship1,2 , David Kavanagh1,2 1 Renal Services Centre, Freeman Hospital, Newcastle upon Tyne, 2The Institute of Genetic Medicine, Newcastle University, Newcastle upon Tyne, 3Department of Immunology, Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle upon Tyne BACKGROUND: Haemolytic uraemic syndrome (HUS) is characterised by the triad of microangiopathic haemolytic anaemia, thrombocytopenia, and acute kidney injury. The typical form is caused by infection with Shiga-toxin (Stx)-producing bacteria, most commonly Escherichia coli 0157:H7 and Shigella dysentariae. The atypical form (aHUS) results from complement dysregulation; a number of causative complement gene mutations have been identified. CLINICAL DESCRIPTION: A 38 year old British woman presented with diarrhoea to A&E in Holland and was found to have acute kidney injury (creatinine 663μmol/L), thrombocytopenia and microangiopathic haemolytic anaemia. Blood and stool cultures were positive for Shigella flexneri and antibiotics were administered. A diagnosis of Stx-associated HUS was made and she was treated with steroids and plasmapheresis. She did not require dialysis and her creatinine normalized. She returned to the UK and was referred to our renal clinic. S. flexneri does not usually produce Stx and Stx-PCR at the time of this patient’s presentation was negative. This led us to investigate for aHUS. GENETIC AND FUNCTIONAL ANALYSIS: Genetic analysis revealed a mutation in the complement regulatory protein CD46 (c.286+2T>G). Functional analysis demonstrated a nonsecreted protein. In individuals with mutations in complement genes, incomplete penetrance is seen and disease may not manifest until middle age, suggesting that a triggering stimulus (e.g. infection) is required. In this case, non-Stx diarrhoea unmasked the latent complement defect resulting in aHUS. DISCUSSION: This case raises important management issues as the patient is at risk of recurrent aHUS at times of infection. She has been advised to present for assessment immediately whenever she is unwell. Her relatives are also at risk and could be counselled. This patient would be a candidate for the complement inhibitor Eculizumab during a future recurrence. In conclusion, HUS presenting in the context of diarrhoea is not necessarily typical (Shigatoxin) HUS, because atypical HUS is not uncommonly triggered by a diarrhoeal illness in patients with complement gene mutations. We would recommend that investigating for aHUS is considered when there are unusual features in the case history, because it has important implications for management.