EFFECTIVENESS, META-ANALYSIS AND QUALITY
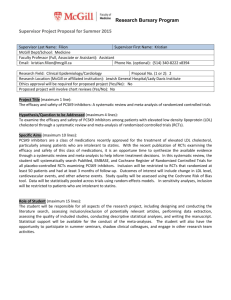
advertisement

Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS EFFECTIVENESS, META-ANALYSIS AND QUALITY-ADJUSTED LIFE YEARS Seminar work of Pharmacoeconomics Prepared by: Ognen Jakasanovski, Faculty of Pharmacy, University of Skopje Rosa López Pazos, Faculty of Pharmacy, University of Santiago de Compostela Luis Marin, Faculty of Pharmacy, University of Grenada Raquel Alonso Rubín, Faculty of Pharmacy, University of Santiago de Compostela Nicolas Jose Mallen, Faculty of Pharmacy, University of San Jorge Mariona Armengol Saborit, Faculty of Pharmacy, University of Barcelona Mentor: Prof. Mitja Kos, PhD Head of Department of Social Pharmacy Faculty of Pharmacy, University of Ljubljana Ljubljana, 25.05.2015 1 Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 2 Table of contents 1. Randomized clinical trials (RCTs).................................................................................. 4 1.1. What is a randomized clinical trial?......................................................................... 4 1.2. Classification of clinical trials ................................................................................. 4 1.3. Why might clinical trials not represent the true difference? .................................... 6 1.4. How randomized clinical trials are developed ......................................................... 8 1.5. Conclusion ............................................................................................................. 10 2. Clinical trial endpoints .................................................................................................. 11 3. Noninferiority trials ...................................................................................................... 14 3.1. Introduction ............................................................................................................ 14 3.2. When to choose to use a noninferiority trial? ........................................................ 14 3.3. How to choose the noninferiority margin, δ .......................................................... 15 3.4. Biocreep ................................................................................................................. 15 3.5. How to choose the correct sample size? ................................................................ 16 3.6 How to analyze noninferiority trials........................................................................17 4. Post-randomization data analysis of clinical trials.....................................................18 4.1. Approaches to analysis of clinical trials with regards to loss to follow-up patients ....................................................................................................................................................19 4.2. Per protocol analysis: post-randomization exclusions ........................................... 19 4.3. Intention-to-treat analysis: advantages and drawbacks of the pragmatic approach 21 Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 3 4.4. Design, implementation and reporting considerations for intention-to-treat analyses ..................................................................................................................................... 23 5. Systemic reviews .......................................................................................................... 25 6. Meta-analysis ................................................................................................................ 28 7. Interpreting meta-analysis graphs ................................................................................. 30 7.1. Meta-analysis graphs ............................................................................................. 30 8. Cost-utility analysis..................................................................................................... 32 8.1. Definition. Difference between cost-effectiveness and cost-utility analysis. ........ 32 8.2. Utilities................................................................................................................... 33 9. Quality-adjusted life-years (QALY) ............................................................................. 35 10. Health utilities ............................................................................................................. 38 10.1. Introduction .......................................................................................................... 38 10.2. Direct methods ..................................................................................................... 38 10.3. Indirect methods................................................................................................... 39 References ......................................................................................................................... 41 Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 4 1. Randomized clinical trials (RCTs) 1.1. What is a randomized clinical trial? Randomized clinical trials are scientific investigations that examine and evaluate the safety and efficacy of new drugs on human volunteers. Clinical trials can compare a new drug against existing drugs or placebo. The pharmaceutical companies are developing the new drug and sponsoring the clinical trials. Some studies using older drugs in new disease areas are funded by health related government agencies. In a randomized clinical trial, patients and trial personnel are accepting of which patient is on the new drug. This form can minimizes bias in the evaluation so that the initial blind random allocation of patients to one or other treatment group is conserved all the trial. Clinical trials must be designed in an ethical so that patients are not denied the benefit of usual treatments. Before at start the clinical trial the patients must give their voluntary consent that they will accept the purpose of the trial. The results that these studies generate are considered to be the most valued data in the era of evidence-based medicine. 1.2. Classification of clinical trials Depending on who is doing the Clinical trial, it will use one type or another kind of clinical trial. For example, Pharmaceutical companies conduct trials involving new drugs or established drugs in disease areas where their drug could gain a new license. For another hand, manufacturers use trials to prove the safety and efficacy of their new device. The clinical investigators unrelated to pharmaceutical companies might have other aims. For this reason, it's necessary different types of trials to cover these goals. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 5 Phases Classification based on the four clinical phases of development of a particular drug (Phases I–IV). In Phase I, manufacturers test the effects of a new drug in healthy volunteers. In Phase II, investigators examine dose–response curves in patients and what benefits might be seen in a small group of patients with a particular disease. In Phase III, a new drug is tested in a controlled fashion in a large patient population against a placebo or standard therapy. This is a key phase, because the drug can make or break its reputation with respect to safety and efficacy before marketing begins. Landmark study is a positive study for a drug; the drug can gain the license to be prescribed for a specific disease. In Phase IV, also called a post marketing study. The drug has already been granted regulatory approval/license. These studies are very important for gathering additional safety information from a larger group and appreciate drug interactions. Trial design This classification is more descriptive in terms of how patients are randomized to treatment. Parallel-group trial. Patients are randomized to the new treatment or to the standard treatment and followed-up to determine the effect of each treatment in parallel groups. Crossover trials randomized patients to different sequences of treatments, but all patients eventually get all treatments in varying order. Factorial trials can assign patients to more than one treatment-comparison group. Cluster randomized trials are used when larger groups are randomized instead of individual patients. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 6 Number of centres We can classify the clinical trials depend of the number of centres where are developing the trial: single-center or multicenter studies according to the number of sites involved. Single-center studies are mainly used for Phase I and II studies. Multicenter studies can be executed out at any stage of clinical development. This type are the most important because we can evaluate a new medication or procedure more efficiently in terms of accruing sufficient subjects over a shorter period of time. Other classifications Trials can also be described as superiority studies, equivalence studies, or noninferiority studies in terms of what the study was designed to prove. Superiority study aims to demonstrate that a new drug is more effective than the comparative treatment (placebo or current best treatment). Equivalence study is designed to show that two drugs have the same clinical benefit. No inferiority study aims to prove that the effect of a new treatment cannot be said to be significantly weaker than that of the current treatment. 1.3. Why might clinical trials not represent the true difference? In a clinical trial, the observed treatment effect not always represents the true difference between of the drugs comparison. Sometimes is possible that appearing erroneous outcomes with regarding the safety and efficacy of a new drug. There are three kinds of erroneous results. Bias/systematic errors. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 7 The design, conduct, analysis, and reporting of the results of a clinical trial, we can associate the occurrence of systematic errors for influenced by bias. The bias can also make the trial-derived estimate of a treatment effect deviate from its true value. There are most common types of bias in clinical trials: Related to subject selection, outcome measurement and estimate bias. Much of the advanced design strategies seek to reduce these systematic errors. Confounding Confounding represents the distortion of the real relationship between treatment and outcome by another factor. Confounding occurs when an extra factor is associated with the outcome of interest and treatment group assignment. For eliminate this type of bias, the solution is randomization in conjunction, evenly distributing both known and unknown confounding factors between treatment groups. Before start the trial we can delete the bias of confounding across randomization techniques: stratified randomization confounding and regression analysis. Random error The random error can have different causes. The sampling error is produced because the sample might yet show a chance false result compared to the overall population. This can be reduced by choosing a very large group of patients or by using special analytic techniques that combine the results of several smaller studies, called a meta-analysis. Statistical testing involves an evolution of the probability of obtaining the observed treatment difference, accepting that there isn't difference between treatments. This probability is called the P-value or false-positive rate. When the P-value is less than a specified critical value (5%), the observed difference is considered to be statistically significant. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 8 1.4. How a randomized clinical trial is developed To design and analyse a clinical trial, one needs to ask several questions. Like: What are the objectives and endpoints of the study? What patient population or disease is the drug meant to treat? What criteria should be used to select patients eligible for the study? How large should the sample size be so that the study will have enough power to detect a clinically significant benefit? How sure can we be about the observed treatment benefits and that they will reflect a genuine treatment difference with minimal influence of systematic errors, confounding, or chance? Objectives and endpoints A clinical trial should have clear objectives that are measured by endpoints. Study design It's important define which type of trial design we used on the clinical trial. It’s crucial to randomize patients to minimize systematic bias or confounding at the start of the study. It is necessary to split patients in groups at the design stage (two-arm, randomized, double-blinded, placebo-controlled). Patient population It should be noted that the results of a clinical trial could only be generalized to patients who are similar to the study participants. The goal is to evaluate a maximum number of patients. It's important define which kind of people need in the clinical trial. The study excludes patients who present with contraindications to treatment. All patients need to give their written informed consent before being enrolled. Sample size calculation Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 9 The sample size calculation is used for minimize random error. This process is called power calculation. The study needed sufficient ‘power’ to be able to say something definitive about the effect of the treatment so it was important to include a sufficient number of patients. For calculate the sample size for any given trial, it's needed statistical models that take account of the recruitment of patients into the trial and the type of statistical test to be used. Different formulas are used depending on the trial design – conventional parallel-arm trials, cluster randomized trials, factorial trials, and crossover trials – as well as on the type of endpoint chosen, such as continuous outcomes, binary outcomes, and time-to-event or survival outcomes. Conduct of the trial This step is important because the investigators recruit patients for the trial, with use of uniform procedures and management, and coordination via a single central unit. Also, they need to define the initial dose used of the study drug. The dose was increased or decreased in response to the patient’s clinical status, and algorithms are provided as guidelines for the management of hypotension or kidney dysfunction. After the titration, visits will scheduled every for X time. Interim monitoring For randomly assign patients is held at an independent statistical center and an independent data and safety monitoring board (DSMB) to establish the safety of patients enrolled in the trial and to monitor trial progress. The DSMB has to make sure that the new drug that patients are taking is not damaging. If, during the process of the trial, is found a risk then the trial has to stop. Monitoring trial results is ethically challenging and has to balance individual ethics with the long-term interest in obtaining sufficient data. Final data analysis All endpoints can analyse with the log-rank test, stratified and displayed on Kaplan–Meier plots. Also, it's possible use ratio from the Cox proportional hazards model useful to assess the size of treatment effect. Statistical analyses are usually stipulated in the trial protocol and should be performed as planned to ensure credibility and to deal with the issue of multiple testing. The principal statistical test for the primary endpoint analysis that is stipulated in the sample size Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 10 calculation should be applied. This means to plan a trial with care and to use current evidence that is as rigorous as possible in order to avoid as much bias as possible at the planning stage. Trial reporting The eventual results may publish different reports, which follow the CONSORT (Consolidated Standards of Reporting Trials) statement and guidelines of reporting. A trial profile was provided to describe the flow of participants through each stage of the randomized controlled trial: enrolment, randomization, treatment allocation, follow-up, and analysis of a clinical trial. The baseline characteristics of patients including demographic information, heart disease risk factors, medical history, and medical treatment, were displayed in an appropriate format for each component trial as well as the overall program. The results with respect to the prespecified primary endpoints and relevant secondary endpoints were provided in appropriate tables and figures. 1.5. Conclusion Randomized clinical trials are a major inversion in terms of patient and personnel involvement, and the funding needed to undertake the trial for the progress of medical care. An appropriate design requires a clear definition of the primary and secondary hypotheses in terms of measured outcomes and an explicit definition of the study population in order to avoid systematic errors. Statistical analyses deal with random errors due to sampling or random variation in the outcome variables. Interpretation of these statistical measures of treatment effect and comparisons should consider the potential contribution of bias or confounding. Finally, the clinical trial is conducted for ethical process and monitored in such a way as to minimize damage to patients, while observed to answer the initial questions posed by the trial of whether the new treatment is better, or similar to the comparison group. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 11 2. Clinical trial endpoints A clinical trial endpoint is a measure that allows researchers to decide whether the null hypothesis of a clinical trial should be accepted or rejected. The null hypothesis always establish that there is no statistically significant difference between two strategies that are compared respect to the endpoint measure chosen. Clinical trial endpoints can be classified as: Primary endpoints: measure outcomes that will answer the primary question in a trial. Usually, large trials have a primary endpoint based on multiple outcome measures, this are called composite endpoints. Secondary endpoints: ask other relevant questions. If secondary endpoints are as important as the primary, they are considered as co-primary endpoints. Types of endpoints: Binary clinical outcome indicating whether an event has occurred. Death from a disease specific cause. The occurrence of disease signs or symptoms. The relief of symptoms. Quality of life while disease is active. The use of healthcare resources. Time taken for an event to occur. Qualitative measurement of a biochemical or socioeconomic parameter. When choosing endpoints, they must: Be clinically meaningful and related to the disease process Answer the questions for a trial. Be assessed in all subjects in the same way. Occur frequently to have statistical power. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 12 If the endpoint consists of more than one outcome, they should be different, so they can be quantified independently. Death or time to death is one of the most important clinical endpoints. However, it has some limitations: it can occur out of the timeframe of the trial; is very expensive to follow-up all the patients of a study until they die; and finally, they can die for other reasons than the disease. Composite endpoints are endpoints make up of multiple outcomes. Is better to organize them in total number of outcomes per patient and in hierarchical counts. In this case, only one outcome is counted for each patient, and usually the most serious outcome is recorded. Other way to record multiple outcomes is compare the number of recurrences of identical outcomes during a followup period. Advantages: Less patients are needed because more events will occur and be observed in total. Better understanding of a treatment can be given across more than one category of outcome. Limitations: Avoiding any other outcome has an equal importance as avoiding any other outcome. All individual outcome measures are related to the disease process and are equally meaningful. Inconsistent results which relative importance should be determined prior to data collection, during the design of the trial. Surrogate endpoints is a laboratory measurement of physical sign used as a substitute for a clinically meaningful endpoint that measures directly how a patient fells, functions, or survives. Surrogate endpoints can be: pharmacokinetic measurements, in vitro measurements, radiological appearance, change in the levels of disease markers, and macroscopic appearance of tissues. They are very useful in Phase II screening trials to identify whether a new intervention has an effect. If there is sufficient change, a large trial might be justifiable. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 13 Advantages: Less sample needed, therefore also duration and costs. Limitations: Only useful if they are good predictor of a clinical outcome. If this relationship is not clearly defined, surrogate endpoints can be misleading. Health economic endpoints are measured using quality-adjusted life-years (QALYs) gained and cost. They can be combined to obtain cost-effectiveness ratio, which indicates the cost of gaining an extra year of life or a benefit in the quality of life for the patient. Besides, it is measured also the willing to pay to avoid one event by patients. Nowadays, assessment of health economics is very important in new treatments and in the approval and reimbursement of new therapies. Advantages: They can be easily compared directly to know where the best to invest the limited resources of healthcare systems. Calculate the cost of all events experienced by each patient, not just the first or the worst one. Limitations: Data might not be even used if the treatment is more expensive and less effective than standard care. Less robust data because many assumptions must be made. This studies are not easily comparable among countries because the cost of care can be very different and clinical results depend on local practice patterns and the availability of facilities. Certain disease states affect the patient only briefly and might not have a long-term impact if they are not fatal. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 14 3. Noninferiority trials 3.1. Introduction A noninferiority trial tries to demonstrate that a new treatment is not worse than the treatment currently in use (the comparator). the margin in which the new treatment can differ is specified by the δ value. It is critically important to choose the correct value of δ, as well as the methods to choose the correct the sample size or considering the issues involving the analysis and evaluation of noninferiority. δ is a value that determines the maximum difference in efficacy between the new treatment and the comparator, meaning that a higher difference would be clinically unacceptable. the trial must be designed to conclusively show that the new treatment’s effect is worse by no more than an agreed, prespecified amount. Noninferiority trials are included in the category of equivalence trial. Noninferiority trials can be used in other therapeutic areas, and not just on comparing active ingredients. For example, it could be used to compare new pharmaceutic forms, new ways to administrate the medicament, new surgeries etc. 3.2. When to choose to use a noninferiority trial? Noninferiority trials are mainly used when an actual effective treatment is already being used. In those cases, carrying a randomized, placebo-controlled clinical trial might be unethical (as it would lead to leaving patients without a treatment intentionally and knowing they could be otherwise treated with the classical treatment). Noninferiority trials are used to discover secondary advantages of a new treatment (safety, convenience, cost-effectiveness), or to discover if it has potential as a second-line therapy in those cases where the standard treatment fails. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 15 Noninferiority trials are not randomized, double-blinded, nor placebo controlled, meaning they do not follow the "gold standard" of a clinical trial. But in some cases it is possible to incorporate a third placebo controlled arm to the trial in order to demonstrate the internal validity within the trial. Also, noninferiority trials have troubles when considering the effectiveness of the treatment, because of poor investigator conduct or patient compliance. 3.3. How to choose the noninferiority margin, δ The value is typically chosen using clinical judgment, with reference to relevant regulatory guidance and, if appropriate, to guidance for the particular indication. When deciding the value of δ, it should be decided so that a value exceeding δ would be unacceptable for a new treatment, and a value not exceeding would be considered clinically irrelevant, so that there would be no relevant differences between the old and new treatments. An alternative way to arrive at a δ is to think of the study as attempting to show that the new compound is superior to a historical control. A δ of half the difference previously demonstrated in a superiority trial might, therefore, seem appropriate. Other factors that might influence the choice of δ are the degree of risk associated with treatment failure for the indication, relative toxicity, ease of use of the new treatment compared with the control, and, possibly, feasibility of the study in terms of enrolling the required number of subjects. 3.4. Biocreep Biocreep is a problem that appears in noninferiority trials. It refers to a phenomenon where a new treatment is accepted by using a noninferiority trial, an that new treatment becomes the comparator for another new treatment. the accumulation of irrelevant values lower than δ finally becomes an actual relevant difference in the effectiveness. The concern can be alleviated when the chosen active comparator is the current gold standard treatment, and δ is chosen appropriately for the indication in question and further reduced if a placebo arm is incorporated into the study design. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 16 3.5. How to choose the correct sample size? The sample size should had a volume that enables the trial to have a confidence interval good enough to prove that the new treatment's efficacy is worse by, at most, δ. The following statistics are required to determine the sample size: 1. Anticipated efficacy of the comparator (ie, proportion for a binary endpoint, and mean and standard deviation for a continuous endpoint) 2. Significance level or threshold (α, Type I error) 3. Power (1 – β, 1 – Type II error) The final sample size will vary depending on the anticipated efficacy of the comparator, the anticipated effect of the new treatment, and the δ that has been decided to use. Noninferiority trials require larger sample sizes than a placebo-controlled superiority trial, although smaller sizes than an active-controlled superiority trial. In noninferiority trials, the null hypothesis is that the difference between treatments is bigger than δ, and the alternative hypothesis is that the difference is not bigger than δ. According to the guidelines a one-sided CI is used to assess noninferiority. In the alternative antiinfectives therapeutic area, a noninferiority trial based on a one-sided 95% CI is used. It has to be taken into account which methodology will be used to calculate the CI for assessing the noninferiority: specially, using conservative analysis methods should be avoided (Such as the binomial approximation to the binomial distribution. 3.6 How to analyze noninferiority trials. In noninferiority trials, we calculate a CI in order to estimate the range of values in which the treatment difference is likely to be. If the calculated CI values are inside the tolerated margin ( δ), Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 17 then the noninferiority is demonstrated. The confidence level of the confidence interval (CI) is generally set ar 95%, corresponding to the 3.5% one sided significance level. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 18 4. Post-randomization data analysis of clinical trials 4.1. Approaches to analysis of clinical trials with regards to loss to follow-up patients The appropriate analysis and presentation of results are of utmost importance for all clinical trials. Often, however, the practical implementation of the trial can create problems in the further analysis. Therefore, in order to reduce bias during the analysis phase of the clinical trial, the study design must be planned in a way, in which it precisely defines the types of analyses conducted in the later phases of the trial. One common problem of data analysis of clinical trials is that of the loss to follow-up – when patients who participate in a particular randomized controlled trial, fail to adhere to the study protocol, for various different reasons. Sometimes, patients lose motivation to comply with the given therapy (both active therapy and placebo), other times clinicians may recommend withdrawal of the study medication because of the presence of adverse reactions in certain patients. Furthermore, sometimes patients die throughout the course of the trial and thereby do not make it until the end. Generally, two different approaches of clinical trial data analysis are used: per-protocol (PP) analysis and intention-to-treat (ITT) analysis. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 19 Figure 1: A simplified scheme for randomized controlled trials. The first step, patient selection comprises inclusion and exclusion criteria including patient consent. That done, randomization treatment A or treatment B should take place ‘as late as possible’, when diagnostic and consent procedures have all been completed. By the end of the trial there are four groups of patients, as shown above. Intention-to-treat analysis compares 1+2 with 3+4. Per protocol analysis compares 2 with 3, ignoring 1 and 4. 4.2. Per protocol analysis: post-randomization exclusions The per-protocol analysis excludes subjects who were not fully compliant with study protocol. It is also called efficacy, explanatory analysis, or analysis by treatment administered. By focusing only on the fully compliant subjects, one can determine the maximal efficacy of a treatment using the PP analysis. Although the researcher can use the information gained from this type of analysis to estimate the efficacy of a therapy to those who have received it in the intended intensity or dose and in the intended time interval, this estimate is very likely to be flawed. The problem of per protocol analysis arises because the reasons for non-adherence to the protocol may be related to the prognosis. Evidence has suggested that patients who adhere to therapy tend to have a better outcome than those who do not adhere, even after the adjustment for all known prognostic factors and irrespective of the assignment to active treatment or placebo. Therefore, excluding non-adherent participants from the analysis leaves those who may be destined to have a better outcome and presents a problem for the desired unbiased comparison done by randomization. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 20 Another important pitfall of the per protocol analysis is that it does not give general, pragmatic results of the studied treatment, but rather a conservative and more specific conclusion that would potentially not be able to mirror the real-life experience of the treatment and its efficacy. One example of creating bias by excluding patients are the examples of excluding patients who do not meet the eligibility criteria of the trial, but were randomized before their eligibility could be confirmed. Excluding such patients can have detrimental implications to the quality of the trial results. For example, one study of an anti-influenza drug randomized 629 patients, of whom 255 (40%) were found not to have influenza throughout the course of the trial.1 The study reported that, in the 374 patients who were infected, the study drug (oseltamivir) reduced the duration of illness by 30% (P < 0.001). However, when all 629 randomized patients have been analyzed (intention-to-treat analysis), the impact of the drug was, as we would expect, much lower, with a reduced duration of 22% (P = 0.004). The approach used in the example study described above, can on the one hand be seen as pure common sense, because there is no need of analyzing the impact of a drug to a population that does not have a potential of benefiting from the treatment. Hence the reason why per protocol analysis is called efficacy or explanatory analysis. However, retrospective exclusion of a large number of patients who would not be expected to benefit from the treatment creates a potentially misleading impression of the overall effect of the treatment on the population for which it would be used. For example, oseltamivir was found to cause nausea or vomiting in 19% of all randomized patients, which also includes the ones who have not been infected with the influenza virus. This clinical scenario mirrors clinical situations that happen in the common clinical practice, where doctors need to treat patients before all information is available. The cases where per protocol types of data analysis are not sufficient and do not provide a sufficient pragmatic view of the effectiveness of a treatment are not only limited to cases like the 1 Treanor JJ, Hayen FG, Crooman PS, Barbarash R, Betis R, Riff D, et al. Efficacy and safety of the oral neuraminidase inhibitor oseltamivir in treating acute influenza. A randomized controlled trial JAMA 2000;283:1016-24 Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 21 one explained above. On the contrary, in many cases of clinical trials, excluding patients from the analysis post-randomization presents a problem for the validity and objectiveness of the results. Other cases include the ones of testing medicines with narrow therapeutic range, as well as chemotherapeutics (e.g. some anti-cancer agents), where the adverse effects caused by the treatment applied in the trial have an influence on the compliance with therapy. Another example is those of drop-outs from the clinical trial because of logistical difficulties of the healthcare systems. When surgical treatment is compared to a medicinal treatment for a particular disease, surgeries usually take longer time, and patients can be scheduled to surgery for a few days, months, or even years. On the other hand, medicinal treatment can usually begin immediately. Patients sometimes die before making it to surgery, and therefore are considered as non-treated. In this case, a pragmatic, intention-to-treat analysis is required, in order to objectively depict the real-life scenarios of burdened healthcare and waiting for surgery, which influence the actual prognosis of the patients. Essentially, the major issue in interpretation of results becomes the one of effectiveness versus efficacy or explanatory versus pragmatic approaches. The clinical studies need to ensure that the benefit of the therapy studied to patients with the underlying condition outweighs the harm to patients exposed to the therapy, without possibility of benefit. Therefore, the scientific community almost unanimously points out that the primary presentation of the results should include the patients randomized into the study (intention-to-treat analysis), whereas a secondary analysis of efficacy can also be conducted, especially in the cases where it is uncertain whether the treatment is actually effective. 4.3. Intention-to-treat analysis: advantages and drawbacks of the pragmatic approach An intention-to-treat (ITT) analysis is a specific clinical trial design and conduct strategy for generating the results of an RCT. It is an approach of comparing all trial subjects according to the treatment groups in they were initially randomized, regardless of treatment compliance, or any treatment subsequently received. The rationale for using the ITT method is that, even though not all patients will fully adhere to the therapy, the non-compliant subjects would probably be equally arranged between the different treatment groups. ITT analysis is also known as effectiveness or pragmatic analysis. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 22 Initially, it appears that the ITT strategy makes less sense than the PP method, but as we have seen, the PP analysis can often lead to potential bias and inference, and thereby give an incomplete depiction of the potential benefit of a certain therapy. As the purpose of randomization is to avoid selection bias and to generate groups which are comparable to each other, any changes to these groups by removing particular individuals’ records or transferring them to another group destroys that comparability. Hence, intention-to-treat types of analysis are the current golden standard for clinical trial data analysis, preferred over PP analyses, which can only be disregarded and inapplicable in rare circumstances in healthcare research. The specific advantages seen in the ITT analysis are: Preserving the strengths of randomization and minimizing bias. An ITT analysis presumes that the rate of non-adherent patients will be equal in all treatment groups, as they were randomly allocated in the first place. An ITT analysis depicts real-life situations better than the PP analysis does. It is therefore a more suitable option for analysis of treatments with lots of adverse effects (e.g. chemotherapeutics), where patient compliance is dependent from the effect of the medicine tested. An ITT analysis uses the information from all subjects at any given point in time, which enables for interim analysis to be performed, whereas the PP method is more suitable after the end of the study, where all non-compliant patients can be identified and excluded. ITT analysis provides practical information on the administration of the surgical treatment. As it has been previously explained, many logistical reasons can lead to non-treatment or non-adherence, so an ITT analysis would give a more objective view on the effectiveness of the therapy. There are also, however, some disadvantages and limitations of using ITT analysis. This type of analysis does not determine the maximum potential efficiency of a treatment as a PP method would. Therefore, in some studies, the ITT method might not show a statistically significant benefit, or might show the benefit to be smaller than that generated by a PP analysis. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 23 When using the ITT method, the definition of a dropout patient should be agreed upon during the design phase of the study. In the worst-case scenario, it could be assumed that all subjects who withdraw count as deaths or as ‘no events’, but in reality these subjects will suffer a mixture of events. In some studies it may be assumed that the event rate in the missing subjects is the same as in the group of subjects with data available (known as imputing event rates). This method should only be used if it proves impossible to get outcome data from a large proportion of subjects, and the results should be presented with and without imputation. 4.4. Design, implementation and reporting considerations for intention-to-treat analyses The ITT strategy is commonly regarded as not only a method of analysis, but also a manner of conducting an entire research study, including trial design. When designing a trial, it should be specified whether the study is pragmatic (aiming to determine the practical impact of the treatment strategy) or explanatory (using a trial to determine the efficiency of a treatment strategy). For pragmatic trial, the ITT method is used, whereas for explanatory trials a combination of ITT and PP provides insights. The distinction between these two methods makes practical significance only in the cases where a large number of the patients were non-compliant with therapy, withdrew, or have provided insufficient data. Recommendations for intention-to-treat analysis Design Decide whether the aim is pragmatic or explanatory. For pragmatic trials, intention to treat is essential. Justify in advance any inclusion criteria which when violated would merit exclusion from intention to treat analysis. Conduct Minimise missing response on the primary outcome. Follow up subjects who withdraw from treatment. Analysis Include all randomized subjects in the groups to which they were allocated Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 24 Investigate the potential effect of missing response Reporting Specify that ITT analysis has been carried out, explicitly describing the handling of deviations from randomized allocation and missing response. Report deviations from randomized allocation and missing response. Discuss the potential effect of missing response. Base conclusions on the results of ITT analysis. Figure 2: Considerations for intention to treat strategy Almost half of the reports of randomized controlled trials have included an analysis described as intention-to-treat in a study by (Holis, 1999). Intention to treat analysis can be often vaguely described and not explicitly presented in the reporting phase as such. Therefore, future researchers should take in consideration all recommendations listed in Table 2, and future readers of papers with ITT analyses should also critically appraise the information provided. Full reporting of any deviations from random allocation and missing response is essential in the assessment of the necessity and appropriateness of an intention-to-treat approach, as emphasized in the CONSORT guidelines on the reporting of randomized controlled trials. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 25 5. Systemic reviews The purpose of a systematic review (literature review) is to sum up the best available research studies on a specific question. This is done by identifying, selecting and synthesizing the results of several studies relevant to that question. Nowadays an understanding of systematic reviews and how to implement them in practice is becoming mandatory for all healthcare professionals. Systematic reviews are not limited to medicine and are quite common in all other sciences where data are collected, they may concern these areas: Clinical tests Economic evaluations Medicine and healthcare Public health interventions Social interventions In the latter half of the 20th century has been an explosion in medical and healthcare professional publishing, which makes keeping up with primary research evidence an impossible feat. There has also been an explosion in Internet access to articles that allow access to large amounts of information. Some of these studies may give unclear, confusing or contradictory results; sometimes they may not be published in our own language. Therefore there could be lack of clarity and lead to a false belief. Reviews have always been a part of the healthcare literature. Traditional reviews (literature reviews) differ from a systematic review: Traditional review They are not led by peer-reviewed protocol and it is no possible to replicate the findings They are not explicit about how studies are selected, assessed and integrated Lack of rigor Different conclusions Systematic review They are led by peer-reviewed protocol and it is possible to replicate the findings They are explicit about how studies are selected, assessed and integrated High quality of rigor Common conclusion between reviewers Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 26 Table 1: Differences between traditional review and systematic review Systematic reviews are needed to establish clinical cost-effectiveness of an intervention or a drug. They are also needed in these situations: 1. Needed to propose a future research plan 2. Required by authors who want to research in primary healthcare 3. Required by postgraduate theses 4. Needed whenever there is a question with different findings A good systematic review requires these following steps: 1. Defining an appropriate healthcare question. This requires a definition of the objectives of the review, phenomena of interest, relevant patients groups… Details that must be rigorously used to select studies for inclusion in the review. 2. Searching the literature. Reviewers should search for published and unpublished literature for the required studies. The grey literature is material that is not formally published, such as conference proceedings, working papers, technical reports, etc. 3. Assessing the studies. After the studies have been identified, they have to be assessed. This assessment should be conducted by two independent reviewers. 4. Combining the results. Reviewers have to exchange their findings and then be aggregated. If a systematic review inspects quantitative data, then they get a meta-analysis. 5. Placing the findings in context. The findings need to be discussed to put them into context. High quality systematic reviews are published in many journals and electronic databases. Some useful websites for systematic reviews could be: The Cochrane Library The Joanna Briggs Institute Pubmed The Campbell Collaboration Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 27 Whether the reviews are well conducted, they should give us the best possible estimate of any true effect. A number of problems may arise within reviews of clinical effectiveness: A. A systematic review may be done badly B. Inappropriate aggregation of studies. Differ in terms of intervention used, patients included, types of data… Contradictory findings should be balanced in order to assure that systematic revision criteria are respected. A systematic review uses transparent procedures to find, evaluate and synthesize the results of relevant research. Procedures are explicitly defined in advance, in order to ensure that the exercise is transparent and can be replicated. This practice is also designed to minimize bias. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 28 6. Meta-analysis Meta-analysis can be defined as a statistical research technique which Metaanalysis combines the findings from previous research. It is a method for systematically combining qualitative and quantitative data from selected independent studies to develop a single conclusion; by combining data from two or more randomized trials. Systematic review They are most often used to assess the clinical effectiveness of healthcare intervention; Does the new treatment confer significant benefits compared with the conventional treatment? In medicine is Randomized trials common to find trials that tried to answer similar questions about clinical effectiveness. Many of the individual trials fail to show a statistical difference between the two treatments. Nowadays meta- analysis studies include these quantitative differences. They are based on systematic review methodology: impartial summary of the existing research. If the systematic review provide a quantitative estimation of benefit is termed a meta-analysis. Therefore, the main requirement for a good meta-analysis is a well-executed systematic review. A meta-analysis research offers a series of advantages: o Overcoming bias. The danger of a narrative reviews is that they could introduce bias. If a meta-analysis is carried out on a rigorous way, it can overcome these dangers. o Precision. These researches have more power to detect clinical significant effects. o Transparency. A good meta-analysis should allow readers to determine for themselves the reasonableness of the decisions taken. There are some steps that reviewers must follow to provide a good and rigorous meta-analysis research: Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 29 1. Location of studies. Meta-analysis requires a search strategy which includes: electronic databases, hand-searching, use of key terms… Then the reviewers include papers with specified terms and exclude papers that do not meet certain criteria. 2. Quality assessment. Once studies have been identified, it has to be defined an explicit and objective criteria for inclusion or rejection. 3. Calculating effect sizes. Results are usually summarized as a ratio of the frequency of the events in the intervention group to that in the control group. The risk ratio (relative risk) is the most common measure. For example, a ratio of 5 implies that the outcome happens about five times as often in the intervention group as in the control group. 4. Checking for publication bias. The most common way of assessing the likely presence of publication bias is to examine a funnel plot. 5. Sensitivity analysis. A good sensitivity analysis excludes various categories of studies. For example, unpublished studies or those of poor quality. Some questions will help to assess the quality of the systematic review and meta-analysis: Was publication bias assessed? Was heterogeneity considered and tested for? Was the quality of the individual studies assessed using an appropriate checklist of criteria? Was combined effect size calculated using appropriate statistical methods? Meta-analysis are an useful tool to resolve therapeutic uncertainty. They offer a systematic and quantitative way of summarizing information. Nevertheless error in their planning can lead clinicians to mislead decisions. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 30 7. Interpreting meta-analysis graphs 7.1. Meta-analysis graphs Meta-analysis is a set of statistical tools that are useful to synthesize data from a collection of studies. The meta-analysis begins by collecting a certain effect estimates (expressed as an index of effect size, as typified mean difference, risk ratio, or correlation) of each study. Meta- analysis can assess these effects in context: if the effect size is consistent, the effect of treatment can be considered as strong and the effect size is estimated more accurately than a single study. If the size of the effect varies, this variation can be described and potentially explained. Displayed above the graph: -Review: Title/research question of the meta-analysis -Comparison: Intervention VS control group -Outcome: Primary outcome measured and presented in the graph. Types: ·Meta-analysis of binary outcome measure. ·Meta-analysis of continuous outcome measure. 7.2. Graph´s components and structure: Meta-analysis graphs can be divided into six columns. ·The first column, “study”, list the individuals study ·The second column relates the the intervention group and the third column to the control group; -Binary outcomes: n/N (n=numbers of participants with the outcome; N=total number of participants in the intervention or control group) -Continuous outcome: In this case “N” mean “SD”(standard deviation) in both studies ,such as Binary and Continuous measures Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 31 ·The fourth column is formed by a line in the middle is called “the line of no effect”; Binary outcome (Odds ratio “OR” or Relative risk “RR”) is around 1, and in continuous outcome (WMD) is around 0. There are some boxes on the line, the size of the box is directly related to the “weighting” of the study in the meta-analysis. The horizontal lines (whiskers) describe the length of the confident interval “CI”. ·The fifth column is related to the weight, is in percentage (%). Indicate influence of the study on the overall results of the meta-analysis. The real measure of how weight or important is the study ,is related with the results provided as a CI. ·The sixth column gives the numerical results for each study( OR,RR or WMD). There is a diamond on the last row that values the overall effect estimate; and width is the effect as width is the “CI”. Is important to check at the bottom of the graph, some graphs display to the left side of the “line of no effect”. Also one needs to be aware if the meta-analysis deals with binary or continuous variables; In Binary always greater than 0 , and in continuous variables values can be negative and positive. 7.3. Results The heterogeneity test: In the bottom of the graph is a parameter P, ranges between 0% and 100% and measure the variability between studies, i.e how comparable studies in meta-analysis are. According with the values of P; if P is smaller than 25% the study is regarded homogeneous and if P is bigger than 75% , the heterogeneity is very high. Fixed and random effect models: When the research question in the meta-analysis is whether treatment has produced an effect in the set of homogeneous studies analyzed, the fixed model is he appropriate one. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 32 8. Cost-utility analysis 8.1. Definition. Difference between cost-effectiveness and cost-utility analysis. Cost-utility analysis (CUA) is a form of evaluation that focuses particular attention on the quality of the health outcome produced or forgone by health programmes or treatments. It has many similarities to cost-effectiveness analysis (CEA), because they have similar underlying principles of conducting. In the CEA analysis, the incremental cost of a programme from a particular viewpoint is compared to the incremental health effects of the programme, with the health effects being natural units related to the objective of the programme (blood pressure improvement in mm Hg, cases found, cases of disease averted, seizures prevented, blood HDL reduced etc.). The results are usually expressed as cost per unit of effect. On the other hand, CUA compares the incremental cost of a programme from a particular viewpoint (same as CEA) with the incremental health improvement attributable to the programme, where the health improvement is measured in quality-adjusted life-years (QALYs) gained, or possibly an alternative, like disability-adjusted life-years (DALYs) gained. The results are expressed as cost per QALYs gained. The main similarity between CEA and CUA is the cost data, which is in most cases similar, or the same. The difference between these two methods of analysis are the outcome (effectiveness) data. In both cases, it is gained either from the literature, from the researchers study, or from experts, however, in the CUA analysis only final outcome effectiveness data will suffice (for example, lives saved, disability-days saved). Intermediate output data (e.g. cases found, patients properly treated…) are not suitable, because they cannot be directly converted in an outcome measure such as QALYs gained which is required for CUA. Below we list the most commonly presented advantages of incorporating a CUA: CUA is a more suitable type of analysis when the health-related quality of life is important outcome (e.g. arthritis, where no program is expected to influence mortality, but rather improve the patient’s physical function, social function, and psychological well-being). Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 33 It is also a more suitable type of analysis when the health-related quality of life is an important outcome (e.g. evaluating neonatal intensive care for very-low-birth-weight infants, where not only is survival an important outcome, but also the quality of the survival). It can be used in cases when the programme (treatment or medicine) tested affect both mortality and morbidity, and there is a need for a common unit of outcome combining both effects (e.g. cancer chemotherapy, which may improve longevity and long-term quality of life, but decreases quality of life during the treatment). It enables comparability and transferability of results, as opposed to CEA, and enables for the programme tested to be compared with other programmes. This is useful when the healthcare systems with limited budgets make decisions about which programme to reduce, eliminate or remove funding from, when a new treatment programme is adopted. This goes in line with the priority of health-care systems to maximize the overall health gain achieved. 8.2. Utilities The effectiveness of a particular medical programme studied can be expressed in prolongation of life (e.g. average number of life-years saved). However, some treatments may prevent worsening of the quality of life without actually extending it. Others, on the contrary may extend life but with the presence of significant disability that reduces its quality. In pharmacoeconomics, those situations are dealt with by placing a value on the quality of life, i.e. its utility. The terms utility, value and preference are often confused between one another, but in fact, they carry different meanings. Preference is the umbrella term which describes the overall concept; utilities and values resemble different types of preferences. As shown in Table 2, there are two types of measurement options. One is the way in which the question is framed, specifically whether the outcomes are certain or uncertain. The other way in which the subject is asked to respond, specifically whether the subject is asked to perform a scaling task based on the introspection or to make a choice. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS Response method Scaling 34 Queston framing Certainty (values) Uncertainty (utilities) 1 – rating scale, category 2 scaling, visual analogue scale, ratio scale Choice 3 – time trade off, paired 4 – standard gamble comparison, equivalence, person trade-off Table 2: Methods of measuring preferences Table 2 is divided into four cells. Cell 1 contains instruments that require the subject to think introspectively about outcomes presented with certainty and to provide a rating or a score. Rating scales (assign a number), category scales (assign a category) and VASs (mark a line) are all variations of the same theme. Ratio scaling, also belongs in this category. In ratio scaling, subjects were asked to indicate how many times worse is an outcome compared to the next best one. The outcomes were defined with certainty and the task was one of introspection. There are no instruments that fall in cell 2, although presumably one could ask subjects to rate their preferences for gamble alternatives. Cell 3 contains the time-trade-off (TTO) approach, the paired comparison approach, and the old equivalence approach, now renamed the person trade-off (PTO) approach. Finally, cell 4 contains the well-known standard gamble in all its variations. Health utilities are further described in Chapter 10: Health Utilities. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 35 9. Quality-adjusted life-years (QALY) The QALY is defined by the National Institute for Health and Clinical Excellence (NICE) as measure of a person’s length of life weighted by a valuation of their health-related quality of life. A quality-adjusted-life-year (QALY) takes into account both the quantity and quality of life generated by healthcare interventions. The QALY is expressed by this equation: QALY= UxT being the T the life years gained and the U the quality of that years. On one hand, the quantity of life is a type of measure to assess if people are alive or not. On the other hand, quality of life is focused on the person´s health status. Quality could be valued between 0 and 1. In this scale, the zero value is the death stage and one is the perfect health. In the middle of this scale, there are different statuses of health. Mobility Pain/discomfort Self-care No problems No pain or No problems Not anxious or walking about. discomfort. with self-care. depressed. Some problems walking about. Some Moderate pain problems or discomfort. washing or dressing. Confined to Extreme pain or bed. discomfort Unable to wash or dress self. Anxiety/depression Usual activities No problems in performing usual activities. Moderately Some problems anxious or in performing depressed. usual activities. Extremely anxious or depressed. Unable to perform usual activities Table 3 One example of different questions to assess health condition is the EQ-5D test. It is formed by five dimensions and has three levels: no problem, some problems and major problems. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 36 The patient is the responsible of giving a score in this test between 0 and 1. One year of perfect health will take a score of 1 and it generates one QALY, whereas one year in a health state valued at 0.5 is regarded as being equivalent to half a QALY. Thus, an intervention that generates four additional years in a health state valued at 0.75 will generate one more QALY than an intervention that generates four additional years in a health state valued at 0.5. For example, if we apply the previous equation we will get this result: Intervention Years gained Quality score QALY A 4 0,75 4x0,75= 3 B 4 0,5 4x0,5=2 So the intervention A is the best alternative, because it gets a higher value of QALYs. QALYs provide a common currency to assess the extent of the benefits gained from a variety of interventions in terms of health- related quality of life and survival for the patient. They are used to assess the effectiveness of interventions and are combined with the costs incurred in providing the interventions to generate cost-utility ratios in a cost-utility analysis. A cost-utility analysis is performed in the same way as a cost-effectiveness analysis except that the unit of effectiveness is quality-adjusted-life-years (QALYS). A cost-utility ratio is the difference between the costs of two interventions divided by the difference in the QALYs they produce. Figure 3: An example of a cost-utility ratio However the QALY have some disadvantages as a measure method of quality of life: 1. It is hard to understand the results by uneducated people and is needed the intervention of an expert. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 37 2. The development of the test is not clear and in some cases is needed a previous explanation before doing the test. 3. Sometimes the outcomes are not reliable. 4. The test is designed only for chronic diseases, what happens in acute diseases? 5. The test is not equal for all population QALYs and cost–utility analysis provide additional information for decision-makers as they grapple with addressing the healthcare dilemma of where to allocate resources to generate the maximum health benefits for their communities and society as a whole. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 38 10. Health utilities 10.1. Introduction Health utilities are cardinal values that reflect an individual's preferences for different health outcomes. They are measured on an intervale scale where: Zero means death One is perfect health This data is used to generate quality-adjusted life-years (QALYs) for use in cost-utility analysis. For measuring health utilities, two components must be considered: Set of health states of interest Measurement of the strength of preference of each one. We can use direct or indirect methods to measure health utilities. 10.2. Direct methods First we should assess relevant dimensions and levels of health that we are considering. If they do not correspond to patient outcomes, it will not be possible to detect differences. Because of this reason, they should be based on direct patient experience. They know first-hand the impact of the disease and treatment. Besides, they can be asked to value a hypothetical health state or their own health state. It has some limitations: - Difficulty of recruiting enough number of patients with the specific health states of interest. - Hypothetical scenarios might not be valid predictors, because in this case, patient values tend to be higher Minimum sample size is another question. In general, a minimum of 100 respondents is considered reliable, and the number of health states should be at maximum ten but fewer if it is possible Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 39 On the other hand, some studies use also opinions of professionals that are backed by literature evidence. However, their value is being recognized as a not valid source. Direct methods are: Standard gamble (SG). Measures preferences in economics under conditions of uncertainty. It presents to the individuals a choice between two alternatives: - A health state that is certain - Gamble with a better and a worse possible outcome Requested people should ask what probability of the better outcome would make them indifferent between remaining in the described health state for certain or going for the risky option. This utilities depend on the risk behavior or the survey respondents, that is, in general, averse to the risk, so the meaning will tend towards the certain outcome rather than the gamble. Time trade-off (TTO). Is based in asking subjects to consider the relative amounts of time they would be willing to sacrifice to avoid a certain poorer health state. It assumes risk neutrality, so risk averse individuals will generate smaller utility values than the ones generated by SG. Rating scale of visual analogue scale (VAS). It consists of a single line with anchors representing best possible health and death. Survey respondents have to place their perceived differences between each health state. Due to its simplicity, is often used to make the patient familiar with comparing health states before performing SG or TTO methods. SG and TTO are more used than VAS, but as we said before, the latter is used to make the patients familiar with the methods. SG approach is more time consuming and difficult to understand than TTO. For this reason, TTO is a reliable and practical middle way. 10.3. Indirect methods Generic utility instruments. Three instruments are used: EQ-5D, SF-6D and the Health Utility Index (HUI). They are based on the public evaluation of a limited number of health states and develop of a scoring algorithm that is developed using econometric modeling or a multiplicative multi-attribute utility function to predict utilities for other health states not directly valued. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 40 Disease-specific utility instruments. Generate potentially sensitive disease-specific utilities. Early stage of development. Mapping utilities. Is used when a generic instrument is not available. It maps the descriptions from a disease-specific QoL instrument onto the utility algorithm of a generic instrument. Effectiveness, meta-analysis and QUALITY-ADJUSTED LIFE-YEARS 41 References 1. Wang (2006). Clinical Trials – A Practical Guide to Design, Analysis, and Reporting, Intention-To-Treat analysis; Pages 255 - 263. 2. Montori, Guyatt (2001). Intention-to-treat principle. Canadian Medical Association or its licensors. 3. Fergusson, Aaron, Guyatt, Hebert (2002). Post-randomization exclusions: the intention-totreat principle and excluding patients from analysis. British Medical Journal Volume 325; 4. Newell (1992). Intention-to-Treat analysis: Implications for Quantitative and Qualitative Research. International Journal of Epidemiology, vol. 21, no. 5. 5. Hollis, Campbell (1999). What is meant by intention-to-treat analysis? Survey of published randomized controlled trials. British Medical Journal, Volume 319. 6. Drummond (2005). Methods for the Economic Evaluation of Health Care Programmes 3rd edition. Oxford University Press, UK. Chapter 6: Cost-utility analysis. 7. Weinstein, Torrace, McGuire (2009). QALYs: The Basics. Value in Health, vol. 12, supplement 1. 8. Toley (2009). What are health utilities?. What is…? series. Health economics. 9. Hemingway (2009). What is a systemic review?. What is…? series. Evidence-based medicine. 10. Crombie (2009). What is meta-analysis?. What is…? series. Evidence-based medicine.