Infective Endocarditis Introduction Infectious clinical syndrome
advertisement
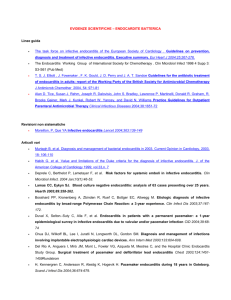
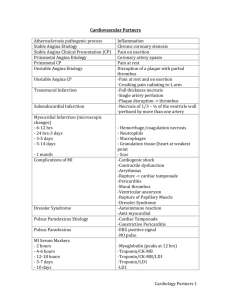
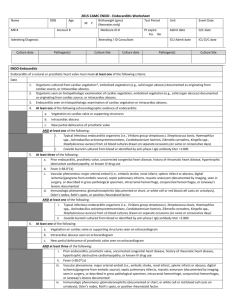
Infective Endocarditis Introduction Infectious clinical syndrome spans a continuum between acute and subacute presentations Acute endocarditis- febrile illness, rapid damage to cardiac structures and seeding of extracardiac sites hematogenously, death within weeks (6 wks). Subacute endocarditis-Follows an indolent course, rarely metastatic infection, slowly damages heart if occurs at all, gradual progression unless complicated by embolic event or ruptured mycotic aneurysm Brief Pathophysiology Infectious syndrome with a lot of causative pathogens. Consult Harrison’s for full list (Native Endocarditis, Prosthetic, IV drug user) Acute Endocarditis 1. Staph aureus 2. B-hemolytic streptococci 3. pneumococci Subacute endocarditis 1. Strep viridans 2. Enterococci 3. Coagulase negative Staph aureus 4. HACEK (Haemophilus, Actinobacillus, Cardiobacterium, Eikenella, Kingella) Endothelial injury [site of impact of high pressure jets or low-pressure side of a cardiac lesion] causes aberrant flow allowing: o Direct infection o Nonbacterial thrombotic endocarditis= Development of uninfected platelet-fibrin thrombus that is later infected during a transient bacteremia Vegetation-prototypic lesion = platelets + fibrin+ microcolony of organisms and scant inflammatory cells Differentials Signs and symptoms of IE are non-specific and highly variable. Why? o A predisposition to IE are valvular defectsvariable cardiac manifestations may be due to IE or the predisposing valvular defect example: murmurs may be due to a congenital VSD or rheumatic heart disease which predisposes the patient to IE or can be caused by IE. o Embolic events are a complication of IE. It can throw emboli anywhere in the body causing events such as stroke, MI, infarction of extremities, bowels, spleen, kidneys. o Metastatic infection-hematogenous spread may result in focal infections at other sites which include skin, brain, kidneys, spleen, skeletal system. It is possible to form abscesses and meningitis. The most common symptom is fever. So differentials will include ALL febrile illnesses. Since infective endocarditis can be caused by bacteremia of a host of pathogens and has variable symptoms and signs as stated earlier its diagnosis is not based on ruling out other diseases but of RULING IN infective endocarditis. (IE can exist with other diseases) Manifestations include: fever, chills and sweats, anorexia, weight loss, malaise, myalgias, arthralgias, back pain, murmurs, heart blocks, heart failure symptoms, arterial emboli, splenomegaly, clubbin, neurologic manifestations, peripheral manifestations, petechiae. Roth’s spots-oval retinal hemorrhages with pale centers Janeway lesions-small erythematous or hemorrhagic, macular nontender lesions on palms and soles due to septic embolic events Osler’s nodes-small tender, subcutaneous nodules in pulp of digits or proximally in fingers lasting for hours or days. Subungual hemorrhages Diagnosis When do we suspect IE? Suspect IE in all febrile patients with: 1. Valvular abnormalities, prosthetic valves 2. Congenital heart disease 3. IV drug abuser 4. Bacteremia with pathogens typical of IE 5. Unexplained arterial emboli 6. Progressive valvular incompetence (new or worsening murmur) Diagnosis is based on Duke’s criteria: DEFINITE endocarditis o 2 major criteria o 1 major + 3 minor criteria o 5 minor criteria POSSIBLE endocarditis o 1 major +1 minor criteria o 3 minor criteria DUKES criteria Major 1. Positive Blood culture a. Typical microorganism in 2 separate cultures b. Persistently positive blood culture i. Blood cultures drawn 12 hours apart ii. All 3 or majority of 4 or more separate blood cultures with 1st and last drawn at least 1 hour apart iii. Exception: Coxiella burnetii-single positive blood culture or elevated IgG antibody titer 2. Evidence of Endocardial involvement a. Positive echocardiogram i. Oscillating intracardiac mass on valve or supporting structures in the absence of an alternative anatomic explanation (vegetation) ii. Abscess iii. New partial dehiscence of prosthetic valve b. New valvular regurgitation Minor 1. Predisposition: heart condition or IV drug user 2. Fever >38.0oC 3. Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjuntival hemorrhage, Janeway lesions 4. Immunologic phenomena: glomerulonephritis, Osler’s nodes, Roth’s spots, Rheumatoid factor 5. Microbiologic evidence: Positive blood culture not meeting major criteria or serologic evidence of active infection with organism consistent with IE Mnemonic for Dukes criteria (original ito by Joguel) BE Vv’s FIMP (Read: Be VV’s PIMP!!!) Major criteria: BE= Blood culture + Endocardial involvement Minor Criteria Vv’s FIMP= Vascular + Fever + Immunologic + Microbiologic + Predisposition Plan Diagnostics Blood Culture, 2-D echo (for Duke’s criteria) o Note Transthoracic echo (TTE) is less sensitive than Transesophageal echo (TEE) CBC with PC with DC- elevated WBC with neutrophilic predominance, may have anemia Crea- kidney function test: involvement of kidney or Gentamicin nephrotoxicity (may be elevated) Chest radiograph- Heart enlargements (heart defects) ECG- detect heart blocks, MI, chamber enlargements Other labs: ESR, C-reactive protein, rheumatoid factor, circulating immune complex titers are all elevated IVF: No particular fluid needed. PNSS 1L x 12-24 hours to keep vein open (KVO). Choice of fluids may depend on other comorbidities Diet: Diet as tolerated Monitor: VS q1-4 hours with TEMP Admit to Ward or Micu-depending on the patient Treatment Ideally, treatment with antibiotics is culture guided. Consult Harrison’s for specific regimen for each pathogen. There are SEVERAL. But…. Empiric treatment (from Med Blue book): Acute Bacterial Endocarditis (including IV drug user)= main target Staph. aureus 1. Oxacillin 2g IV q4 or Vancomycin 500mg IV q6 or 1 gm q 12 (1 gm in 250 mL D5W infused slowly over 1 hour q 12) for 4 weeks 2. + Gentamicin 100-200 mg IV (2mg/kg), then 80 mg (1-1.5mg/kg) IV q8 for 3-5 days Note: may change regimen once with culture and sensitivity results. Subacute Bacterial Endocarditis= main target Strep viridans, Enterococci 1. Penicillin G 2-4 M units (12-24 M units/day) IV q4 for 4 weeks or Ampicillin 2 g (12g/day) q4 [high or low dose penicillin depends on microorganism and clinical course. High dose=toxic patients] If culture negative use Ceftriaxone 2 g IV OD for 4 weeks 2. + Gentamicin 80mg (1-1.5 mg/kg) IV q8 x 2 weeks Expected clinical course: Defervescence after 3-7 days Repeat blood C/S 2 and 4 weeks after end of treatment to detect relapse