Supplementary Information (docx 473K)
advertisement
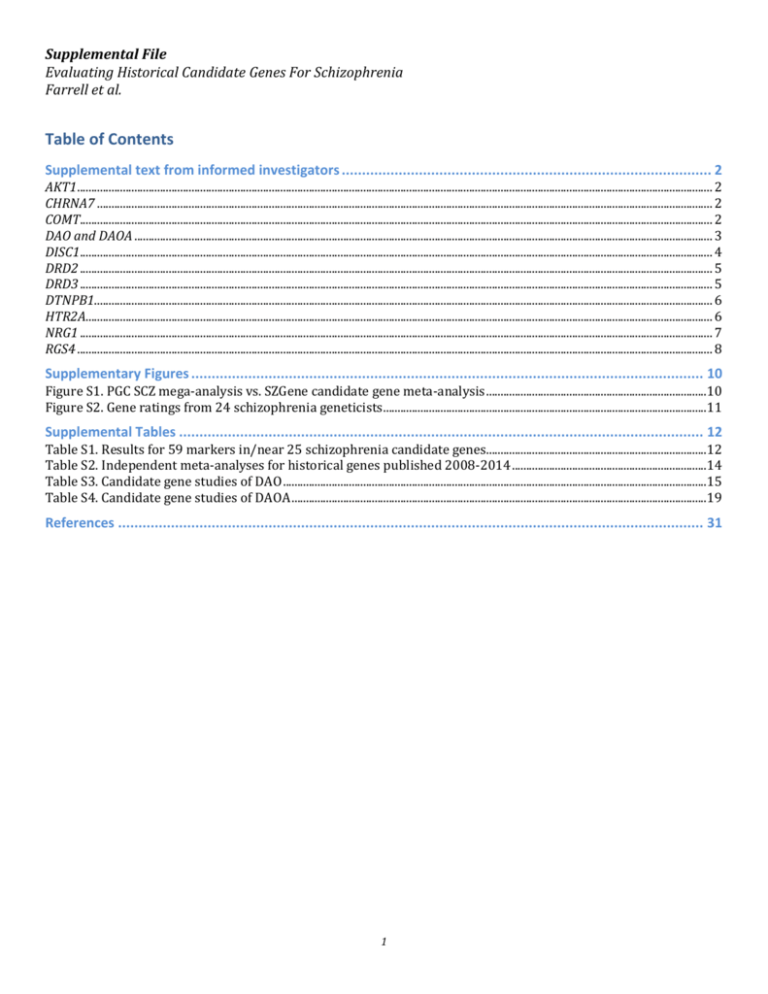
Supplemental File Evaluating Historical Candidate Genes For Schizophrenia Farrell et al. Table of Contents Supplemental text from informed investigators ........................................................................................... 2 AKT1.............................................................................................................................................................................................................................. 2 CHRNA7 ....................................................................................................................................................................................................................... 2 COMT............................................................................................................................................................................................................................. 2 DAO and DAOA .......................................................................................................................................................................................................... 3 DISC1............................................................................................................................................................................................................................. 4 DRD2 ............................................................................................................................................................................................................................. 5 DRD3 ............................................................................................................................................................................................................................. 5 DTNPB1........................................................................................................................................................................................................................ 6 HTR2A........................................................................................................................................................................................................................... 6 NRG1 ............................................................................................................................................................................................................................. 7 RGS4 .............................................................................................................................................................................................................................. 8 Supplementary Figures .............................................................................................................................. 10 Figure S1. PGC SCZ mega-analysis vs. SZGene candidate gene meta-analysis .............................................................................10 Figure S2. Gene ratings from 24 schizophrenia geneticists .................................................................................................................11 Supplemental Tables ................................................................................................................................. 12 Table S1. Results for 59 markers in/near 25 schizophrenia candidate genes.............................................................................12 Table S2. Independent meta-analyses for historical genes published 2008-2014 ....................................................................14 Table S3. Candidate gene studies of DAO ....................................................................................................................................................15 Table S4. Candidate gene studies of DAOA .................................................................................................................................................19 References ................................................................................................................................................ 31 1 Supplemental text from informed investigators AKT1 Personal communication from Drs Joseph Gogos and Maria Karayiorgou (Columbia University, New York, NY, USA). Authoritative investigator rating: 5 PGC schizophrenia PI mean rating: 2.5 The rating for AKT1 was 5 (very likely). We base this rating on the original integrative biological data, subsequent work in various genetic animal models (including unpublished work from our labs) as well as gene network analysis that implicates AKT1/GSK3beta signaling as a major node connected to many SCZ candidate genes. 1,2 CHRNA7 Personal communication from Drs Robert Freedman and Sherry Leonard (University of Colorado, Denver, CO, USA). Authoritative investigator rating: 5 PGC schizophrenia PI mean rating: 2.9 Linkage to schizophrenia of the CHRNA7 gene, which codes for the α7-nicotinic receptor subunit, was first observed using a physiological endophenotype, auditory P50 evoked potential inhibition, that had been previously associated with schizophrenia and α-7 nicotinic receptor function (LOD 5.2) 3. Subsequent study showed association of both schizophrenia and the P50 endophenotype with SNPs in the proximal CHRNA7 promoter that decrease expression in vitro 4. This finding is consonant with several reports of decreased expression of α7-nicotinic receptor subunits in post mortem schizophrenia samples 5. A SNP in the more distal promoter has the most significant reported association, P=0.0009, African-American; P=0.013, Caucasian 6. Perhaps the most persuasive evidence for the CHRNA7 gene’s role in schizophrenia is the well-replicated finding of 15q13.3 CNV CHRNA7 deletions 7,8. CHRFAM7A, a partial duplication containing CHRNA7 exons 5-10, which is only found in humans, also maps nearby on 15q 9, and polymorphisms in CHRFAM7A are associated with schizophrenia (Sinkus 2009). CHRFAM7A product subunits can associate with CHRNA7 subunits as part of the α7-nicotinic acetylcholine receptor, which is a pentameric ring. Compared to a receptor composed entirely of CHRNA7 subunits, those incorporating CHRFAM7A subunits have significantly decreased ion flux, which suggests that CHRFAM7A may limit CHRNA7 function and thereby have an additional pathological role 10. COMT Personal communication from Dr Daniel R Weinberger (Lieber Institute, Johns Hopkins University School of Medicine). Authoritative investigator rating: 1 (main effect), 4 (epistatic effect) PGC schizophrenia PI mean rating: 2.4 Catechol-o-methyl transferase (COMT) has been perhaps the most extensively studied candidate gene in behavioral genetics since the initial report of an association with schizophrenia in 1996 11. Its popularity is based on many factors, including that it is mapped to an early schizophrenia linkage region on chromosome 22, it is contained within the 22q11 hemi-deletion critical region of the VCFS syndrome, and it is involved in catecholamine metabolism, a virtually sacrosanct biochemistry of neurotransmitters related to psychiatric disorders and their treatment. Since the initial report, over twenty independent case control studies found significant association with common COMT variants and psychosis, with another ten family based studies also showing significant association 12. Even an early genome-wide association study found a nominally significant signal in COMT 13. COMT shows significant association signals in the current SZGene meta-analysis 12 and has been linked with psychosis in cases with velocardiofacial syndrome (VCFS) 14,15. COMT also has been shown in several studies to interact with environmental risk factors associated with psychosis (e.g. cannabis) 16,17. Most of the early studies 2 focused on a common coding variant with established effect on enzyme activity, the Val158Met variation, but recent reports have emphasized signals in other polymorphisms. In addition to these associations with clinical diagnosis, beginning with the first study of association of COMT with cognition and cortical physiology 18 and with evidence that COMT is primarily involved in cortical dopamine flux 19, over 50 reports have documented a role for COMT in cortical information processing, establishing a biologic basis for understanding a potential mechanism of association of COMT with behavioral syndromes. Virtually all of the clinical associations of COMT with aspects of cortical function related to cognition and emotion have been confirmed in studies of genetically engineered mice with analogous COMT variation 20-22. Given these multiple positive reports of clinical association with albeit relatively small samples and the elaboration of a biological mechanism by which COMT could influence brain function linked to psychosis and other psychiatric disorders, why has association been so decidedly negative at the single locus level in the current incarnation of GWAS data? And is the prior evidence of a role of COMT in brain function related to psychiatric disorders a “red herring”? A reasoned response to these questions is that the jury is still out on both counts. The failure to find association in the current GWAS data may reflect interactions with modifying factors and the biologic heterogeneity of functional variants within the COMT gene that are not accounted for in the current GWAS single locus association analyses. Several functional polymorphisms within the COMT gene have been implicated 23-25, each acting via different molecular mechanisms, so their cumulative effects are complex. A recent study of molecular haplotypes in individuals with VCFS showed that alleles at one variant have paradoxical effects on COMT expression and enzyme activity in the context of alleles at other variants 14. There are considerable population differences in allele frequencies at the various functional polymorphisms within COMT, adding insuperable heterogeneity to single locus analyses. Sex effects on COMT associations also have been identified in clinical studies and in mice 20,22. Another complication with association with COMT involves the biology of cortical dopamine function. The relationship between cortical function and dopamine activity is nonlinear 26 and thus, predictable relationships between single SNP allele load and clinical biology may require multilocus and nonlinear (e.g. epistatic) models. A recent study in mice and in humans demonstrated that the COMT Val158Met polymorphism shows opposite associations with cortical function depending on haplotype at another gene (DTNBP1) that also influences cortical dopamine signaling 27. Interestingly, one meta-analysis of COMT associations with psychosis suggested that the strongest signal was a protective association with heterozygosity at the Val158Met variant, implying that in a given context (i.e. varying genomes and environments), too much or too little COMT mediated cortical dopamine could have similar associations 28. Such effects would literally obliterate single locus association in heterogeneous samples such as current GWAS. It is reasonable to assume that COMT is a genetic risk factor for psychiatric syndromes linked to cortical dopamine signaling, but statistical confirmation of this association will require multifactorial and probably nonlinear genetic models that address the critical role of context, both genomic and environmental. DAO and DAOA Personal communication from Drs Marcella Rietschel and Jens Treutlein (Central Institute of Mental Health, University of Heidelberg, Mannheim, Germany). Authoritative investigator rating: 3, 3 PGC schizophrenia PI mean rating: 2.2, 2.0 See Tables S2 and S3. The first report of an association between schizophrenia and variants in the genes d-amino acid oxidase (DAO) and d-amino acid oxidase activator (DAOA, alias G72) was published in 2002. In a sample of 213 schizophrenia patients and 241 controls from Canada, Chumakov et al. performed a systematic investigation of SNPs in a 5-Mb segment of the 13q34 chromosomal region. Two of the six nominally significant variants from this study were subsequently replicated in an independent schizophrenia sample 29, and in a sample of patients with bipolar disorder 30. These two variants were located in the DAOA gene, whose product interacts with DAO. DAO metabolizes D-serine, which is an 3 activator of NMDA glutamate receptors, and glutamatergic signaling has been implicated in the etiology of psychotic symptoms and schizophrenia. Since these genes were plausible candidates for psychiatric disorders, numerous studies attempted to corroborate their involvement in schizophrenia, bipolar disorder, and related traits. To our knowledge, a total of ~76 studies for DAOA and ~25 studies for DAO have tested markers in schizophrenia and related phenotypes. However, the findings have been inconsistent. Furthermore, few findings remained significant following correction for the number of SNPs tested. Several meta-analyses of the role of DAOA in schizophrenia and bipolar disorder have been published. The meta-analysis by Detera-Wadleigh & McMahon in 2006 31 included seven studies of schizophrenia and three studies of bipolar disorder, and found association between schizophrenia and the markers M12, M15, M22, M23, and M24. The meta-analysis by Shi et al. in 2008 32 included 23 studies, and detected association between schizophrenia and the markers M18, M22, and M24. The meta-analysis by Müller et al. in 2011 33 included 24 studies of schizophrenia and 11 studies of bipolar disorder, and revealed association between schizophrenia and the marker M15. The most recent meta-analysis by Tan et al. in 2014 34 included 46 studies (17,515 cases and 25,189 controls), and tested the markers M15, M18, and M23. However, no significant finding was identified. In summary, the available data provide no support for the hypothesis that variants in DAO or DAOA confer risk for schizophrenia. This view is supported by the observation that the number of positive findings in meta-analyses is inversely proportional to the number of studies examined. It could be argued, however, that since the anticipated effect sizes are small, and that the effects of genetic variants will be blurred by interaction with other factors, this inverse relationship is unsurprising when increasing heterogeneity of the samples. Interestingly, research has indicated possible association between specific markers in DAO and DAOA and more homogenous patient groups, e.g. association between markers M23 and M24 in Europeans. Given their function, and the fact that genetic variation in these genes is unlikely to occur without any effect, DAO and DAOA remain plausible candidate genes for schizophrenia. However, confirmation of this hypothesis can not be made on the basis on the available data but will require further analyses. DISC1 Personal communication from Dr David Porteous (Centre for Genomic and Experimental Medicine, Institute of Genetics and Molecular Medicine, University of Edinburgh, Western General Hospital, Crewe Road, Edinburgh, UK). Authoritative investigator rating: 4.5 PGC schizophrenia PI mean rating: 2.7 Disrupted in Schizophrenia 1 (DISC1) is an archetypal positional candidate gene, disrupted by a balanced t(1;11) translocation that is linked, with genome-wide significance, to schizophrenia alone (LOD = 3.6) and to schizophrenia plus related mental illness (MLOD = 7.1) in a large Scottish family 35,36. Thus, the DISC1 locus meets the primary genetic criterion for candidature and merits biological validation. DISC1 encodes a scaffold protein regulating neuronal proliferation, migration, integration and signaling, spine formation and synapse maintenance-neurobiology that aligns well with current concepts in schizophrenia 37. Moreover, DISC1 protein binding partners, including PDE4B, PCM1 and NDE1, are independently implicated as genetic risk factors for schizophrenia and related major mental illness through cytogenetics, copy number variation and linkage (reviewed in 38). Rare DISC1 amino acid substitution variants have been reported in schizophrenia 39, recurrent major depressive disorder, segregating with psychiatric disorder 40 and autism 41. In contrast, meta-analysis of common DISC1 SNPs has found no evidence of genome-wide significant association with schizophrenia 42 and DISC1 does not appear on the GWAS list of significant associations for schizophrenia 43. The absence of evidence from 4 GWAS is, of course, not evidence of absence of effect; while GWAS can identify ancient variants common to all populations, variants that are moderate to rare and/or population-specific and/or disorder subtype-specific for illness will fall below the accepted level of genome wide significance. A further limitation of GWAS and many CNV studies is that they do not identify functional variants directly. In this regard, structure-function analysis of DISC1 has proved fruitful, demonstrating biological pleiotropy and epistasis that is hidden from current GWAS analysis 44. There is good evidence from human 45,46 and mouse 47 studies that modulation of DISC1 expression affects systems level changes in biologically relevant pathways and clinical endophenotypes. Amino acid substitution polymorphisms and rare variants have been shown experimentally to modulate structural and oligomerisation properties of DISC1 and to modulate or abrogate relevant biological traits, including -catenin signaling, ATF4-dependent stress response and mitochondrial trafficking 48-51. Thus, DISC1 is analogous to the examples of APP and PSEN1 and 2 in Alzheimer’s disease 52; risk genes that may score low on GWAS criteria, but high on rare variant criteria do offer valuable and direct etiological insight into psychiatric disorders. Score = 4.5/5 (genome wide significant by linkage; functional genetic variants and biological evidence for relevance). DRD2 Personal communication from Drs James Kennedy and Clement Zia (Centre for Addiction and Mental Health, University of Toronto, Toronto, Ontario, Canada). Authoritative investigator rating: 4 PGC schizophrenia PI mean rating: 4.1 One of the top hits in the most recent Psychiatric Genomics Consortium GWAS meta-analysis of schizophrenia is rs2514218, located approximately 50kb upstream of DRD2. There is substantial neurobiological evidence supporting a role of the dopamine D2 receptor in schizophrenia, most notably the fact that all efficacious antipsychotic medications have significant D2 antagonism (Seeman et al, 1975). Furthermore, schizophrenia patients show elevated striatal D2 levels (e.g., SPECT 53) as well as D2 receptor super-sensitivity 54,55. These findings collectively suggest that rs2514218 and/or correlated variants in regulatory sites may create elevated risk for schizophrenia by giving rise to higher D2 receptor expression. While rs2514218 does not appear to have a strong functional role based on ENCODE data 56-58, molecular studies using tissues from specific brain regions will clarify the molecular mechanisms of this genome-wide significant association. Interrogation of DRD2 regulatory sites for possible association with the increased striatal D2 levels in schizophrenia patients may be useful. D2 receptor occupancy is correlated with therapeutic efficacy for antipsychotics 59. Putative functional single-nucleotide polymorphisms in DRD2 have been implicated in antipsychotic response (rs1799732/141C insertion/deletion 60) and side effects including rs1800497/TaqIA in tardive dyskinesia 61,62 and rs6277/C957T 63 in antipsychotic-induced weight gain. However, association findings of these and other DRD2 markers in the diagnosis of schizophrenia have been mixed 64, suggesting that the role of D2 in the etiopathophysiology of schizophrenia may be modulatory rather than directly causative. Interestingly, ZNF804A, another one of the top hits in the PGC2 GWAS meta-analysis, may regulate the expression of DRD2 in addition to other schizophrenia candidate genes 65. Given this observation as well as the complexity of D2-mediated signaling, further DRD2 gene-based studies as well as gene-gene interaction and pathway analyses are required to decipher the role of DRD2 in schizophrenia. Based on its welldocumented therapeutic role, we can be cautiously optimistic that DRD2 may become one of the more meaningful GWAS hits in terms of translational impact. DRD3 Personal communication from Dr Michael Owen (Cardiff University, Cardiff, Wales, UK). Authoritative investigator rating: 2 PGC schizophrenia PI mean rating: 2.3 5 This was an excellent functional candidate gene for schizophrenia given its role in pharmacology and its location in the brain. In the light of what we know now about the genetic architecture of schizophrenia, the initial studies and even the several meta-analyses that we, and others, conducted were underpowered. The updated results of meta-analysis of candidate gene studies in SZGene and the findings from PGC2 provide no support for the hypothesis that common genetic variants in this gene confer risk of schizophrenia. DTNPB1 Personal communication from Dr Brien Riley (Virginia Institute of Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, VA, USA). Authoritative investigator rating: 2 PGC schizophrenia PI mean rating: 2.4 The score is based on the following rationale. If a “1” signifies a locus for which there has never been any credible support (i.e., null expectation), there is some evidence for a locus in this region of chr 6 in family studies and it does not seem to me, although this is intuitive rather than empirical, that the chr 6p signal is being driven by the HLA region signal, although it is certainly possible. However, the pattern of different haplotypes associated in almost every sample examined strongly suggests that there is no stable association signal detectable at this locus in European samples. I think this is also the answer to the publication pattern question: the focus in the early days of association studies was on any signal from a locus of interest with very little attention paid to whether the specific signal observed was consistent (i.e., really represented replication). HTR2A Personal communication from Drs Jiang Li and Herbert Y. Meltzer (Northwestern University, Feinberg School of Medicine). Authoritative investigator rating: 4 PGC schizophrenia PI mean rating: 2.3 Three HTR2A polymorphisms, rs6311, rs6313, rs6314, have been widely investigated in association studies with schizophrenia. rs6311 (-1438G>A), located in the promoter region of HTR2A, is in strong linkage disequilibrium with rs6313 (102T>C), a synonymous mutation. rs6314 (His452Tyr), the most common missense variant, is located at the C-terminal region. It has been implicated in binding of accessory/scaffolding proteins as well as G protein-coupled receptor desensitization and internalization 66. rs6313, a silent substitution, has been controversially associated with schizophrenia 67-75. It has been associated with a subgroup of schizophrenia patients characterized by poor long-term outcome and poor response to typical antipsychotic drugs 76. Prepulse inhibition and habituation has been reported to be modulated by rs6311/rs6313 in schizophrenia, suggesting alterations in brain HTR2A may contributes to the prepulse inhibition deficits present in some patients with schizophrenia. It conferred an increased risk for psychosis in a meta-analysis of Alzheimer dementia subjects 77. These studies support the conclusion that rs6311/rs6313 may contribute to an endophenotype characterized by poor treatment response to clozapine, Only Arranz et al. reported positive finding with regard to clozapine response in association with rs6311/rs6313 78,79. Others cannot replicate their findings 80-85. A metaanalysis of the association between HTR2A polymorphisms and clozapine response showed a deviation from theoretically expected pattern in the funnel plots where studies should converge with increasing sample size, suggesting a possibility of publication bias. The weighted mean of the odds ratios of all studies on HTR2A genotypes including rs6311/rs6313/rs6314 was 1.7, thus, predicting only a minor influence of this gene on clozapine response86. rs6314 has been associated with hippocampal volume 87 and novelty processing in humans 88. It has been shown to predict poor response to the atypical antipsychotic drug, clozapine, in some 78-80,89, but not all studies 82-84. A recent study examined evidence from functional imaging and clinical data and reported 6 that rs6314 is associated with prefrontal function and response of negative symptoms to olanzapine, a clozapine-like atypical antipsychotic drug 90. Functional studies have suggested that rs6314 may impact on calcium signaling and mobilization as well as on reduced activation of phospholipases C and D, resulting in markedly reduced intracellular signaling capacity 91,92. An in silico-based bioinformatics analysis predict that rs6314 alters patterns of splicing with possible effects on HTR2A expression 90. Based on an early study of allelic expression imbalance (AEI) in 23 adult brain tissue heterozygous for rs6313, Bray et al. asserted that the HTR2A locus does not contain common variants affecting mRNA levels in adult brain 93. However, Smith et al. recently combined in vitro gene-reporter assay and AEI analysis with next-generation sequencing technology to show that significant AEI can be observed only in the extended form of HTR2A harboring rs6311, but not in any mature mRNA transcripts. The translational efficiency of long UTR is higher than short UTR, suggesting that rs6311 decreases usage of an upstream transcription start site encoding a longer 5’UTR with greater translational efficiency 94. According to postmortem prefrontal cortex samples from BrainCloud 95, promoter SNP rs6311(LD with rs6313) is also a methylation QTL for HTR2A as it is highly correlated with CpG methylation at the HTR2A across ethnicity 94, further suggesting potential epigenetic effect of this polymorphism on gene expression. In conclusion, the common functional variants including rs6311, rs6313 and rs6314 of HTR2A make a limited but definite contribution to the risk of schizophrenia and treatment response to clozapine. Controversial results warrant more extensive investigation. Further study should focus on the association with endophenotypes instead of a complex disease trait alone, or treatment response in general, as the biological and pharmacological background influencing those traits could be largely heterogeneous. Further study should also focus on the interaction between the genetic variants and environmental factors in the context of the association with schizophrenia or drug response. With increased sample size, not only common variants, but also rare mutations should also be included in analysis to determine the accumulated genetic burden in conferring the risk for the disease or endophenotypes. NRG1 Personal communication from Dr Amanda Law (University of Colorado, Denver, CO, USA). Authoritative investigator rating: 3 PGC schizophrenia PI mean rating: 2.9 Neuregulin 1 (NRG1) is an essential neurotrophin, a critical mediator of neurodevelopment, synaptic plasticity and neocortical function and one of the most researched candidate susceptibility genes for schizophrenia. NRG1 maps to 8p21-p12, a chromosomal region with prior evidence of genome-wide linkage to schizophrenia 96-98. Association to common genetic variation in NRG1 and schizophrenia was first reported in the landmark study of Stefansson and colleagues, in 2002 99, whereby genome-wide linkage scans, extensive fine mapping and association analyses of extended Icelandic pedigrees identified a 290kb risk haplotype in the 5’ region of NRG1 (HAPICE); a finding confirmed in Scottish 100 and Irish 101 populations. Subsequent association has been validated in three separate meta-analyses 102-104. Since the original report, 30 independent studies have reported significant association to common NRG1 variants (most notably complex haplotypes) and schizophrenia in European, Asian and African populations 12. While NRG1 did not show significant association in the current SZGene meta-analysis 12, more recent updates list NRG1 as positive 12 and recent analyses of three European genome-wide data sets provide support for association of NRG1 HAPICE and additional novel haplotypes with schizophrenia 105. Nevertheless, it is important to note that the associated haplotype or variants are not always HAPICE, (a finding likely related to population heterogeneity), no obviously pathogenic mutations or copy number variations have been identified in NRG1 and several negative studies exist12,106. In addition to statistical associations, the evidence in favor of NRG1 as a schizophrenia risk gene is strengthened by biological findings. First, risk polymorphisms in NRG1 are associated in humans with multiple neurobiological phenotypes relevant to schizophrenia, including cognitive function, prefrontal 7 cortical physiology, and neocortical development 107-109. Second, neurobiological roles of NRG1 are relevant to the disease process of schizophrenia, including key roles in neuronal migration, neurotransmitter function, cortical inhibitory circuit development and myelination 106. Third, NRG1 gene expression is altered in the brain of patients with schizophrenia and related to risk polymorphisms 110112; and fourth, mutation of NRG1 in rodents produces abnormalities in several behavioral domains relevant to schizophrenia, including learning, memory, cognitive function and sociability 99,113-115. Interestingly, genetic manipulations in mice 99,113-115 demonstrate that ‘overexpression’ or ‘knockdown’ of the NRG1 gene leads to similar schizophrenia-related behaviors, suggesting a non-linear, inverted-U model of NRG1 signaling and schizophrenia, an observation which may have important implications for genetic association studies. Even so, despite multiple positive reports of clinical association, the distinct neurobiological relevance of NRG1’s functions to neurodevelopment and cortical function, and identification of potential biological mechanisms of risk, large genome-wide association studies of schizophrenia have failed to provide corroborative evidence of association to NRG1. Lack of support from this approach raises several important questions regarding the validity of pre-GWAS genetic associations to NRG1; challenges whether NRG1 is a reliable, disease-relevant genetic factor for schizophrenia, and raises the issue of whether current GWAS single-marker association approaches are capable of identifying association to complex genetic loci. It would be only pragmatic to conclude that the current data are inconclusive as to whether NRG1 is a significant genetic risk factor for schizophrenia. However, failure to find association to NRG1 in current schizophrenia GWAS may relate to several factors, including: limitations of singlemarker analysis; noting that the majority of previous associations to NRG1 are to complex and diverse haplotypes, not single nucleotide variants 99-104,106; heterogeneity; noting that original isolation of the gene was in small, relatively homogenous populations 99-101 and heterogeneity within the 1.2Mb, vastly complex gene 106 has been shown to be pervasive within and across larger populations 104,106; geneenvironment interactions; noting the significant interaction of NRG1 with environmental risk variables, including obstetric complications, psychosocial stress and cannabis 116,117, and finally gene-gene interactions; noting variant interactions between NRG1 and genes in the neureuglin signaling pathway to increase risk 108,118. Despite the failure of current GWAS to confirm association to NRG1, previous data support critical roles for NRG1 in neurodevelopmental and neurobehavioral functions relevant to schizophrenia. The ‘pre’- ‘post-GWAS’ validity conundrum will only likely resolve for NRG1 with the application of multifactorial methods for GWAS data analysis which account for association in the context of genetic background, genetic interplay and environmental modification. RGS4 Personal communication from Dr Karoly Mirnics (Vanderbilt University, Nashville, KY, USA). Authoritative investigator rating: 2 PGC schizophrenia PI mean rating: 2.1 Based on the current golden standards, the evidence that RGS4 sequence variants predispose to schizophrenia is weak. However, this does not mean that RGS4 is not important for the disease pathophysiology. These two categories should be always considered separately as a gene that has no sequence variant predisposing toward a disease can be still critical for the overall progression of pathology and emergence of symptoms. RGS4, just like most of the initial schizophrenia candidate genes, did not show positive association in GWA studies (including BDNF, COMT, RELN and others), but the evidence for their involvement in the disease progression and schizophrenia-associated endophenotypes can be considered very strong. The following genetic studies support RGS4 as a schizophrenia susceptibility gene 119-129. The following candidate gene studies (in addition to GWAS) do not support the notion that sequence variants of RGS4 predispose to schizophrenia 130-139. The pathophysiological evidence supporting a role for RGS4 in schizophrenia include: 1) Decreased RGS4 brain transcript expression in schizophrenia 140-143 8 2) 3) 4) 5) 6) 7) 8) 9) 10) Decreased RGS4 brain protein expression in schizophrenia 144 Plausibility of biological effects – regulation of GPCR signaling 145-150 Genetic association/DNA methylation with suicide attempts in schizophrenia 119 Converging “hub” gene and interaction with other schizophrenia susceptibility genes 121,151-156 Cortical thickness associated with genotype 125 Brain connectivity associated with genotype 157 Working memory/cognitive performance associated with genotype 120,158-160 Medication efficacy depending on genotype 161,162 Antipsychotic treatment increases RGS4 membrane expression 163 9 Supplementary Figures Figure S1. PGC SCZ mega-analysis vs. SZGene candidate gene meta-analysis For each gene, the x-axis is the –log10(P) from the SZGene meta-analysis and the y-axis is the –log10(P) from the PGC mega-analysis for a 25 kb window encompassing the gene. The data points are sized and colored by the number of pre-GWAS candidate gene studies as reported in Table 1. The horizontal line indicates the genome-wide significance threshold (5x10-8). 10 Figure S2. Gene ratings from 24 schizophrenia geneticists The x-axis labels indicate the gene being rated as a risk factor for schizophrenia and the y-axis indicates the distribution of ratings. The vertical length of a colored bar represents the proportion of investigators giving a particular rating to that gene. The rating color scheme is in the legend on the right. The ratings were a summary judgment of the current status of a gene as a genetic risk factor for schizophrenia (1=very unlikely and 5=very likely). On the far left, “equal distribution reference” provides a reference bar size for equal distribution amongst raters for a given gene. The absence of a particular colored bar indicates that none of the investigators gave that rating for a gene. 11 Supplemental Tables Table S1. Results for 59 markers in/near 25 schizophrenia candidate genes Gene Marker Studies Ncase AKT1 APOE BDNF rs3730358 .2/3/4 270C/T rs6265 rs28531779 rs737865 rs165599 rs4680 rs3918346 rs947267 rs778294 rs3916967 rs3916965 rs778293 rs1421292 rs3918342 rs2391191 rs1322784 rs1000731 rs999710 rs6675281 rs3738401 rs821616 rs1800497 rs1799732 rs1801028 rs6280 rs4646983 rs2619528 rs909706 rs2619522 rs2619538 rs1018381 rs2005976 rs760761 rs2619539 rs1011313 rs3213207 rs2228595 2 15 7 9 2 6 8 28 5 6 6 8 9 9 9 10 11 6 6 7 8 9 9 10 10 16 44 3 6 7 7 7 9 9 10 10 11 13 3 2543 1549 1242 2397 861 4552 5359 7622 1364 1524 3334 3574 4058 4348 4712 3968 5083 3297 3412 3608 3896 4705 4705 1228 3457 4160 6031 406 3370 4081 4101 4332 4227 4761 4560 5451 5385 6305 1227 CHRNA7 COMT DAO DAOA DISC1 DRD2 DRD3 DRD4 DTNBP1 GRM3 SZG OR (95% CI) 1.01 (0.91-1.13) 0.99 (0.82-1.20) 0.68 (0.52-0.87) 0.95 (0.87-1.04) 0.97 (0.72-1.30) 1.00 (0.95-1.06) 1.00 (0.95-1.05) 1.00 (0.96-1.05) 1.00 (0.89-1.12) 1.05 (0.95-1.16) 0.96 (0.89-1.03) 1.00 (0.94-1.07) 0.95 (0.90-1.01) 1.00 (0.94-1.06) 1.02 (0.97-1.08) 0.99 (0.94-1.05) 0.97 (0.92-1.02) 0.99 (0.92-1.07) 1.06 (0.98-1.14) 1.07 (1.00-1.14) 1.03 (0.95-1.12) 1.05 (0.99-1.12) 1.00 (0.94-1.06) 0.90 (0.79-1.03) 0.92 (0.82-1.02) 0.85 (0.71-1.03) 1.03 (0.97-1.08) 1.13 (0.76-1.67) 1.01 (0.93-1.09) 1.04 (0.97-1.10) 1.01 (0.93-1.08) 1.01 (0.95-1.07) 1.04 (0.93-1.15) 0.95 (0.89-1.02) 0.97 (0.90-1.04) 1.04 (0.99-1.10) 1.12 (1.02-1.23) 1.10 (1.02-1.19) 1.21 (0.96-1.52) SZG P 0.82 0.95 0.0028 0.29 0.82 0.96 0.99 0.92 0.94 0.33 0.22 0.97 0.11 0.93 0.37 0.80 0.26 0.81 0.12 0.045 0.48 0.095 0.93 0.14 0.12 0.10 0.33 0.56 0.89 0.29 0.88 0.80 0.51 0.17 0.37 0.12 0.015 0.015 0.099 PGC OR (95% CI) 1.02 (0.99-1.06) 0.99 (0.96-1.02) † 1.01 (0.97-1.06) † 0.95 (0.92-0.97) 1.01 (0.96-1.05) 0.98 (0.96-1.01) 1.00 (0.99-1.03) 0.99 (0.97-1.01) 1.03 (1.00-1.05) 0.99 (0.97-1.01) 1.00 (0.98-1.03) 1.00 (0.98-1.02) 1.00 (0.98-1.02) 1.01 (0.99-1.03) 1.00 (0.98-1.02) 1.00 (0.98-1.02) 1.00 (0.98-1.02) 1.00 (0.98-1.03) 1.02 (0.99-1.04) 1.01 (0.99-1.03) 0.98 (0.95-1.01) 1.00 (0.97-1.02) 1.00 (0.98-1.03) 1.00 (0.98-1.03) No data 0.95 (0.89-1.03) 0.99 (0.97-1.01) No data 0.97 (0.94-0.99) 1.01 (0.99-1.03) 1.03 (1.00-1.06) 1.00 (0.98-1.03) 0.99 (0.96-1.03) 0.97 (0.95-1.00) 0.97 (0.95-1.00) 0.99 (0.97-1.01) 0.99 (0.96-1.03) 1.04 (1.01-1.08) 1.01 (0.97-1.06) 12 PGC P 0.17 0.48 0.55 8.0e-5 0.79 0.17 0.29 0.56 0.035 0.30 0.82 0.88 0.96 0.53 0.81 0.77 0.92 0.82 0.22 0.29 0.13 0.68 0.76 0.88 0.22 0.31 0.019 0.35 0.020 0.74 0.72 0.022 0.021 0.32 0.78 0.012 0.58 PGC Pmin ±25kb 3.0e-4 0.0095 8.0e-5 PGC SNPs ±25kb 330 195 279 0.0096 0.0065 540 419 0.00040 0.015 390 360 0.00095 1652 8.3e-9 369 0.015 0.0026 0.0073 403 287 574 1.0e-10 677 HTR2A KCNN3 MTHFR NOTCH4 NRG1 PPP3CC PRODH RGS4 SLC6A3 SLC6A4 TNF ZDHHC8 rs6311 rs6313 1333T/C rs1801131 rs1801133 rs367398 rs6994992 rs62510682 rs35753505 rs7837713 rs383964 rs10917670 rs951439 rs2661319 rs951436 VNTR 5-HTTVNTR 5-HTTLPR rs1800629 rs175174 7 26 1 8 11 5 6 6 13 1 4 7 7 8 9 6 9 15 7 4 2717 6384 184 1964 2529 1045 3999 4192 5874 1870 1453 4377 4519 4827 5049 731 1951 2652 1081 1461 1.14 (1.06-1.23) 0.98 (0.93-1.03) 1.12 (0.33-3.76) 0.91 (0.84-0.99) 1.09 (1.01-1.17) 1.00 (0.87-1.15) 1.06 (0.99-1.13) 0.94 (0.88-1.01) 0.95 (0.90-1.01) 0.99 (0.81-1.21) 1.09 (0.88-1.35) 0.94 (0.89-0.99) 0.97 (0.91-1.03) 0.93 (0.88-0.99) 1.01 (0.96-1.07) 0.97 (0.82-1.16) 1.11 (1.01-1.21) 1.01 (0.94-1.09) 1.00 (0.86-1.17) 1.00 (0.90-1.11) 0.0005 0.40 0.86 0.031 0.026 0.99 0.087 0.074 0.076 0.91 0.42 0.033 0.28 0.013 0.73 0.77 0.024 0.75 0.98 0.96 1.01 (0.99-1.04) 1.01 (0.99-1.04) 0.95 (0.93-0.98) † 1.02 (1.00-1.05) 1.01 (0.98-1.03) No data 1.01 (0.98-1.03) 0.97 (0.95-1.00) 1.00 (0.97-1.02) 1.01 (0.97-1.06) 1.02 (0.97-1.07) 1.00 (0.97-1.02) 1.00 (0.97-1.02) 1.01 (0.99-1.03) 1.01 (0.99-1.03) 0.98 (0.94-1.01) † 0.91 (0.86-0.96) † 1.03 (1.00-1.07) † 0.91 (0.89-0.94) 0.98 (0.96-1.01) 0.18 0.18 3.3e-5 0.030 0.55 0.61 0.024 0.69 0.62 0.41 0.66 0.67 0.47 0.38 0.24 4.2e-4 0.058 5.6e-10 0.17 (rs12704290) 0.011 444 6.8e-6 0.016 713 443 1.1e-18 0.0012 560 4586 0.00017 0.0092 0.0061 387 445 238 0.0103 4.2e-4 497 207 1.7e-18 4.1e-6 294 314 We obtained the SZGene 164 database (http://www.szgene.org) in 11/2009 (active work on SZGene stopped in 12/2011). We selected all study for the 25 genes in Table 1 that met inclusion criteria: (a) case/control design, (b) published before 2009 (we verified that no GWAS were included), (c) subjects of European ancestry, (d) biallelic markers and complete data. We selected markers that had been in ≥5 studies. If a gene did not have a marker with ≥5 studies, we selected the marker with the largest number of studies so that all 25 genes had at least one genetic marker. We conducted a fixed-effect metaanalysis for each marker. The first six columns show characteristics derived from SZGene. Gene=standard gene name. Marker=name of genetic variant (converted to rs IDs where possible). Studies=SZGene studies that met inclusion criteria. Ncase=sum of cases. SZG OR=odds ratio (OR) and 95% confidence interval (CI) from the SZGene meta-analysis. SZG P=meta-analysis P-value. The next four columns show results from the PGC schizophrenia megaanalysis. 165 PGC OR=OR and 95% CI. PGC P= P-value. PGC Pmin=minimum P-value ±25 kb of a gene. PGC SNPs=SNPs ±25 kb of the gene. Alleles were harmonized between SZGene and PGC so that the ORs are comparable. The PGC and SZGene results are mostly for the same SNP but, for markers that were not SNPs (†), all PGC SNP results within a range encompassing the variant were obtained, and the one with smallest P-value is shown (BDNF 270C/T, SLC6A3 VNTR, SLC6A4 5-HTTLPR, SLC6A4 5-HTTVNTR, APOE rs429358/rs7412, and KCNN3 1333T/C). 13 Table S2. Independent meta-analyses for historical genes published 2008-2014 Gene PMID rSID Year Lead Author OR P Note AKT1 19931325 rs3730358 2010 Lee 1.02 (0.94-1.12) NS Pooled across multiple ancestries AKT1 23747160 rs3730358 2013 Loh 1.004(0.926–1.090) 0.92 Pooled across multiple ancestries AKT1 18715757 rs3730358 2008 Shi 0.951 (0.854–1.060) 0.36 EUR BDNF 23438165 270C/T 2013 Watanabe 1.20 (0.93–1.55) 0.16 EUR COMT 19329282 rs737865 2009 Okochi 1.041 (0.978-1.108) 0.21 Pooled across multiple ancestries COMT 19329282 rs165599 1.032 (0.960-1.108) 0.40 Pooled across multiple ancestries COMT 19329282 rs4680 0.989 (0.942-1.039) 0.67 Pooled across multiple ancestries COMT 20488458 rs4680 2011 Costas 0.947 (0.904-0.993) 0.023 Only over-dominant model reported DAOA 21443574 rs2391191 2011 Muller CI includes 1.0 NS Only forest plot presented DAOA 24447945 rs2391191 2014 Tan 0.96 (0.89-1.04) 0.30 EUR, random effects model DAOA 24447945 rs947267 0.97 (0.87-1.09) 0.63 EUR, fixed effects model DAOA 24447945 rs3918342 1.03 (0.92-1.15) 0.64 EUR, random effects model DISC1 21483435 rs6675281 0.93 EUR DISC1 21483435 rs3738401 0.11 EUR DISC1 21483435 rs821616 0.51 EUR DRD2 22370928 rs1801028 2012 Liu 1.47 (1.18-1.83) 0.0006 Pooled across multiple ancestries DRD3 18295456 rs6280 2008 Ma 1.017 (0.943-1.097) 0.67 EUR HTR2A 23857788 rs6313 2012 Jianliang 1.06 (0.96-1.17) NS Chinese HTR2A 24962835 rs6313 2014 Tan 0.994 (0.903-1.093) 0.89 EUR, random effects model HTR2A 23404241 rs6313 2013 Gu 1.12 (1.05-1.20) 0.28 EUR MTHFR 21185933 rs1801131 2011 Peerbooms 1.06 (0.99-1.15) NS Pooled across multiple ancestries MTHFR 24535549 rs1801133 2014 Nishi 1.16 (1.03-1.31) 0.014 Japanese, fixed effects model MTHFR 24938371 rs1801133 2014 Hu 1.07 (0.98–1.16) 0.14 EUR, random effects model MTHFR 24938371 rs1801131 1.07 (0.96–1.19) 0.22 EUR, random effects model NRG1 19362450 rs6994992 1.03(0.97–1.10) 0.33 Pooled across multiple ancestries NRG1 19362450 rs35753505 1.02(0.92–1.11) 0.76 Pooled across multiple ancestries NRG1 19362450 rs62510682 1.06(0.98–1.15) 0.12 Pooled across multiple ancestries 2012 2009 Mathieson Gong ZDHHC8 20661937 rs175174 2010 Xu 0.97 (0.88-1.07) 0.55 EUR, fixed effects model We searched PubMed for: ("schizophrenia"[MeSH Terms] OR "schizophrenia"[All Fields]) AND ("meta-analysis"[Publication Type] OR "meta-analysis as topic"[MeSH Terms] OR "meta-analysis"[All Fields]). All studies 2008-2014 were obtained. NS=not significant at 0.05. 14 Table S3. Candidate gene studies of DAO Paper Bass et al, 2009 Ancestry 3 of 4 grandparents were of English, Irish, Welsh, or Scottish descent Canadian, Russian Phenotype schizophrenia Sample size 431 cases 442 controls Variant rs3741775, rs3918346, rs2111902 P-value (OR) n.s. schizophrenia Korean homicidal behaviors in schizophrenia Corvin et al, 2007 Irish origin, i.e., Irish parents / grandparents schizophrenia 373 cases, 812 controls Fallin et al, 2005 Ashkenazi 274 trios Gaysina et al, 2010 UK, Canada schizophrenia, schizoaffective disorder bipolar I disorder bipolar disorder rs3741775, rs3918346, rs2111902, MDAAO-1 (SNP), MDAAO-2 (SNP), MDAAO-3 (SNP), rs3918347, rs888531 rs2070586, rs2070587, rs2070588, rs2111902, rs3918346, rs3741775, rs3825251 rs3741775, rs888531 rs3918346 rs2111902 rs2070587, rs2070588, rs3741775, rs3825251, rs3918346 5 SNPs typed rs3741775 four SNP markers were associated in Canadian samples Chung et al, 2007 213 (Canadian cases) 241 (Canadian controls) 183 (Russian cases) 183 (Russian controls) 188 cases Jönsson et al, 2009 Danish, Norwegian, Swedish schizophrenia rs2070587, rs2070588, rs3741775, rs3825251 n.s. Kim et al, 2010 Korean schizophrenia rs2070588, rs3741775, rs3825251, rs3918346, rs2111902, rs3220845 rs2070586 n.s. Chumakov et al, 2002 337 trios 515 cases (UK) 1316 controls (UK) 385 cases (Canada) 312 controls (Canada) 420 cases (Denmark) 1004 controls (Denmark) 162 cases (Norway) 177 controls (Norway) 255 cases (Sweden) 292 controls (Sweden) 96 cases 96 controls rs2070587 Liu et al, 2004 Chinese schizophrenia 547 cases 536 controls Liu et al, 2006 Taiwanese schizophrenia 218 families Ohnuma et al, 2009 Japanese schizophrenia 340 cases 340 controls Ohnuma et al, 2010 Japanese population schizophrenia Papagni et al, 2011 native English speakers regional activation and functional connectivity 1656 cases 1842 controls 121 subjects rs3918347 rs2070587, rs2070588, rs3825251, rs3918346, rs2111902 rs3741775 rs2111902, rs3918346, rs3741775 rs4964762, rs11114083, rs2070586, rs2111902, rs3918346, rs3741775, rs11114086, rs11114087, rs3825251, rs3918347, rs4964770 rs3825251, rs3918347, rs4964770 rs3918346 15 n.s. n.s. 0.0034 (OR 1.43) 0.018 (OR 1.29) n.s. highly suggestive (any SNP or haplotype p <0.01) n.s. 0.005 (allelic, females) 0.014 (genotypic, females) 0.025 (allelic, males) 0.002 (allelic, females) 0.005 (genotypic, females) 0.018 (allelic females) n.s. 0.000001 (OR 1.59) n.s. n.s. n.s. Cases with one or two copies of the T allele showed lower deactivation in the left precuneus and greater Prata et al, 2008 Roussos et al, 2011 Caucasian with at least 3 grandparents born in Scotland Greek in schizophrenia, bipolar I, controls bipolar affective disorder activation in the right posterior cingulate gyrus 213 cases, 197 controls rs2111902, rs3918346, rs3741775, rs3918347 n.s. sensorimotor gating, working memory, personality in healthy males 530 individuals rs2111902, rs3918346, rs3741775, rs3825251 rs4623951 n.s. Sacchetti et al, 2013 Italian schizophrenia 391 patients,488 controls Schumacher et al, 2004 German bipolar affective disorder schizophrenia 300 cases, 300 controls schizophrenia Stefanis et al, 2007 Caucasian, Indian, Native American, Asian, African, and mixed ethnicity Greek 113 nuclear families 168 cases 168 controls 2243 young male military conscripts Suliman et al, 2010 German schizophrenia Shinkai et al, 2007 schizotypy and cognitive endophenotypes 299 cases, 300 controls 531 cases 755 controls Vilella et al, 2007 Spanish schizophrenia 589 cases 617 controls Wirgeres et al, 2008 Norwegian 155 patients Wood et al, 2007 self-reported whites from various US regions PANSS in schizophrenia schizophrenia 345 schizophrenia cases 150 schizoaffective cases 352 controls rs2070586, rs2070587, rs2111902, rs10861974, rs3741775, rs3918347 MDAAO4, MDAAO5, MDAAO6 MDAAO4 MDAAO5 MDAAO6 rs3741775, rs3918346, rs2111902, rs3918347 n.s. 0.026 (allelic) 0.019 (allelic), 0.041 (genotypic) 0.021 (allelic) n.s. rs2111902 rs3918346 rs3741775 n.s. 0.033 (d´-S2B working memory) 0.048 (perceptual aberration scale CAPE, depression) rs987044, rs3916982, rs7136681, rs73410945, rs7980427, rs11114086, rs3825251, STR-1-dao2, STR2-dao3, SNP-3-exon11, rs10746135, rs7313861, rs3918305 rs11114071 rs4964766 rs2070586 rs73193464 rs2111902 rs3918346 rs3741775 rs4623951, rs11114086, rs2070587, hCV2880411, rs4964281 rs2070588, rs3741775 rs2070587 rs3741775, rs17041020, rs4623951 rs2070586 n.s. rs2111902 16 0.015 (adjusted p-value, PPI 85_30) 0.004 (adjusted p-value, PPI 85_60) 0.004 (adjusted p-value, pooled PPI 60 ms) n.s. 0.04 0.049 0.015 0.017 0.021 0.039 0.046 n.s. n.s. 0.036 (PANSS total score) n.s. 0.02159 (SCZ vs CON, allelic) 0.01219 (SCZ+SCA vs CON, allelic) 0.03973 (SCZ+SCA vs CON, genotypic) 0.00219 (SCZ vs CON, allelic) 0.00667 (SCZ vs CON, genotypic) 0.00056 (SCZ+SCA vs CON, allelic) 0.00192 (SCZ+SCA vs CON, genotypic) rs3918346 rs3825251 Yamada et al, 2005 Central Japan schizophrenia 50 cases 52 controls IVS1a+465G>C IVS1b+15G>A 570 cases 570 controls (sample set B) IVS1a+465G>C, IVS1b+15G>A, DAO-01, DAO-02, DAO-03, DAO-04, DAO-05 DAO-06 124 families Yang et al, 2013 Taiwan Han Chinese Table S2 Citations ratio of D-Serine to total Serine schizophrenia Sustained attention was assessed using the unmasked and masked CPTs (Zd´ and Zmd´) Four CPT strata 50 cases 52 controls 912 cases, 600 controls IVS1a+465G>C, IVS1b+15G>A, DAO-01, DAO02, DAO-03, DAO-04, DAO05, DAO-06 DAO-01, DAO-02, DAO-03, DAO-04, DAO-05, DAO-06 rs2070585, rs2070587 rs11114083 rs2070586 rs55944529 0.00068 (SCZ vs CON, allelic) 0.00297 (SCZ vs CON, genotypic) 0.00004 (SCZ + SCA vs CON, allelic) 0.00028 (SCZ + SCA vs CON, genotypic) 0.01800 (SCZ vs CON, allelic) 0.04340 (SCZ vs CON, genotypic) 0.00246 (SCZ+SCA vs CON, allelic) 0.00647(SCZ + SCA vs CON, genotypic) 0.038 (genotypic) 0.041 (allelic) 0.026 (genotypic) n.s. 0.020 (case-control, allelic) 0.023 (case-control, genotypic) n.s. n.s. n.s. 0.0357 (raw p-value, allele-based, Zmd´ >= -2.5) 0.0293 (raw p-value, trend-based, Zmd´>= -2.5) 0.0491 (raw p-value, genotype-based, Zd´>= -2.5) 0.0275 (raw p-value, allele-based, Zmd´ >= -2.5) 0.0252 (raw p-value, trend-based, Zmd´>= -2.5) 0.0459 (raw-p-value, genotype-based, overall) 0.0313 (raw p-value, allele-based, overall) 0.0299 (raw p-value, trend-based, overall) 0.0392 (raw p-value, allele-based, Zd´ < -2.5) 0.0365 (raw p-value, trend-based, Zd´ < -2.5) Bass NJ, Datta SR, McQuillin A, Puri V, Choudhury K, Thirumalai S, Lawrence J, Quested D, Pimm J, Curtis D, Gurling HM. Evidence for the association of the DAOA (G72) gene with schizophrenia and bipolar disorder but not for the association of the DAO gene with schizophrenia. Behav Brain Funct. 2009 Jul 8;5:28. Chumakov I, Blumenfeld M, Guerassimenko O, Cavarec L, Palicio M, Abderrahim H, Bougueleret L, Barry C, Tanaka H, La Rosa P, Puech A, Tahri N, Cohen-Akenine A, Delabrosse S, Lissarrague S, Picard FP, Maurice K, Essioux L, Millasseau P, Grel P, Debailleul V, Simon AM, Caterina D, Dufaure I, Malekzadeh K, Belova M, Luan JJ, Bouillot M, Sambucy JL, Primas G, Saumier M, Boubkiri N, Martin-Saumier S, Nasroune M, Peixoto H, Delaye A, Pinchot V, Bastucci M, Guillou S, Chevillon M, Sainz-Fuertes R, Meguenni S, Aurich-Costa J, Cherif D, Gimalac A, Van Duijn C, Gauvreau D, Ouellette G, Fortier I, Raelson J, Sherbatich T, Riazanskaia N, Rogaev E, Raeymaekers P, Aerssens J, Konings F, Luyten W, Macciardi F, Sham PC, Straub RE, Weinberger DR, Cohen N, Cohen D. Genetic and physiological data implicating the new human gene G72 and the gene for D-amino acid oxidase in schizophrenia. Proc Natl Acad Sci U S A. 2002 Oct 15;99(21):13675-80. Chung S, Jung J, Chung HY, Yoo HK, Kim CY, Joo YH, Choi SE, Hong JP. No association between polymorphisms of DAO and DAOA genes and homicidal behaviors in Korean schizophrenia. Psychiatr Genet. 2007 Oct;17(5):313. Corvin A, McGhee KA, Murphy K, Donohoe G, Nangle JM, Schwaiger S, Kenny N, Clarke S, Meagher D, Quinn J, Scully P, Baldwin P, Browne D, Walsh C, Waddington JL, Morris DW, Gill M. Evidence for association and epistasis at the DAOA/G30 and D-amino acid oxidase loci in an Irish schizophrenia sample. Am J Med Genet B Neuropsychiatr Genet. 2007 Oct 5;144B(7):949-53. Fallin MD, Lasseter VK, Avramopoulos D, Nicodemus KK, Wolyniec PS, McGrath JA, Steel G, Nestadt G, Liang KY, Huganir RL, Valle D, Pulver AE. Bipolar I disorder and schizophrenia: a 440single-nucleotide polymorphism screen of 64 candidate genes among Ashkenazi Jewish case-parent trios. Am J Hum Genet. 2005 Dec;77(6):918-36. Gaysina D, Cohen-Woods S, Chow PC, Martucci L, Schosser A, Ball HA, Tozzi F, Perry J, Muglia P, Kennedy JL, King N, Vincent JB, Parikh SV, Strauss J, Craig IW, McGuffin P, Farmer A. Association analysis of DAOA and DAO in bipolar disorder: results from two independent case-control studies. Bipolar Disord. 2010 Aug;12(5):579-81. 17 Jönsson EG, Saetre P, Vares M, Andreou D, Larsson K, Timm S, Rasmussen HB, Djurovic S, Melle I, Andreassen OA, Agartz I, Werge T, Hall H, Terenius L. DTNBP1, NRG1, DAOA, DAO and GRM3 polymorphisms and schizophrenia: an association study. Neuropsychobiology. 2009;59(3):142-50.Ohnuma T, Shibata N, Maeshima H, Baba H, Hatano T, Hanzawa R, Arai H. Association analysis of glycine- and serine-related genes in a Japanese population of patients with schizophrenia. Prog Neuropsychopharm Biol Psychiatry. 2009 Apr 30;33(3):511-8. Kim B, Kim H, Joo YH, Lim J, Kim CY, Song K. Sex-different association of DAO with schizophrenia in Koreans. Psychiatry Res. 2010 Sep 30;179(2):121-5. Liu X, He G, Wang X, Chen Q, Qian X, Lin W, Li D, Gu N, Feng G, He L. Association of DAAO with schizophrenia in the Chinese population. Neurosci Lett. 2004 Oct 21;369(3):228-33. Liu YL, Fann CS, Liu CM, Chang CC, Wu JY, Hung SI, Liu SK, Hsieh MH, Hwang TJ, Chan HY, Chen JJ, Faraone SV, Tsuang MT, Chen WJ, Hwu HG. No association of G72 and D-amino acid oxidase genes with schizophrenia. Schizophr Res. 2006 Oct;87(1-3):15-20. Ohnuma T, Shibata N, Baba H, Ohi K, Yasuda Y, Nakamura Y, Okochi T, Naitoh H, Hashimoto R, Iwata N, Ozaki N, Takeda M, Arai H. No association between DAO and schizophrenia in a Japanese patient population: a multicenter replication study. Schizophr Res. 2010 May;118(1-3):300-2. Ohnuma T, Shibata N, Maeshima H, Baba H, Hatano T, Hanzawa R, Arai H. Association analysis of glycine- and serine-related genes in a Japanese population of patients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2009 Apr 30;33(3):511-8. Papagni SA, Mechelli A, Prata DP, Kambeitz J, Fu CH, Picchioni M, Walshe M, Toulopoulou T, Bramon E, Murray RM, Collier DA, Bellomo A, McGuire P. Differential effects of DAAO on regional activation and functional connectivity in schizophrenia, bipolar disorder and controls. Neuroimage. 2011 Jun 15;56(4):2283-91. Prata D, Breen G, Osborne S, Munro J, St Clair D, Collier D. Association of DAO and G72(DAOA)/G30 genes with bipolar affective disorder. Am J Med Genet B Neuropsychiatr Genet. 2008 Sep 5;147B(6):914-7.Corvin A, Donohoe G, McGhee K, Murphy K, Kenny N, Schwaiger S, Nangle JM, Morris D, Gill M. D-amino acid oxidase (DAO) genotype and mood symptomatology in schizophrenia. Neurosci Lett. 2007 Oct 16;426(2):97-100. Roussos P, Giakoumaki SG, Adamaki E, Georgakopoulos A, Robakis NK, Bitsios P. The association of schizophrenia risk D-amino acid oxidase polymorphisms with sensorimotor gating, working memory and personality in healthy males. Neuropsychopharmacology. 2011 Jul;36(8):1677-88. Sacchetti E, Scassellati C, Minelli A, Valsecchi P, Bonvicini C, Pasqualetti P, Galluzzo A, Pioli R, Gennarelli M. Schizophrenia susceptibility and NMDA-receptor mediated signalling: an association study involving 32 tagSNPs of DAO, DAOA, PPP3CC, and DTNBP1 genes. BMC Med Genet. 2013 Mar 9;14:33. Schumacher J, Jamra RA, Freudenberg J, Becker T, Ohlraun S, Otte AC, Tullius M, Kovalenko S, Bogaert AV, Maier W, Rietschel M, Propping P, Nöthen MM, Cichon S. Examination of G72 and D-amino-acid oxidase as genetic risk factors for schizophrenia and bipolar affective disorder. Mol Psychiatry. 2004 Feb;9(2):203-7. Schumacher J, Abou Jamra R, Becker T, Klopp N, Franke P, Jacob C, Sand P, Fritze J, Ohlraun S, Schulze TG, Rietschel M, Illig T, Propping P, Cichon S, Deckert J, Nöthen MM. Investigation of the DAOA/G30 locus in panic disorder. Mol Psychiatry. 2005 May;10(5):428-9. Shinkai T, De Luca V, Hwang R, Müller DJ, Lanktree M, Zai G, Shaikh S, Wong G, Sicard T, Potapova N, Trakalo J, King N, Matsumoto C, Hori H, Wong AH, Ohmori O, Macciardi F, Nakamura J, Kennedy JL. Association analyses of the DAOA/G30 and D-amino-acid oxidase genes in schizophrenia: further evidence for a role in schizophrenia. Neuromolecular Med. 2007;9(2):169-77. Stefanis NC, Trikalinos TA, Avramopoulos D, Smyrnis N, Evdokimidis I, Ntzani EE, Ioannidis JP, Stefanis CN. Impact of schizophrenia candidate genes on schizotypy and cognitive endophenotypes at the population level. Biol Psychiatry. 2007 Oct 1;62(7):784-92. Suliman H, Schumacher J, Becker T, Cichon S, Schulze TG, Propping P, Rietschel M, Nöthen MM, Jamra RA. Association study of 20 genetic variants at the (D)-amino acid oxidase gene in schizophrenia. Psychiatr Genet. 2010 Apr;20(2):82-3. Vilella E, Costas J, Sanjuan J, Guitart M, De Diego Y, Carracedo A, Martorell L, Valero J, Labad A, De Frutos R, Nájera C, Moltó MD, Toirac I, Guillamat R, Brunet A, Vallès V, Pérez L, Leon M, de Fonseca FR, Phillips C, Torres M. Association of schizophrenia with DTNBP1 but not with DAO, DAOA, NRG1 and RGS4 nor their genetic interaction. J Psychiatr Res. 2008 Mar;42(4):278-88. Wirgenes KV, Djurovic S, Agartz I, Jonsson EG, Werge T, Melle I, Andreassen OA. Dysbindin and d-amino-acid-oxidase gene polymorphisms associated with positive and negative symptoms in schizophrenia. Neuropsychobiology.2009;60(1):31-6. Wood LS, Pickering EH, Dechairo BM. Significant support for DAO as a schizophrenia susceptibility locus: examination of five genes putativelyassociated with schizophrenia. Biol Psychiatry. 2007 May 15;61(10):1195-9. Yamada K, Ohnishi T, Hashimoto K, Ohba H, Iwayama-Shigeno Y, Toyoshima M, Okuno A, Takao H, Toyota T, Minabe Y, Nakamura K, Shimizu E, Itokawa M, Mori N, Iyo M, Yoshikawa T. Identification of multiple serine racemase (SRR) mRNA isoforms and genetic analyses of SRR and DAO in schizophrenia and D-serine levels. Biol Psychiatry. 2005 Jun 15;57(12):1493503. Yang HC, Liu CM, Liu YL, Chen CW, Chang CC, Fann CS, Chiou JJ, Yang UC, Chen CH, Faraone SV, Tsuang MT, Hwu HG. The DAO gene is associated with schizophrenia and interacts with other genes in the Taiwan Han Chinese population. PLoS One. 2013;8(3):e60099. 18 Table S4. Candidate gene studies of DAOA Paper Addington et al, 2004 Andreou et al, 2012 Bakker et al, 2007 Bass et al, 2009 Ancestry mixed Caucasian patients had at least three Dutch-born Caucasian grandparents three of the grandparents were of English, Irish, Welsh, or Scottish descent Phenotype childhood-onset schizophrenia and psychosis NOS Sample size 98 children and adolescents 5-HIAA, HVA, and MHPG concentration in cerebrospinal fluid in healthy individuals 132 individuals deficit and non-deficit schizophrenia 308 cases 580 controls schizophrenia 431 cases 442 controls bipolar disorder 303 cases 442 controls 734 cases 442 controls 225 individuals 301 cases 604 controls 139 cases (116 ´enriched cases´ (linkage to 13q33), 113 controls Bousman et al, 2013 Australian schizophrenia and bipolar disorder combined transition to psychosis in individuals at ultra-high risk for psychosis Carrera et al, 2010 Spanish Caucasian origin schizophrenia Chen et al, 2004 US birth, self-reported as ´white´ bipolar affective disorder Chen et al, 2013 Chinese schizophrenia 454 cases 480 controls Chen et al, 2012 Chinese resting-state brain activity in major depression 488 cases 480 controls Chiesa et al, 2011 Korean Chiesa et al, 2012 Korean Chumakov et al, 2002 Canadian, Russian schizophrenia, treatment outcomes major depressive disorder (MDD), bipolar disorder (BD) 221 cases 145 cases (MDD) 132 cases (BD) 170 controls 213 (Canadian cases) 241 (Canadian controls) 183 (Russian cases) 183 (Russian controls) 19 Variant rs746187, rs3916964, rs778294, rs778293, rs1935062, rs1935058 rs2391191 rs3916967 rs2391191, rs778294 P-value (OR) n.s. rs3918342 0.03 (5-HIAA) 0.001 (HVA) 0.004 (HVA) n.s. rs1421292 rs3918342, rs2391191, rs3916967, rs1421292 rs3916965, rs3916967, rs2391191, rs947267, rs778294, rs778293, rs1421292 rs3918342 rs2391191, rs947267, rs778294, rs1421292, rs1341402, rs1935062, rs954581 rs3918342 rs3918342 rs1421292 rs7320588, rs6416389, rs1935057, rs1341402, rs2391191, rs1539070, rs1935062, rs6491961, rs7986339, rs2153674, rs7989006, rs7984976, rs947267, rs778294, rs778293, rs3918342 rs9586843, rs7329966, rs7324448, rs1575633, rs1570709 rs1935058, rs2391191, rs954581 rs1935062 rs947267 rs3916965, rs3916966, rs3916967, rs2391191, rs3918341, rs9558562, rs947267, rs778294, rs3918342, rs1421292 rs3916965, rs3916966, rs3916967, rs9558562, rs947267, rs3918342, rs1421292 rs2391191 rs3918341 rs778294 rs3916966, rs3916967, rs2391191, rs3916968, rs778293 rs7139958 rs9558571 rs3916966, rs3916967, rs2391191, rs3916968, rs7139958, rs9558571, rs778293 DAOA_M06 (SNP), rs746187 (M07), DAOA_M08 (SNP), DAOA_M09 (SNP), DAOA_M10 (SNP), rs3916964 (M11), rs3916966 (M13), rs3918341 (M16), DAOA_M17 (SNP), rs947267 (M18), rs778294 (M19), rs3916971 (M21), rs3916970 (M20) rs3918342 (M23) 0.031 0.015 n.s. n.s. 0.016 n.s. 0.038 0.008 0.044 n.s. n.s. n.s. 0.0072 (OR 1.67) 0.0048 (enriched, OR 1.77) 0.0403 (all cases, OR 0.69) 0.0295 (enriched cases, OR 0.66) n.s. n.s. 0.01 (allelic OR 1.27) 0.04 (OR 1.09) 0.02 (1.37) n.s. 0.005 PANSS positive at baseline) 0.008 (allelic, PANSS at baseline) n.s. n.s. 0.019 (allelic, Canadian) rs2391191 (M15) rs778293 (M22) rs3916967 (M14) rs3916965 (M12) rs1421292 (M24) Chung et al, 2007 Korean Corvin et al, 2007 Irish Corvin et al, 2007 Irish origin, i.e., Irish parents / grandparents Dalvie et al, 2010 mixed ancestry, Caucasian Detera-Wadleigh et al, 2006 various ethnicities homicidal behaviors in schizophrenia depression/anxiety factor in schizophrenia schizophrenia 188 cases bipolar 1: age at onset, # depressive episodes, # hospitalizations for depression schizophrenia and bipolar disorder 191 cases schizophrenia bipolar disorder 196 schizophrenia, 59 schizoaffective 373 cases, 812 controls meta-analysis meta-analysis meta-analysis Di Maria et al, 2009 Italian descent psychosis 185 Alzheimer´s disease Donohoe et al, 2007 Irish episodic memory 93 cases Fallin et al, 2005 Ashkenazi schizophrenia / schizoaffective disorder 274 trios rs3918341, rs9301030, rs3916968, rs947267, rs701567, rs778294 rs3918346 0.01 rs778293, rs3918342, rs1421292 rs2391191 rs3916965 rs701567 n.s. 0.01 (corrected p-value, OR 1.31) 0.005 (corrected p-value, OR 1.34) n.s. rs746187, rs3916964, rs1341402, rs3916967, rs3918341, rs947267, rs778294, rs954581, rs3916970, rs3916971 rs3916965 rs3916966 rs1935058 rs2391191 rs1935062 rs778293 rs3918342 rs1421292 rs746187, rs3916964, rs3916966, rs1935058, rs1341402, rs3916967, rs3918341, rs1935062, rs947267, rs778294, rs954581, rs3916970, rs3916971 rs3916965 rs2391191 rs778293 rs3918342 rs1421292 rs746187, rs3916964, rs3916965, rs3916966, rs1935058, rs1341402, rs3916967, rs2391191, rs3918341, rs947267, rs778294, rs954581, rs3916970, rs3916971, rs778293, rs1421292 rs1935062 rs3918342 rs1341402, rs1341403, rs6491961, rs9558571, rs778294, rs12864685 rs2153674 rs2391191 n.s. rs2391191, rs947267, rs778294, rs3916970, rs3916968, rs1935062, rs954580, rs2893229, rs1341406, rs1341402, rs701567, DAOA_GCintronic, DAOA_3'UTR873, 20 0.017 (allelic, Russian) 0.032 (allelic, Canadian) 0.003 (allelic, Canadian) 0.007 (genotypic, Canadian) 0.038 (allelic, Canadian) 0.007 (allelic, Canadian) 0.020 (genotypic, Canadian) 0.019 (allelic, Canadian) 0.044 (genotypic, Canadian) 0.006 (genotypic, Russian) n.s. 0.0001 0.0413 0.0015 0.0000 0.0143 0.0003 0.0000 0.0010 n.s. 0.0002 0.0006 0.0033 0.0006 0.0092 n.s. 0.0019 0.0309 n.s. 0.033 0.028 (immediate recall) 0.015 (delayed recall) gene is suggestive (any SNP or haplotype minimal p value 0.01<p<0.05) DAOA_3'UTR1746 Gawlik et al, 2010 Gaysina et al, 2010 Goldberg et al, 2006 Gomez et al, 2008 Grigoroiu-Serbanescu et al, 2010 Hall et al, 2004 Hall et al, 2008 Hattori et al, 2003 bipolar I disorder 337 trios 14 SNPs German Caucasian descent UK, Canada affective psychosis Americans of European extraction (Caucasian according to self report) schizophrenia, cognitive variables 248 cases 188 controls 515 cases (UK) 1316 controls (UK) 385 cases (Canada) 312 controls (Canada) up to 106 trios >600 subjects (cognitive function) 14 normal individuals (fMRI) 30 normal individuals (fMRI) rs3916966, rs1935058, rs2391191, rs1935062, rs947267, rs3918342, rs9558575 rs3916965, rs12584489, rs2391191, rs1935062, rs947267, rs778292, rs3918342, rs1421292 rs9558562 M01, M02, M03, rs2391191 (M04), rs1935058 (M05), rs1935062 (M06), rs778294 (M07), M08, M09, M10, M11 M10 646 nuclear families rs1341402, rs12874006, rs1539070, rs9284226, rs2153674, rs9558567, rs947267, rs3918342 rs2391191 rs3918341 rs1935062 rs3916965, rs1935057, rs1341402, rs3916967, rs2391191, rs1935062, rs67705083, rs778294, rs954581, rs3916971, rs778293, G72_z6:1117, rs3918342, rs1421292 rs778293 rs3916965 rs1935057 rs3916967 rs2391191 M7, M12, M14, M23, M25 M15 rs3918342, rs1421292 Hungarian Romanian South African Afrikaner, USA Scottish bipolar disorder juvenile onset mood disorders bipolar I global diagnosis, psychotic bipolar I subtype 198 cases 180 controls bipolar I with delusions bipolar I in non-psychotic 123 cases 38 cases schizophrenia 169 South African trios 210 USA trios 61 individuals hippocampal function in subjects at high risk of schizophrenia bipolar disorder 22 multiplex families 21 rs1998654, rs2181953, rs978714, rs1359387, M-13, rs2391191, rs947267, rs954581, rs778334, rs2012887, M-23 rs1815686 rs1935058 rs1341402 rs1935062 rs778294 suggestive (any SNP or haplotype minimal p value 0.01<p<0.05) n.s. n.s. 0.05 (UK sample) n.s. 0.03 (genotypic, continuous performance test) 0.04 (genotypic, n-back [one back] working memory test) 0.05 (genotypic, verbal paired associate learning) fMRI: strong effect on BOLD activation in hippocampus during episodic memory paradigm n.s. 0.025 0.029 0.026 n.s. 0.042 (dominant model) 0.044 (OR 1.82) 0.037 (OR 1.88) 0.043 (OR 1.82) 0.043 (OR 1.82) n.s. 0.045 (S African trios; n.s. US trios differences in the activation of the left hippocampus and parahippocampus in the contrast of sentence completion versus rest, and in recruitment of right inferior prefrontal cortex in relation to increasing task difficulty n.s. 0.041 0.00077 0.0075 0.0078 0.018 Hong et al, 2006 Hukic et al, 2013 Chinese Swedish schizophrenia cognitive manic symptoms (CMS) in bipolar I disorder 152 families (NIMH pedigrees) 216 families 488 cases 1044 controls rs1935058, rs1341402, rs2391191, rs1935062, rs947267, rs778294, rs954581 rs947267 rs3916967 rs2391191 Jansen et al, 2009 European descent cognitive functions 423 healthy individuals rs1935062 rs3918342 rs1421292 Jansen et al, 2010 Jönsson et al, 2009 European descent Danish, Norwegian, Swedish memory encoding, retrieval schizophrenia Korostishevsky et al, 2004 Ashkenazi schizophrenia Korostishevsky et al, 2006 Kotaka et al, 2009 Palestinian Arab Japanese Krug et al, 2011 western- or middle European descent Li et al, 2007 various ethnicities schizophrenia methamphetamine induced psychosis brain activation in right middle temporal gyrus during verbal fluency task schizophrenia (meta-analysis) 83 healthy subjects 420 cases (DK), 1004 controls (DK), 162 cases (Norway), 177 controls (Norway), 255 cases (Sweden), 292 controls (Sweden) 60 cases 130 controls 56 families from northern Israel 136 families from central Israel 31 families from southern Israel 209 cases 291 controls rs3918342, rs1421292 rs2391191, rs778294, rs3918342, M9924634108M24 rs3916965, rs3916967, rs2391191, rs3918341, rs947267, rs778294, rs3916970 rs3918342 rs778293 rs3916971 rs3916966 rs3916965, rs3916966, rs3916967, rs2391191, rs3918341, rs947267, rs778294 , rs3916971, rs778293, rs3918342 rs3916970 rs3916965, rs2391191, rs947267, rs3918342, rs1421292 rs778293 96 healthy individuals rs3918342, rs1421292 2138 cases, 2228 controls, 463 parentoffspring trios rs3916966, rs3916967, rs3918341, rs947267, rs778294, rs3916970, rs3916971, rs778293, rs1935062 rs3916965 rs2391191 rs3918342 rs1421292 rs3916965, rs3916966, rs3916967, rs2391191, rs947267, rs778294, rs3916970, rs3916971, rs778293, rs3918342, rs3916968 rs3916965, rs3916967, rs2391191 rs778294 rs3918342 rs778293 Liu et al, 2006 Taiwanese schizophrenia 218 families Ma et al, 2006 Han Chinese, Scottish schizophrenia 588 (Han Chinese cases) 588 (Han Chinese controls) 183 (Scottish cases) 182 (Scottish controls) 22 n.s. 0.016 0.018 (CMS vs. Non-CMS) 0.026 (CMS vs controls) 0.039 (CMS vs. Non-CMS) 0.019 (CMS vs controls) n.s. 0.002 (letter-number-span test) 0.001 (d2-test for attention) 0.001 (letter-number-span test) 0.001 (d2-test for attention) n.s. n.s. n.s. 0.001 (genotypic) 0.001 (allelic) 0.005 (genotypic) 0.04 (genotypic) 0.04 (genotypic) n.s. 0.018 (haplotype relative risk, northern Israel) 0.014 (transmission disequilibrium test, northern Israel) n.s. 0.0015 (allelic) 0.00016 (genotypic) rs1421292 positively correlated with brain activation in right middle temporal gyrus and right procuneus n.s. 0.0225 (OR 1.12) 0.0086 (OR 1.15) 0.0136 (OR 0.88) 0.0010 (OR 0.8) n.s. n.s. 0.025 (OR 0.69, Scottish sample) 0.0005 (OR 0.60, Scottish) 0.022 (OR 0.71, Scottish) 0.0013 (OR 0.76, Han Chinese) Ma et al, 2009 Chinese Maheshwari et al, 2009 Caucasian 126 family trios bipolar disorder 19 families with 146 samples from Statistical Explanation for Positional Cloning (STEPC) analysis 376 bipolar parentproband trios 555 cases, 564 controls Mössner et al, 2010 Mulle et al, 2005 Müller et al, 2011 German samples from NIMH Genetics Initiative and the Western Psychiatric Institute and Clinic at the University of Pittsburgh Canadian progression of prodromal syndromes to first episode psychosis 82 probands schizophrenia 159 trios rs778294 rs3918342 rs778293 rs1935058 rs1341402 rs9301030 rs1815686 rs12862108 rs1935062 rs778294 rs778326 rs978714, rs2025522, rs3916964, rs9558551, rs7981258, rs9301029, rs1253464, rs3916965, rs9519671, rs3916966, rs1935057, rs1935058, ss107796322, rs1341402, rs2391191, ss107796323, ss107796324, rs12862108, rs9301030, rs1935062, rs9519683, ss104807115, rs7986339, rs947267, rs701567, rs778294, rs7987770, ss107796325, rs9558581, rs778326, rs954581, rs9301034, rs778336, rs778334, rs778293, rs2012887, rs3918342, rs1421292 variants identified by sequencing DAOA exons: ss104807091, ss104807092, ss104807093, ss104807094, ss104807095, ss104807096, ss104807097, ss104807098, ss104807099, ss104807100, ss104807101, ss104807102, ss104807103, rs2391191, ss104807104, ss104807105, ss104807106, ss104807107, rs9558562, ss104807108, ss104807109, ss104807110, ss104807111, ss104807112, ss104807113, rs9519683, ss104807114, ss104807115, ss104807116, ss104807117, ss104807118, rs9582999, ss104807119, ss104807120, rs9670704, ss104807121, ss104807122, ss104807123, rs778294, ss104807124, ss104807125, ss104807126, ss104807127, ss104807128, ss104807129, ss104807130, ss104807131, rs9558573, ss104807132, ss104807133, ss104807134, ss104807135, ss104807136 rs1935058, rs2391191, rs1935062, rs947267, rs778293, rs3918342, rs1421292 rs1341402 rs778294 M-1, M-2, M-3, M-5, M-11, M-12, M-13, M-14, M-15, M-16, M-21, M-22, M-23, M-24 M-4 n.s. 0.02 (all) (all), 0.041 (male) 0.0009 0.0083 0.031 0.039 0.020 0.0074 0.017 0.026 n.s. No significant excess of rare variants in cases compared to controls n.s. 0.002 0.030 n.s. 0.04 bipolar disorder 303 core families rs1341402, rs2391191, rs947267, rs778294 rs1935062 n.s. 0.02 (total sample) bipolar disorder with psychotic symptoms 157 families rs1935062 0.01 (European sample) n.s. 23 Ohi et al, 2009 Pae et al, 2010 Prata et al, 2008 Prata et al, 2012 Rethelyi et al, 2009 Rietschel et al, 2008 Japanese Korean bipolar disorder meta-analysis schizophrenia meta-analysis schizophrenia antipsychotic response after switch to aripiprazole 1774 (cases) 2092 (controls) 86 patients rs1341402, rs2391191, rs1935062, rs947267, rs778294 rs1341402, rs2391191, rs1935062, rs947267, rs778294 rs2391191 rs3916965, rs3916967, rs2391191, rs778294, rs3916970 rs778293 rs947267 rs3918342 rs746187, rs3916966, rs2391191, rs3916972 brain function during verbal fluency 50 healthy volunteers rs746187 Hungarian Caucasian descent German schizophrenia 280 cases, 230 controls 500 major depression patients, 1030 controls rs2391191, rs3918342 schizophrenia 391 patients, 488 controls Sanders et al, 2008 European ancestry schizophrenia 1870 cases 2002 controls Schulz et al, 2011 Caucasian Schulze et al, 2005 German, Polish reduced cortical thickness in schizophrenia bipolar disorder 52 patients, 42 controls 300 patients (German), 300 controls (German), 294 patients (Polish), 24 0.019 (allelic) 0.005 (Schedule for the Assessment of Negative Symptoms [SANS] score) 0.02 (Brief Psychiatric Rating Scale [BPRS] score) n.s. n.s. 213 bipolar I cases, 197 controls Italian 0.03 (fixed effects model, East Asians) n.s. 0.034 (genotypic) 0.030 (allelic) 0.037 (allelic) 0.02 (Brief Psychiatric Rating Scale [BPRS] score) bipolar disorder Saccetti et al, 2013 n.s. rs3918342 rs1421292 rs2391191 Caucasian with at least 3 of 4 grandparents born in Scotland English native speakers major depression, neuroticism n.s. Significant effect on activation in the left postcentral and supramarginal gyri (FWE p<0.05) n.s. rs3916965, rs1935058, rs1341402, rs3916967, rs2391191, rs1935062, DAO_3UTR_SNP12, rs3916971, rs3918342, rs1421292 rs778293 G72_z6:1117 n.s. rs1341402, rs1341403, rs6491961, rs9558571, rs778294 rs12864685 rs778294, rs3918342, rs2391191, rs778293, rs3916968, rs3916967, rs3916966, rs3916965, rs1421292, rs701567, rs778334, rs17713906, rs10492528, rs12864685, rs12874006, rs1935060, rs2039934, rs7139958, rs8002132, rs9284226, rs9301030, rs9555175, rs9558573, rs9670704, rs1361562, G72GD486 (SNP), G72RS425 (SNP)(SNP rs identifiers from SZ gene database) rs1539070 rs1557072 rs2391191 n.s. rs1341402, rs2391191 rs3918342 rs3918342 rs3918342 0.02 (major depression) 0.04 (major depression) 0.05 (recessive model) n.s. 0.05 (OR 1.13) 0.02 (OR 1.84) associated with distinct cortical thinning n.s. <0.02 (bipolar disorder) 0.005 (bipolar with psychosis) <0.0004 (bipolar with delusions) Schumacher et al, 2004 Caucasian schizophrenia bipolar disorder Schumacher et al, 2005 German descent panic disorder 311 controls (Polish) 299 cases 300 controls 300 cases 300 controls 152 cases, 208 controls Seifuddin et al, 2012 various ethnicities bipolar disorder meta-analysis Shi et al, 2009 Han Chinese schizophrenia 561 families Shi et al, 2008 various ethnicities schizophrenia 4304 cases, 5423 controls, 1384 families (Meta-analysis) rs1421292 rs1341402, rs1935062, rs778294 M23 rs2391191 M12 M24 M12, rs1341402, rs2391191, rs1935062, rs778294, M24 M23 rs2391191, rs3916972 rs421292 rs778293 rs3918342 rs1421292, rs2391191, rs778294 rs3918342 rs947267 rs778293 rs3916965, rs3916966, rs1935058, rs1341402, rs3916967, rs2391191, rs3918341, rs1935062, rs778294, rs3916970, rs3916971, rs778293, rs3918342, rs1421292 rs947267 rs778293 rs1421292 bipolar disorder Shin et al, 2007 Korean schizophrenia Shinkai et al, 2007 Canadian population, various ethnicities schizophrenia Soronen et al, 2008 Finnish visuospatial ability in bipolar disorder 1145 cases, 1829 controls, 174 families 388 patients, 367 controls 113 nuclear families, 168 cases, 168 controls 180 families rs2391191, rs778294, rs1341402, rs1935058, rs1935062 rs947267 rs778294 rs3916965, rs3916966, rs3916967, rs2391191, rs3918341, rs3916970 rs3916971 rs947267, rs2391191, rs778293, rs3916967 , rs3916965, rs1421292, rs3916972 rs746187 rs3918342 rs3916966 rs2391191 25 <0.007 (bipolar delusions) n.s. 0.033 (allelic), (OR 1.28) 0.037 (allelic), (OR 1.28) 0.048 (allelic), (OR 1.25) 0.036 (allelic), (OR 1.27) n.s. 0.013 (allelic, OR 1.33) 0.025 (genotypic, OR 1.68) n.s. 0.024 (OR 2.12, dominant) 0.031 (OR 1.39, allelic model) 0.049 (OR 1.35, allelic model) 0.047 (OR 1.35, allelic model) n.s. 0.05 (OR 1.14) n.s. 0.0012 n.s. 0.03 (OR 0.87, all), 5.62E-6 (OR 0.71, Asians) 0.0002 (OR 0.81, Asians) 0.027 (OR 1.11, all ethnicities) 0.031 (OR 1.12, Europeans) n.s. 0.008 0.009 n.s. 0.03 n.s. 0.013 (OR 0.67, case-control) 0.029 (transmission disequilibrium test) 0.0015 (General ability) 0.0010 (Abstraction) 0.0013 (Psychomotor speed) 4.00E-06 (Visuospatial ability) 0.0091 (Auditory attention) 0.0298 (Verbal working memory) 0.0047 (Immediate visual memory) 0.0005 (Delayed visual memory) 0.0032 (Free short delay recall) 0.0443 (Free long delay recall) 0.0173 (Recognition memory) 0.0162 (Stroop Interference score) 0.0195 (Semantic fluency) 0.0002 (General ability) 0.0003 (Abstraction) Soronen et al, 2011 Finnish Mood disorder (MOOD), bipolar disorder, major depressive disorder (MDD), anxiety, alcoholism, psychotic symptoms, suicide attempts, more time ill 178 bipolar I and II patients, 272 major depressive disorder patients, 1322 controls rs2391191 rs778336 Stefanis et al, 2007 Greek 2243 male conscripts rs2391191, rs778293, rs3918342 Tan et al, 2014 Caucasian, Asian n.s. Spanish white persons from the United Kingdom rs746187, rs3916967, rs2391191, rs947267, rs778293, rs1421292, rs2181953 rs3916965, rs2391191, rs778294, rs778293, rs1421292, rs1935058, rs1341402, rs954581, DAOA_3'UTR_SNP12 rs2391191, rs778294, rs778293, rs1421292, rs1935058, rs954581, rs391695 rs1341402 DAOA_3'UTR_SNP12 rs3916967, rs778293, rs3918342, rs1935062 rs2391191 n.s. Williams et al, 2006 17515 cases, 25189 controls 589 cases 617 controls 709 cases 1416 controls rs2391191, rs947267, rs3918342 Vilella et al, 2007 schizotypy and cognitive endophenotypes schizophrenia, bipolar disorder, depressive disorder schizophrenia 0.0034 (Psychomotor speed) 5.00E-06 (Visuospatial ability) 0.0088 (Auditory attention) 0.0213 (Verbal working memory) 0.0047 (Immediate visual memory) 0.0010 (Delayed visual memory) 0.0024 (Free short delay recall) 0.0206 (Free long delay recall) 0.0079 (Recognition memory) 0.0060 (Stroop Interference score) 0.0239 (Semantic fluency) 0.0086 (General ability) 0.0063 (Abstraction) 0.0369 (Phonemic fluency) 0.0083 (General ability) 0.0173 (Abstraction) 0.0125 (Psychomotor speed) 0.0108 (Visuospatial ability) 0.0047 (Stroop Interference score) 0.0168 (Semantic fluency) 0.0051 (General ability) 0.0392 (Visuospatial ability) 0.0465 (MOOD, all) 0.0310 (MOOD, all) 0.0209 (MOOD, positive FHx) 0.0406 (MDD, all) 0.0407 (MDD, positive FHx) 0.0447 (anxiety) 0.0114 (time ill) n.s. rs2153674 rs701567 rs954580 schizophrenia bipolar I disorder Wang et al, 2004 Han Chinese schizophrenia 706 cases 1416 controls 537 cases 538 controls rs3916965 Wood et al, 2007 self-reported whites from various US regions schizophrenia 345 schizophrenia cases, 150 schizoaffective cases, 352 controls Yang et al, 2013 Taiwan´s Han Chinese Population schizophrenia 912 cases, 600 controls 26 rs2391191, rs947267, rs3918342, rs1935062, rs1935058, rs954580, rs1341402, rs9301036, rs9301035, rs778336, rs778334, rs778332, rs778331, rs778330, rs17713906, rs1642681, rs1341401, rs11618600, rs10492527 rs3916966, rs45476401, rs113692101, rs2391191, rs778294, rs9558573 n.s. n.s. 0.047 0.03 0.01 n.s. 0.0010 (OR 1.33, all) 0.020 (OR 1.33, males) 0.021, OR 1.34, females) 0.019 (OR 1.23, all) 0.045 (OR 1.29, females) n.s. n.s. Yue et al, 2006 Chinese Han descendants schizophrenia (SZ), early onset schizophrenia (EOS), male schizophrenia Yue et al, 2007 Han Chinese schizophrenia (SZ), clinical symptoms Zhang et al, 2009 Chinese Han bipolar disorder Zuliani et al, 2009 UK population bipolar disorder, temporal lobe and amygdala structure Zou et al, 2005 Han Chinese 216 cases, 321 controls (SZ), 88 cases, 131 controls (EOS), 120 cases, 184 controls (men) 359 cases 359 controls 237 trios 475 cases, 588 controls 38 cases, 81 controls 233 trios rs2391191, rs778294 n.s. rs947267 0.006 (OR 1.43, SZ) 0.012 (OR 1.67, EOS) 0.034 (OR 1.45, males) n.s. 0.004 (OR 1.38) 0.019 (, trios) n.s. 0.047 (OR 0.77) 0.003 (OR 1.33) rs1421292: decreased gray matter density left temporal pole in bipolar disorder. rs3918342: reductions in right amygdala gray matter density n.s. 0.0108 0.0018 rs2391191, rs778294, rs3918342 rs947267 rs3916965, rs2391191, rs3918342 rs778294 rs778293 rs1421292, rs3918342 rs3916967 rs2391191 rs3916965 Addington AM, Gornick M, Sporn AL, Gogtay N, Greenstein D, Lenane M, Gochman P, Baker N, Balkissoon R, Vakkalanka RK, Weinberger DR, Straub RE, Rapoport JL. Polymorphisms in the 13q33.2 gene G72/G30 are associated with childhood-onset schizophrenia and psychosis not otherwise specified. Biol Psychiatry. 2004 May 15;55(10):976-80. Andreou D, Saetre P, Werge T, Andreassen OA, Agartz I, Sedvall GC, Hall H, Terenius L, Jönsson EG. D-amino acid oxidase activator gene (DAOA) variation affects cerebrospinal fluid homovanillic acid concentrations in healthy Caucasians. Eur Arch Psychiatry Clin Neurosci. 2012 Oct;262(7):549-56. Bakker SC, Hoogendoorn ML, Hendriks J, Verzijlbergen K, Caron S, Verduijn W, Selten JP, Pearson PL, Kahn RS, Sinke RJ. The PIP5K2A and RGS4 genes are differentially associated with deficit and non-deficit schizophrenia. Genes Brain Behav. 2007 Mar;6(2):113-9. Bass NJ, Datta SR, McQuillin A, Puri V, Choudhury K, Thirumalai S, Lawrence J, Quested D, Pimm J, Curtis D, Gurling HM. Evidence for the association of the DAOA (G72) gene with schizophrenia and bipolar disorder but not for the association of the DAO gene with schizophrenia. Behav Brain Funct. 2009 Jul 8;5:28. Bousman CA, Yung AR, Pantelis C, Ellis JA, Chavez RA, Nelson B, Lin A, Wood SJ, Amminger GP, Velakoulis D, McGorry PD, Everall IP, Foley DL. Effects of NRG1 and DAOA genetic variation on transition to psychosis in individuals at ultra-high risk for psychosis. Transl Psychiatry. 2013 Apr 30;3:e251. Carrera N, Arrojo M, Paz E, Ramos-Ríos R, Agra S, Páramo M, Brenlla J, Costas J. Testing the antagonistic pleiotropy model of schizophrenia susceptibility by analysis of DAOA, PPP1R1B, and APOL1 genes. Psychiatry Res. 2010 Sep 30;179(2):126-9. Chen J, Xu Y, Zhang J, Liu Z, Xu C, Zhang K, Shen Y, Xu Q. Genotypic association of the DAOA gene with resting-state brain activity in major depression. Mol Neurobiol. 2012 Oct;46(2):36173. Chen J, Xu Y, Zhang J, Liu Z, Xu C, Zhang K, Shen Y, Xu Q. A combined study of genetic association and brain imaging on the DAOA gene in schizophrenia. Am J Med Genet B Neuropsychiatr Genet. 2013 Mar;162B(2):191-200. Chen YS, Akula N, Detera-Wadleigh SD, Schulze TG, Thomas J, Potash JB, DePaulo JR, McInnis MG, Cox NJ, McMahon FJ. Findings in an independent sample support an association between bipolar affective disorder and the G72/G30 locus on chromosome 13q33. Mol Psychiatry. 2004 Jan;9(1):87-92. Chiesa A, Pae CU, Porcelli S, Han C, Lee SJ, Patkar AA, Park MH, Serretti A. DAOA variants and schizophrenia: influence on diagnosis and treatment outcomes. Int J Psychiatry Clin Pract. 2011 Nov;15(4):303-10. Chiesa A, Pae CU, Porcelli S, Han C, Lee SJ, Patkar AA, Park MH, Jun TY, Serretti A. DAOA variants on diagnosis and response to treatment in patients with major depressive disorder and bipolar disorder. J Int Med Res. 2012;40(1):258-65. Chumakov I, Blumenfeld M, Guerassimenko O, Cavarec L, Palicio M, Abderrahim H, Bougueleret L, Barry C, Tanaka H, La Rosa P, Puech A, Tahri N, Cohen-Akenine A, Delabrosse S, Lissarrague S, Picard FP, Maurice K, Essioux L, Millasseau P, Grel P, Debailleul V, Simon AM, Caterina D, Dufaure I, Malekzadeh K, Belova M, Luan JJ, Bouillot M, Sambucy JL, Primas G, Saumier M, Boubkiri N, Martin-Saumier S, Nasroune M, Peixoto H, Delaye A, Pinchot V, Bastucci M, Guillou S, Chevillon M, Sainz-Fuertes R, Meguenni S, Aurich-Costa J, Cherif D, Gimalac A, Van Duijn C, Gauvreau D, Ouellette G, Fortier I, Raelson J, Sherbatich T, Riazanskaia N, Rogaev E, Raeymaekers P, Aerssens J, Konings F, Luyten W, Macciardi F, Sham PC, Straub RE, Weinberger DR, Cohen N, Cohen D. Genetic and physiological data implicating the new human gene G72 and the gene for D-amino acid oxidase in schizophrenia. Proc Natl Acad Sci U S A. 2002 Oct 15;99(21):13675-80. Chung S, Jung J, Chung HY, Yoo HK, Kim CY, Joo YH, Choi SE, Hong JP. No association between polymorphisms of DAO and DAOA genes and homicidal behaviors in Korean schizophrenia. Psychiatr Genet. 2007 Oct;17(5):313. 27 Corvin A, McGhee KA, Murphy K, Donohoe G, Nangle JM, Schwaiger S, Kenny N, Clarke S, Meagher D, Quinn J, Scully P, Baldwin P, Browne D, Walsh C, Waddington JL, Morris DW, Gill M. Evidence for association and epistasis at the DAOA/G30 and D-amino acid oxidase loci in an Irish schizophrenia sample. Am J Med Genet B Neuropsychiatr Genet. 2007 Oct 5;144B(7):949-53. Corvin A, Donohoe G, McGhee K, Murphy K, Kenny N, Schwaiger S, Nangle JM, Morris D, Gill M. D-amino acid oxidase (DAO) genotype and mood symptomatology in schizophrenia. Neurosci Lett. 2007 Oct 16;426(2):97-100. Dalvie S, Horn N, Nossek C, van der Merwe L, Stein DJ, Ramesar R. Psychosis and relapse in bipolar disorder are related to GRM3, DAOA, and GRIN2B genotype. Afr J Psychiatry (Johannesbg). 2010 Sep;13(4):297-301. Detera-Wadleigh SD, McMahon FJ. G72/G30 in schizophrenia and bipolar disorder: review and meta-analysis. Biol Psychiatry. 2006 Jul 15;60(2):106-14. Di Maria E, Bonvicini C, Bonomini C, Alberici A, Zanetti O, Gennarelli M. Genetic variation in the G720/G30 gene locus (DAOA) influences the occurrence of psychotic symptoms in patients with Alzheimer's disease. J Alzheimers Dis. 2009;18(4):953-60. Donohoe G, Morris DW, Robertson IH, McGhee KA, Murphy K, Kenny N, Clarke S, Gill M, Corvin AP. DAOA ARG30LYS and verbal memory function in schizophrenia. Mol Psychiatry. 2007 Sep;12(9):795-6. Fallin MD, Lasseter VK, Avramopoulos D, Nicodemus KK, Wolyniec PS, McGrath JA, Steel G, Nestadt G, Liang KY, Huganir RL, Valle D, Pulver AE. Bipolar I disorder and schizophrenia: a 440single-nucleotide polymorphism screen of 64 candidate genes among Ashkenazi Jewish case-parent trios. Am J Hum Genet. 2005 Dec;77(6):918-36. Gawlik M, Wehner I, Mende M, Jung S, Pfuhlmann B, Knapp M, Stöber G. The DAOA/G30 locus and affective disorders: haplotype based association study in a polydiagnostic approach. BMC Psychiatry. 2010 Jul 29;10:59. Gaysina D, Cohen-Woods S, Chow PC, Martucci L, Schosser A, Ball HA, Tozzi F, Perry J, Muglia P, Kennedy JL, King N, Vincent JB, Parikh SV, Strauss J, Craig IW, McGuffin P, Farmer A. Association analysis of DAOA and DAO in bipolar disorder: results from two independent case-control studies. Bipolar Disord. 2010 Aug;12(5):579-81. Goldberg TE, Straub RE, Callicott JH, Hariri A, Mattay VS, Bigelow L, Coppola R, Egan MF, Weinberger DR. The G72/G30 gene complex and cognitive abnormalities in schizophrenia. Neuropsychopharmacology. 2006 Sep;31(9):2022-32. Gomez L, Wigg K, Feng Y, Kiss E, Kapornai K, Tamás Z, Mayer L, Baji I, Daróczi G, Benák I, Kothencné VO, Dombovári E, Kaczvinszk E, Besnyo M, Gádoros J, King N, Székely J, Kovacs M, Vetró A, Kennedy JL, Barr CL. G72/G30 (DAOA) and juvenile-onset mood disorders. Am J Med Genet B Neuropsychiatr Genet. 2009 Oct 5;150B(7):1007-12. Grigoroiu-Serbanescu M, Herms S, Diaconu CC, Jamra RA, Meier S, Bleotu C, Neagu AI, Prelipceanu D, Sima D, Gherghel M, Mihailescu R, Rietschel M, Nöthen MM, Cichon S, Mühleisen TW. Possible association of different G72/G30 SNPs with mood episodes and persecutory delusions in bipolar I Romanian patients. Prog Neuropsychopharmacol Biol Psychiatry. 2010 May 30;34(4):657-63. Hall D, Gogos JA, Karayiorgou M. The contribution of three strong candidate schizophrenia susceptibility genes in demographically distinct populations. Genes Brain Behav. 2004 Aug;3(4):240-8. Hall J, Whalley HC, Moorhead TW, Baig BJ, McIntosh AM, Job DE, Owens DG, Lawrie SM, Johnstone EC. Genetic variation in the DAOA (G72) gene modulates hippocampal function in subjects at high risk of schizophrenia. Biol Psychiatry. 2008 Sep 1;64(5):428-33. Hattori E, Liu C, Badner JA, Bonner TI, Christian SL, Maheshwari M, Detera-Wadleigh SD, Gibbs RA, Gershon ES. Polymorphisms at the G72/G30 gene locus, on 13q33, are associated with bipolar disorder in two independent pedigree series. Am J Hum Genet. 2003 May;72(5):1131-40. Hong CJ, Hou SJ, Yen FC, Liou YJ, Tsai SJ. Family-based association study between G72/G30 genetic polymorphism and schizophrenia. Neuroreport. 2006 Jul 17;17(10):1067-9. Hukic DS, Frisén L, Backlund L, Lavebratt C, Landén M, Träskman-Bendz L, Edman G, Schalling M, Ösby U. Cognitive manic symptoms in bipolar disorder associated with polymorphisms in the DAOA and COMT genes. PLoS One. 2013 Jul 5;8(7):e67450. Jansen A, Krach S, Krug A, Markov V, Eggermann T, Zerres K, Thimm M, Nöthen MM, Treutlein J, Rietschel M, Kircher T. Effect of the G72 (DAOA) putative risk haplotype on cognitive functions in healthy subjects. BMC Psychiatry. 2009 Sep 24;9:60. Jansen A, Krach S, Krug A, Markov V, Thimm M, Paulus FM, Zerres K, Stöcker T, Shah NJ, Nöthen MM, Treutlein J, Rietschel M, Kircher T. The effect of G72 genotype on neural correlates of memory encoding and retrieval. Neuroimage. 2010 Nov 15;53(3):1001-6. Jönsson EG, Saetre P, Vares M, Andreou D, Larsson K, Timm S, Rasmussen HB, Djurovic S, Melle I, Andreassen OA, Agartz I, Werge T, Hall H, Terenius L. DTNBP1, NRG1, DAOA, DAO and GRM3 polymorphisms and schizophrenia: an association study. Neuropsychobiology. 2009;59(3):142-50. Korostishevsky M, Kaganovich M, Cholostoy A, Ashkenazi M, Ratner Y, Dahary D, Bernstein J, Bening-Abu-Shach U, Ben-Asher E, Lancet D, Ritsner M, Navon R. Is the G72/G30 locus associated with schizophrenia? single nucleotide polymorphisms,haplotypes, and gene expression analysis. Biol Psychiatry. 2004 Aug 1;56(3):169-76. Korostishevsky M, Kremer I, Kaganovich M, Cholostoy A, Murad I, Muhaheed M, Bannoura I, Rietschel M, Dobrusin M, Bening-Abu-Shach U, Belmaker RH, Maier W, Ebstein RP, Navon R. Transmission disequilibrium and haplotype analyses of the G72/G30 locus: suggestive linkage to schizophrenia in Palestinian Arabs living in the North of Israel. Am J Med Genet B Neuropsychiatr Genet. 2006 Jan 5;141B(1):91-5. Kotaka T, Ujike H, Okahisa Y, Takaki M, Nakata K, Kodama M, Inada T, Yamada M, Uchimura N, Iwata N, Sora I, Iyo M, Ozaki N, Kuroda S. G72 gene is associated with susceptibility to methamphetamine psychosis. Prog Neuropsychopharmacol Biol Psychiatry. 2009 Aug 31;33(6):1046-9. Krug A, Markov V, Krach S, Jansen A, Zerres K, Eggermann T, Stöcker T, Shah NJ, Nöthen MM, Georgi A, Strohmaier J, Rietschel M, Kircher T. Genetic variation in G72 correlates with brain activation in the right middle temporal gyrus in a verbal fluency task in healthy individuals. Hum Brain Mapp. 2011 Jan;32(1):118-26. 28 Li D, He L. G72/G30 genes and schizophrenia: a systematic meta-analysis of association studies. Genetics. 2007 Feb;175(2):917-22. Maheshwari M, Shi J, Badner JA, Skol A, Willour VL, Muzny DM, Wheeler DA, Gerald FR, Detera-Wadleigh S, McMahon FJ, Potash JB, Gershon ES, Liu C, Gibbs RA. Common and rare variants of DAOA in bipolar disorder. Am J Med Genet B Neuropsychiatr Genet. 2009 Oct 5;150B(7):960-6. Liu YL, Fann CS, Liu CM, Chang CC, Wu JY, Hung SI, Liu SK, Hsieh MH, Hwang TJ, Chan HY, Chen JJ, Faraone SV, Tsuang MT, Chen WJ, Hwu HG. No association of G72 and D-amino acid oxidase genes with schizophrenia. Schizophr Res. 2006 Oct;87(1-3):15-20. Ma J, Qin W, Wang XY, Guo TW, Bian L, Duan SW, Li XW, Zou FG, Fang YR, Fang JX, Feng GY, Gu NF, St Clair D, He L. Further evidence for the association between G72/G30 genes and schizophrenia in two ethnically distinct populations. Mol Psychiatry. 2006 May;11(5):479-87. Ma J, Sun J, Zhang H, Zhang R, Kang WH, Gao CG, Liu HS, Ma XH, Min ZX, Zhao WX, Ning QL, Wang SH, Zhang YC, Guo TW, Lu SM. Evidence for transmission disequilibrium at the DAOA gene locus in a schizophrenia family sample. Neurosci Lett. 2009 Sep 22;462(2):105-8. Maheshwari M, Shi J, Badner JA, Skol A, Willour VL, Muzny DM, Wheeler DA, Gerald FR, Detera-Wadleigh S, McMahon FJ, Potash JB, Gershon ES, Liu C, Gibbs RA. Common and rare variants of DAOA in bipolar disorder. Am J Med Genet B Neuropsychiatr Genet. 2009 Oct 5;150B(7):960-6. Mössner R, Schuhmacher A, Wagner M, Quednow BB, Frommann I, Kühn KU, Schwab SG, Rietschel M, Falkai P, Wölwer W, Ruhrmann S, Bechdolf A, Gaebel W, Klosterkötter J, Maier W. DAOA/G72 predicts the progression of prodromal syndromes to first episode psychosis. Eur Arch Psychiatry Clin Neurosci. 2010 Apr;260(3):209-15. Mulle JG, Chowdari KV, Nimgaonkar V, Chakravarti A. No evidence for association to the G72/G30 locus in an independent sample of schizophrenia families. Mol Psychiatry. 2005 May;10(5):431-3. Müller DJ, Zai CC, Shinkai T, Strauss J, Kennedy JL. Association between the DAOA/G72 gene and bipolar disorder and meta-analyses in bipolar disorder and schizophrenia. Bipolar Disord. 2011 Mar;13(2):198-207. Ohi K, Hashimoto R, Yasuda Y, Yoshida T, Takahashi H, Iike N, Fukumoto M, Takamura H, Iwase M, Kamino K, Ishii R, Kazui H, Sekiyama R, Kitamura Y, Azechi M, Ikezawa K, Kurimoto R, Kamagata E, Tanimukai H, Tagami S, Morihara T, Ogasawara M, Okochi M, Tokunaga H, Numata S, Ikeda M, Ohnuma T, Ueno S, Fukunaga T, Tanaka T, Kudo T, Arai H, Ohmori T, Iwata N, Ozaki N, Takeda M. Association study of the G72 gene with schizophrenia in a Japanese population: a multicenter study. Schizophr Res. 2009 Apr;109(1-3):80-5. Pae CU, Chiesa A, Serretti A. Influence of DAOA gene variants on antipsychotic response after switch to aripiprazole. Psychiatry Res. 2010 Jul 30;178(2):430-2. Prata D, Breen G, Osborne S, Munro J, St Clair D, Collier D. Association of DAO and G72(DAOA)/G30 genes with bipolar affective disorder. Am J Med Genet B Neuropsychiatr Genet. 2008 Sep 5;147B(6):914-7. Prata DP, Papagni SA, Mechelli A, Fu CH, Kambeitz J, Picchioni M, Kane F, Kalidindi S, McDonald C, Kravariti E, Toulopoulou T, Bramon E, Walshe M, Murray R, Collier DA, McGuire PK. Effect of D-amino acid oxidase activator (DAOA; G72) on brain function during verbal fluency. Hum Brain Mapp. 2012 Jan;33(1):143-53. Réthelyi JM, Bakker SC, Polgár P, Czobor P, Strengman E, Pásztor PI, Kahn RS, Bitter I. Association study of NRG1, DTNBP1, RGS4, G72/G30, and PIP5K2A with schizophrenia and symptom severity in a Hungarian sample. Am J Med Genet B Neuropsychiatr Genet. 2010 Apr 5;153B(3):792-801. Rietschel M, Beckmann L, Strohmaier J, Georgi A, Karpushova A, Schirmbeck F, Boesshenz KV, Schmäl C, Bürger C, Jamra RA, Schumacher J, Höfels S, Kumsta R, Entringer S, Krug A, Markov V, Maier W, Propping P, Wüst S, Kircher T, Nöthen MM, Cichon S, Schulze TG. G72 and its association with major depression and neuroticism in large population-based groups from Germany. Am J Psychiatry. 2008 Jun;165(6):753-62. Sacchetti E, Scassellati C, Minelli A, Valsecchi P, Bonvicini C, Pasqualetti P, Galluzzo A, Pioli R, Gennarelli M. Schizophrenia susceptibility and NMDA-receptor mediated signalling: an association study involving 32 tagSNPs of DAO, DAOA, PPP3CC, and DTNBP1 genes. BMC Med Genet. 2013 Mar 9;14:33. Sanders AR, Duan J, Levinson DF, Shi J, He D, Hou C, Burrell GJ, Rice JP, Nertney DA, Olincy A, Rozic P, Vinogradov S, Buccola NG, Mowry BJ, Freedman R, Amin F, Black DW, Silverman JM, Byerley WF, Crowe RR, Cloninger CR, Martinez M, Gejman PV. No significant association of 14 candidate genes with schizophrenia in a large European ancestry sample: implications for psychiatric genetics. Am J Psychiatry. 2008 Apr;165(4):497-506. Schultz CC, Nenadic I, Koch K, Wagner G, Roebel M, Schachtzabel C, Mühleisen TW, Nöthen MM, Cichon S, Deufel T, Kiehntopf M, Rietschel M, Reichenbach JR, Sauer H, Schlösser RG. Reduced cortical thickness is associated with the glutamatergic regulatory gene risk variant DAOA Arg30Lys in schizophrenia. Neuropsychopharmacology. 2011 Jul;36(8):1747-53. Schulze TG, Ohlraun S, Czerski PM, Schumacher J, Kassem L, Deschner M, Gross M, Tullius M, Heidmann V, Kovalenko S, Jamra RA, Becker T, Leszczynska-Rodziewicz A, Hauser J, Illig T, Klopp N, Wellek S, Cichon S, Henn FA, McMahon FJ, Maier W, Propping P, Nöthen MM, Rietschel M. Genotype-phenotype studies in bipolar disorder showing association between the DAOA/G30 locus and persecutory delusions: a first step toward a molecular genetic classification of psychiatric phenotypes. Am J Psychiatry. 2005 Nov;162(11):2101-8. Schumacher J, Jamra RA, Freudenberg J, Becker T, Ohlraun S, Otte AC, Tullius M, Kovalenko S, Bogaert AV, Maier W, Rietschel M, Propping P, Nöthen MM, Cichon S. Examination of G72 and D-amino-acid oxidase as genetic risk factors for schizophrenia and bipolar affective disorder. Mol Psychiatry. 2004 Feb;9(2):203-7. Schumacher J, Abou Jamra R, Becker T, Klopp N, Franke P, Jacob C, Sand P, Fritze J, Ohlraun S, Schulze TG, Rietschel M, Illig T, Propping P, Cichon S, Deckert J, Nöthen MM. Investigation of the DAOA/G30 locus in panic disorder. Mol Psychiatry. 2005 May;10(5):428-9. Seifuddin F, Mahon PB, Judy J, Pirooznia M, Jancic D, Taylor J, Goes FS, Potash JB, Zandi PP. Meta-analysis of genetic association studies on bipolar disorder. Am J Med Genet B Neuropsychiatr Genet. 2012 Jul;159B(5):508-18. Shi J, Badner JA, Gershon ES, Liu C. Allelic association of G72/G30 with schizophrenia and bipolar disorder: a comprehensive meta-analysis. Schizophr Res. 2008 Jan;98(1-3):89-97. Shi J, Badner JA, Gershon ES, Chunyu L, Willour VL, Potash JB. Further evidence for an association of G72/G30 with schizophrenia in Chinese. Schizophr Res. 2009 Feb;107(2-3):324-6. Shin HD, Park BL, Kim EM, Lee SO, Cheong HS, Lee CH, Kim SG, Sohn JW, Park CS, Kim JW, Kim BH, Kim IY, Choi IG, Woo SI. Association analysis of G72/G30 polymorphisms with schizophrenia in the Korean population. Schizophr Res. 2007 Nov;96(1-3):119-24. 29 Shinkai T, De Luca V, Hwang R, Müller DJ, Lanktree M, Zai G, Shaikh S, Wong G, Sicard T, Potapova N, Trakalo J, King N, Matsumoto C, Hori H, Wong AH, Ohmori O, Macciardi F, Nakamura J, Kennedy JL. Association analyses of the DAOA/G30 and D-amino-acid oxidase genes in schizophrenia: further evidence for a role in schizophrenia. Neuromolecular Med. 2007;9(2):169-77. Soronen P, Silander K, Antila M, Palo OM, Tuulio-Henriksson A, Kieseppä T, Ellonen P, Wedenoja J, Turunen JA, Pietiläinen OP, Hennah W, Lönnqvist J, Peltonen L, Partonen T, Paunio T. Association of a nonsynonymous variant of DAOA with visuospatial ability in a bipolar family sample. Biol Psychiatry. 2008 Sep 1;64(5):438-42. Soronen P, Mantere O, Melartin T, Suominen K, Vuorilehto M, Rytsälä H, Arvilommi P, Holma I, Holma M, Jylhä P, Valtonen HM, Haukka J, Isometsä E, Paunio T. P2RX7 gene is associated consistently with mood disorders and predicts clinical outcome in three clinical cohorts. Am J Med Genet B Neuropsychiatr Genet. 2011 Jun;156B(4):435-47. Stefanis NC, Trikalinos TA, Avramopoulos D, Smyrnis N, Evdokimidis I, Ntzani EE, Ioannidis JP, Stefanis CN. Impact of schizophrenia candidate genes on schizotypy and cognitive endophenotypes at the population level. Biol Psychiatry. 2007 Oct 1;62(7):784-92. Suliman H, Schumacher J, Becker T, Cichon S, Schulze TG, Propping P, Rietschel M, Nöthen MM, Jamra RA. Association study of 20 genetic variants at the (D)-amino acid oxidase gene in schizophrenia. Psychiatr Genet. 2010 Apr;20(2):82-3. Tan J, Lin Y, Su L, Yan Y, Chen Q, Jiang H, Wei Q, Gu L. Association between DAOA gene polymorphisms and the risk of schizophrenia, bipolar disorder and depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2014 Jun 3;51:89-98. Vilella E, Costas J, Sanjuan J, Guitart M, De Diego Y, Carracedo A, Martorell L, Valero J, Labad A, De Frutos R, Nájera C, Moltó MD, Toirac I, Guillamat R, Brunet A, Vallès V, Pérez L, Leon M, de Fonseca FR, Phillips C, Torres M. Association of schizophrenia with DTNBP1 but not with DAO, DAOA, NRG1 and RGS4 nor their genetic interaction. J Psychiatr Res. 2008 Mar;42(4):278-88. Williams NM, Green EK, Macgregor S, Dwyer S, Norton N, Williams H, Raybould R, Grozeva D, Hamshere M, Zammit S, Jones L, Cardno A, Kirov G, Jones I, O'Donovan MC, Owen MJ, Craddock N. Variation at the DAOA/G30 locus influences susceptibility to major mood episodes but not psychosis in schizophrenia and bipolar disorder. Arch Gen Psychiatry. 2006 Apr;63(4):366-73. Wang X, He G, Gu N, Yang J, Tang J, Chen Q, Liu X, Shen Y, Qian X, Lin W, Duan Y, Feng G, He L. Association of G72/G30 with schizophrenia in the Chinese population. Biochem Biophys Res Commun. 2004 Jul 9;319(4):1281-6. Wood LS, Pickering EH, Dechairo BM. Significant support for DAO as a schizophrenia susceptibility locus: examination of five genes putatively associated with schizophrenia. Biol Psychiatry. 2007 May 15;61(10):1195-9. Yang HC, Liu CM, Liu YL, Chen CW, Chang CC, Fann CS, Chiou JJ, Yang UC, Chen CH, Faraone SV, Tsuang MT, Hwu HG. The DAO gene is associated with schizophrenia and interacts with other genes in the Taiwan Han Chinese population. PLoS One. 2013;8(3):e60099. Yue W, Liu Z, Kang G, Yan J, Tang F, Ruan Y, Zhang J, Zhang D. Association of G72/G30 polymorphisms with early-onset and male schizophrenia. Neuroreport. 2006 Dec 18;17(18):1899902. Yue W, Kang G, Zhang Y, Qu M, Tang F, Han Y, Ruan Y, Lu T, Zhang J, Zhang D. Association of DAOA polymorphisms with schizophrenia and clinical symptoms or therapeutic effects. Neurosci Lett. 2007 Apr 6;416(1):96-100. Zhang Z, Li Y, Zhao Q, Huang K, Wang P, Yang P, Li S, Feng G, Lindpaintner K, He L, Shi Y. First evidence of association between G72 and bipolar disorder in the Chinese Han population. Psychiatr Genet. 2009 Jun;19(3):151-3. Zuliani R, Moorhead TW, Job D, McKirdy J, Sussmann JE, Johnstone EC, Lawrie SM, Brambilla P, Hall J, McIntosh AM. Genetic variation in the G72 (DAOA) gene affects temporal lobe and amygdala structure in subjects affected by bipolar disorder. Bipolar Disord. 2009 Sep;11(6):621-7. Zou F, Li C, Duan S, Zheng Y, Gu N, Feng G, Xing Y, Shi J, He L. A family-based study of the association between the G72/G30 genes and schizophrenia in the Chinese population. Schizophr Res. 2005 Mar 1;73(2-3):257-61. 30 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Emamian, E.S., Hall, D., Birnbaum, M.J., Karayiorgou, M. & Gogos, J.A. Convergent evidence for impaired AKT1-GSK3beta signaling in schizophrenia. Nat Genet 36, 131-7 (2004). Gilman, S.R. et al. Diverse types of genetic variation converge on functional gene networks involved in schizophrenia. Nature neuroscience 15, 1723-8 (2012). Freedman, R. et al. Linkage of a neurophysiological deficit in schizophrenia to a chromosome 15 locus. Proceedings of the National Academy of Sciences of the United States of America 94, 587-592 (1997). Leonard, S. et al. Association of promoter variants in the alpha 7 nicotinic acetylcholine receptor subunit gene with an inhibitory deficit found in schizophrenia. Arch. Gen. Psych. 59, 1085-1096 (2002). Freedman, R., Hall, M., Adler, L.E. & Leonard, S. Evidence in postmortem brain tissue for decreased numbers of hippocampal nicotinic receptors in schizophrenia. Biol. Psych. 38, 22-33 (1995). Stephens, S.H. et al. Association of the 5'-upstream regulatory region of the α7 nicotinic acetylcholine receptor subunit gene (CHRNA7) with schizophrenia. Schizo.Res. 109, 102-112 (2009). Stone, J.L. et al. Rare chromosomal deletions and duplications increase risk of schizophrenia. Nature 455, 237-241 (2008). Stefansson, H. et al. Large recurrent microdeletions associated with schizophrenia. Nature 455, 232-237 (2008). Gault, J. et al. Genomic organization and partial duplication of the human α7 neuronal nicotinic acetylcholine receptor gene. Genomics 52, 173-185 (1998). Araud, T. et al. The duplicated alpha 7 nicotinic receptor gene CHRFAM7A is a dominant negative regulator of CHRNA7 expression. Biochem. Pharmacol. 82, 904914 (2011). Li, T. et al. Preferential transmission of the high activity allele of COMT in schizophrenia. Psychiatr Genet 6, 131-133 (1996). Allen, N.C. et al. Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: the SzGene database. Nat Genet 40, 827-834 (2008). Sullivan, P.F. et al. Genomewide association for schizophrenia in the CATIE study: results of stage 1. Mol Psychiatry 13, 570-584 (2008). Gothelf, D. et al. Biological effects of COMT haplotypes and psychosis risk in 22q11.2 deletion syndrome. Biol Psychiatry 75, 406-413 (2014). Gothelf, D. et al. COMT genotype predicts longitudinal cognitive decline and psychosis in 22q11.2 deletion syndrome. Nat Neurosci 8, 1500-2 (2005). Caspi, A. et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry 57, 111727 (2005). 31 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. Henquet, C. et al. An experimental study of catechol-o-methyltransferase Val158Met moderation of delta-9-tetrahydrocannabinol-induced effects on psychosis and cognition. Neuropsychopharmacology 31, 2748-2757 (2006). Egan, M.F. et al. Effect of COMT Val108/158 Met genotype on frontal lobe function and risk for schizophrenia. Proc Natl Acad Sci U S A 98, 6917-6922 (2001). Kaenmaki, M. et al. Quantitative role of COMT in dopamine clearance in the prefrontal cortex of freely moving mice. J Neurochem 114, 1745-1755 (2010). Papaleo, F., Erickson, L., Liu, G., Chen, J. & Weinberger, D.R. Effects of sex and COMT genotype on environmentally modulated cognitive control in mice. Proc Natl Acad Sci U S A 109, 20160-20165 (2012). Papaleo, F. et al. Genetic dissection of the role of catechol-O-methyltransferase in cognition and stress reactivity in mice. J Neurosci 28, 8709-8723 (2008). Risbrough, V., Ji, B., Hauger, R. & Zhou, X. Generation and Characterization of Humanized Mice Carrying COMT158 Met/Val Alleles. Neuropsychopharmacology (2014). Bray, N.J. et al. A haplotype implicated in schizophrenia susceptibility is associated with reduced COMT expression in human brain. Am J Hum Genet 73, 152-161 (2003). Chen, J. et al. Functional analysis of genetic variation in catechol-Omethyltransferase (COMT): effects on mRNA, protein, and enzyme activity in postmortem human brain. Am J Hum Genet 75, 807-821 (2004). Nackley, A.G. et al. Human catechol-O-methyltransferase haplotypes modulate protein expression by altering mRNA secondary structure. Science 314, 1930-1933 (2006). Cools, R. & D'Esposito, M. Inverted-U-shaped dopamine actions on human working memory and cognitive control. Biol Psychiatry 69, 113-125 (2011). Papaleo, F., Burdick, M.C., Callicott, J.H. & Weinberger, D.R. COMT-Dysbindin epistatic interaction. Mol Psychiatry 19, 273-273 (2014). Costas, J. et al. Interaction between COMT haplotypes and cannabis in schizophrenia: a case-only study in two samples from Spain. Schizophr Res 127, 22-7 (2011). Chumakov, I. et al. Genetic and physiological data implicating the new human gene G72 and the gene for D-amino acid oxidase in schizophrenia. Proc Natl Acad Sci U S A 99, 13675-80 (2002). Schumacher, J. et al. Examination of G72 and D-amino-acid oxidase as genetic risk factors for schizophrenia and bipolar affective disorder. Mol Psychiatry 9, 203-7 (2004). Detera-Wadleigh, S.D. & McMahon, F.J. G72/G30 in schizophrenia and bipolar disorder: review and meta-analysis. Biol Psychiatry 60, 106-14 (2006). Shi, J., Badner, J.A., Gershon, E.S. & Liu, C. Allelic association of G72/G30 with schizophrenia and bipolar disorder: a comprehensive meta-analysis. Schizophr Res 98, 89-97 (2008). Muller, D.J., Zai, C.C., Shinkai, T., Strauss, J. & Kennedy, J.L. Association between the DAOA/G72 gene and bipolar disorder and meta-analyses in bipolar disorder and schizophrenia. Bipolar Disord 13, 198-207 (2011). 32 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. Tan, J. et al. Association between DAOA gene polymorphisms and the risk of schizophrenia, bipolar disorder and depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry 51, 89-98 (2014). Millar, J.K. et al. Disruption of two novel genes by a translocation co-segregating with schizophrenia. Human Molecular Genetics 9, 1415-23 (2000). Blackwood, D.H. et al. Schizophrenia and affective disorders--cosegregation with a translocation at chromosome 1q42 that directly disrupts brain-expressed genes: clinical and P300 findings in a family. American Journal of Human Genetics 69, 42833 (2001). Brandon, N.J. & Sawa, A. Linking neurodevelopmental and synaptic theories of mental illness through DISC1. Nat Rev Neurosci 12, 707-22 (2011). Bradshaw, N.J. & Porteous, D.J. DISC1-binding proteins in neural development, signalling and schizophrenia. Neuropharmacology 62, 1230-41 (2012). Song, W. et al. Identification of high risk DISC1 structural variants with a 2% attributable risk for schizophrenia. Biochemical and Biophysical Research Communications 367, 700-706 (2008). Thomson, P.A. et al. 708 Common and 2010 rare DISC1 locus variants identified in 1542 subjects: analysis for association with psychiatric disorder and cognitive traits. Mol Psychiatry (2013). Sanders, S.J. et al. De novo mutations revealed by whole-exome sequencing are strongly associated with autism. Nature 485, 237-41 (2012). Mathieson, I., Munafo, M.R. & Flint, J. Meta-analysis indicates that common variants at the DISC1 locus are not associated with schizophrenia. Molecular Psychiatry 17, 634-41 (2012). Ripke, S. et al. Genome-wide association analysis identifies 13 new risk loci for schizophrenia. Nat Genet 45, 1150-9 (2013). Soares, D.C., Carlyle, B.C., Bradshaw, N.J. & Porteous, D.J. DISC1: Structure, Function, and Therapeutic Potential for Major Mental Illness. ACS Chem Neurosci 2, 609-632 (2011). Hennah, W. & Porteous, D. The DISC1 pathway modulates expression of neurodevelopmental, synaptogenic and sensory perception genes. PLoS One 4, e4906 (2009). Carless, M.A. et al. Impact of DISC1 variation on neuroanatomical and neurocognitive phenotypes. Molecular Psychiatry 16, 1096-104, 1063 (2011). Zhou, M. et al. mTOR Inhibition ameliorates cognitive and affective deficits caused by Disc1 knockdown in adult-born dentate granule neurons. Neuron 77, 647-54 (2013). Leliveld, S.R. et al. Oligomer Assembly of the C-Terminal DISC1 Domain (640−854) Is Controlled by Self-Association Motifs and Disease-Associated Polymorphism S704C. Biochemistry 48, 7746-7755 (2009). Singh, K.K. et al. Common DISC1 polymorphisms disrupt Wnt/GSK3beta signaling and brain development. Neuron 72, 545-58 (2011). Malavasi, E.L., Ogawa, F., Porteous, D.J. & Millar, J.K. DISC1 variants 37W and 607F disrupt its nuclear targeting and regulatory role in ATF4-mediated transcription. Human Molecular Genetics 21, 2779-92 (2012). 33 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. Ogawa, F. et al. DISC1 complexes with TRAK1 and Miro1 to modulate anterograde axonal mitochondrial trafficking. Hum Mol Genet (2013). Bertram, L., Lill, C.M. & Tanzi, R.E. The genetics of Alzheimer disease: back to the future. Neuron 68, 270-81 (2010). Corripio, I. et al. Density of striatal D2 receptors in untreated first-episode psychosis: an I123-IBZM SPECT study. Eur Neuropsychopharmacol 21, 861-6 (2011). Seeman, P. Schizophrenia and dopamine receptors. Eur Neuropsychopharmacol 23, 999-1009 (2013). Seeman, P. et al. Dopamine supersensitivity correlates with D2High states, implying many paths to psychosis. Proc Natl Acad Sci U S A 102, 3513-8 (2005). Ward, L.D. & Kellis, M. HaploReg: a resource for exploring chromatin states, conservation, and regulatory motif alterations within sets of genetically linked variants. Nucleic Acids Res 40, D930-4 (2012). Boyle, A.P. et al. Annotation of functional variation in personal genomes using RegulomeDB. Genome Res 22, 1790-7 (2012). Xu, Z. & Taylor, J.A. SNPinfo: integrating GWAS and candidate gene information into functional SNP selection for genetic association studies. Nucleic Acids Res 37, W6005 (2009). Yilmaz, Z. et al. Antipsychotics, dopamine D(2) receptor occupancy and clinical improvement in schizophrenia: a meta-analysis. Schizophr Res 140, 214-20 (2012). Zhang, J.P., Lencz, T. & Malhotra, A.K. D2 receptor genetic variation and clinical response to antipsychotic drug treatment: a meta-analysis. Am J Psychiatry 167, 763-72 (2010). Zai, C.C. et al. Meta-analysis of two dopamine D2 receptor gene polymorphisms with tardive dyskinesia in schizophrenia patients. Mol Psychiatry 12, 794-5 (2007). Bakker, P.R., van Harten, P.N. & van Os, J. Antipsychotic-induced tardive dyskinesia and polymorphic variations in COMT, DRD2, CYP1A2 and MnSOD genes: a metaanalysis of pharmacogenetic interactions. Mol Psychiatry 13, 544-56 (2008). Muller, D.J. et al. Systematic analysis of dopamine receptor genes (DRD1-DRD5) in antipsychotic-induced weight gain. Pharmacogenomics J 12, 156-64 (2012). Collins, A.L. et al. Hypothesis-driven candidate genes for schizophrenia compared to genome-wide association results. Psychol Med 42, 607-16 (2012). Girgenti, M.J., LoTurco, J.J. & Maher, B.J. ZNF804a regulates expression of the schizophrenia-associated genes PRSS16, COMT, PDE4B, and DRD2. PLoS One 7, e32404 (2012). Ferguson, S.S. Evolving concepts in G protein-coupled receptor endocytosis: the role in receptor desensitization and signaling. Pharmacol Rev 53, 1-24 (2001). Williams, J. et al. Association between schizophrenia and T102C polymorphism of the 5-hydroxytryptamine type 2a-receptor gene. European Multicentre Association Study of Schizophrenia (EMASS) Group. Lancet 347, 1294-6 (1996). Hawi, Z. et al. No association or linkage between the 5-HT2a/T102C polymorphism and schizophrenia in Irish families. Am J Med Genet 74, 370-3 (1997). Erdmann, J. et al. Systematic screening for mutations in the human serotonin-2A (5HT2A) receptor gene: identification of two naturally occurring receptor variants and association analysis in schizophrenia. Hum Genet 97, 614-9 (1996). 34 70. 71. 72. 73. 74. 75. 76. 77. 78. 79. 80. 81. 82. 83. 84. 85. 86. 87. 88. Arranz, M.J., Lin, M.W., Powell, J., Kerwin, R. & Collier, D. 5HT 2a receptor T102C polymorphism and schizophrenia. Lancet 347, 1831-2 (1996). Ishigaki, T. et al. Intact 5-HT2A receptor exons and the adjoining intron regions in schizophrenia. Neuropsychopharmacology 14, 339-47 (1996). Malhotra, A.K., Goldman, D., Buchanan, R., Breier, A. & Pickar, D. 5HT 2a receptor T102C polymorphism and schizophrenia. Lancet 347, 1830-1 (1996). Sasaki, T., Hattori, M., Fukuda, R., Kunugi, H. & Nanko, S. 5HT 2a receptor T102C polymorphism and schizophrenia. Lancet 347, 1832 (1996). Saiz, P.A. et al. Association study of serotonin 2A receptor (5-HT2A) and serotonin transporter (5-HTT) gene polymorphisms with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 31, 741-5 (2007). Penas-Lledo, E.M., Dorado, P., Caceres, M.C., de la Rubia, A. & Llerena, A. Association between T102C and A-1438G polymorphisms in the serotonin receptor 2A (5HT2A) gene and schizophrenia: relevance for treatment with antipsychotic drugs. Clin Chem Lab Med 45, 835-8 (2007). Joober, R. et al. T102C polymorphism in the 5HT2A gene and schizophrenia: relation to phenotype and drug response variability. J Psychiatry Neurosci 24, 141-6 (1999). Ramanathan, S. & Glatt, S.J. Serotonergic system genes in psychosis of Alzheimer dementia: meta-analysis. Am J Geriatr Psychiatry 17, 839-46 (2009). Arranz, M.J. et al. Evidence for association between polymorphisms in the promoter and coding regions of the 5-HT2A receptor gene and response to clozapine. Mol Psychiatry 3, 61-6 (1998). Arranz, M. et al. Association between clozapine response and allelic variation in 5HT2A receptor gene. Lancet 346, 281-2 (1995). Masellis, M. et al. Serotonin subtype 2 receptor genes and clinical response to clozapine in schizophrenia patients. Neuropsychopharmacology 19, 123-32 (1998). Lin, C.H. et al. No evidence for association of serotonin-2A receptor variant (102T/C) with schizophrenia or clozapine response in a Chinese population. Neuroreport 10, 57-60 (1999). Malhotra, A.K. et al. Lack of association between polymorphisms in the 5-HT2A receptor gene and the antipsychotic response to clozapine. Am J Psychiatry 153, 1092-4 (1996). Nothen, M.M. et al. Genetic variation of the 5-HT2A receptor and response to clozapine. Lancet 346, 908-9 (1995). Schumacher, J., Schulze, T.G., Wienker, T.F., Rietschel, M. & Nothen, M.M. Pharmacogenetics of the clozapine response. Lancet 356, 506-7 (2000). Masellis, M. et al. Genetic variation of 5-HT2A receptor and response to clozapine. Lancet 346, 1108 (1995). Kirchheiner, J. et al. Pharmacogenetics of antidepressants and antipsychotics: the contribution of allelic variations to the phenotype of drug response. Mol Psychiatry 9, 442-73 (2004). Filippini, N. et al. Influence of serotonin receptor 2A His452Tyr polymorphism on brain temporal structures: a volumetric MR study. Eur J Hum Genet 14, 443-9 (2006). Schott, B.H. et al. Genetic variation of the serotonin 2a receptor affects hippocampal novelty processing in humans. PLoS One 6, e15984 (2011). 35 89. 90. 91. 92. 93. 94. 95. 96. 97. 98. 99. 100. 101. 102. 103. 104. 105. 106. Olajossy-Hilkesberger, L. et al. Polymorphisms of the 5-HT2A receptor gene and clinical response to olanzapine in paranoid schizophrenia. Neuropsychobiology 64, 202-10 (2011). Blasi, G. et al. Converging evidence for the association of functional genetic variation in the serotonin receptor 2a gene with prefrontal function and olanzapine treatment. JAMA Psychiatry 70, 921-30 (2013). Ozaki, N. et al. A naturally occurring amino acid substitution of the human serotonin 5-HT2A receptor influences amplitude and timing of intracellular calcium mobilization. J Neurochem 68, 2186-93 (1997). Hazelwood, L.A. & Sanders-Bush, E. His452Tyr polymorphism in the human 5-HT2A receptor destabilizes the signaling conformation. Mol Pharmacol 66, 1293-300 (2004). Bray, N.J., Buckland, P.R., Hall, H., Owen, M.J. & O'Donovan, M.C. The serotonin-2A receptor gene locus does not contain common polymorphism affecting mRNA levels in adult brain. Mol Psychiatry 9, 109-14 (2004). Smith, R.M. et al. Multiple regulatory variants modulate expression of 5hydroxytryptamine 2A receptors in human cortex. Biol Psychiatry 73, 546-54 (2013). Colantuoni, C. et al. Temporal dynamics and genetic control of transcription in the human prefrontal cortex. Nature 478, 519-23 (2011). Blouin, J.L. et al. Schizophrenia susceptibility loci on chromosomes 13q32 and 8p21. Nat Genet 20, 70-73 (1998). Pulver, A.E. et al. Schizophrenia: a genome scan targets chromosomes 3p and 8p as potential sites of susceptibility genes. Am J Med Genet 60, 252-260 (1995). Badner, J.A. & Gershon, E.S. Meta-analysis of whole-genome linkage scans of bipolar disorder and schizophrenia. Mol Psychiatry 7, 405-411 (2002). Stefansson, H. et al. Neuregulin 1 and susceptibility to schizophrenia. Am J Hum Genet 71, 877-92 (2002). Stefansson, H. et al. Association of neuregulin 1 with schizophrenia confirmed in a Scottish population. Am J Hum Genet 72, 83-87 (2003). Corvin, A.P. et al. Confirmation and refinement of an 'at-risk' haplotype for schizophrenia suggests the EST cluster, Hs.97362, as a potential susceptibility gene at the Neuregulin-1 locus. Mol Psychiatry 9, 208-213 (2004). Li, D., Collier, D.A. & He, L. Meta-analysis shows strong positive association of the neuregulin 1 (NRG1) gene with schizophrenia. Hum Mol Genet 15, 1995-2002 (2006). Munafo, M.R., Thiselton, D.L., Clark, T.G. & Flint, J. Association of the NRG1 gene and schizophrenia: a meta-analysis. Mol Psychiatry 11, 539-546 (2006). Gong, Y.G. et al. A two-method meta-analysis of Neuregulin 1(NRG1) association and heterogeneity in schizophrenia. Schizophr Res 111, 109-114 (2009). Agim, Z.S. et al. Discovery, validation and characterization of Erbb4 and Nrg1 haplotypes using data from three genome-wide association studies of schizophrenia. PLoS One 8(2013). Harrison, P.J. & Law, A.J. Neuregulin 1 and schizophrenia: genetics, gene expression, and neurobiology. Biol Psychiatry 60, 132-140 (2006). 36 107. 108. 109. 110. 111. 112. 113. 114. 115. 116. 117. 118. 119. 120. 121. 122. 123. 124. Hall, J. et al. A neuregulin 1 variant associated with abnormal cortical function and psychotic symptoms. Nat Neurosci 9, 1477-1478 (2006). Nicodemus, K.K. et al. Biological validation of increased schizophrenia risk with NRG1, ERBB4, and AKT1 epistasis via functional neuroimaging in healthy controls. Arch Gen Psychiatry 67, 991-991001 (2010). Knickmeyer, R.C. et al. Common variants in psychiatric risk genes predict brain structure at birth. Cereb Cortex 24, 1230-1246 (2014). Hashimoto, R. et al. Expression analysis of neuregulin-1 in the dorsolateral prefrontal cortex in schizophrenia. Mol Psychiatry 9, 299-307 (2004). Law, A.J. et al. Neuregulin 1 transcripts are differentially expressed in schizophrenia and regulated by 5' SNPs associated with the disease. Proc Natl Acad Sci U S A 103, 6747-6752 (2006). Moon, E. et al. Lack of association to a NRG1 missense polymorphism in schizophrenia or bipolar disorder in a Costa Rican population. Schizophr Res 131, 52-57 (2011). Law, A.J. unpublished observations. Deakin, I.H. et al. Transgenic overexpression of the type I isoform of neuregulin 1 affects working memory and hippocampal oscillations but not long-term potentiation. Cereb Cortex 22, 1520-1529 (2012). Yin, D.-M. et al. Reversal of behavioral deficits and synaptic dysfunction in mice overexpressing neuregulin 1. Neuron 78, 644-657 (2013). Nicodemus, K.K. et al. Serious obstetric complications interact with hypoxiaregulated/vascular-expression genes to influence schizophrenia risk. Mol Psychiatry 13, 873-877 (2008). Karl, T. Neuregulin 1: a prime candidate for research into gene-environment interactions in schizophrenia? Insights from genetic rodent models. Front Behav Neurosci 7, 106 (2013). Norton, N. et al. Evidence that interaction between neuregulin 1 and its receptor erbB4 increases susceptibility to schizophrenia. Am J Med Genet B Neuropsychiatr Genet 141B, 96-9101 (2006). Bani-Fatemi, A. et al. Analysis of CpG SNPs in 34 genes: association test with suicide attempt in schizophrenia. Schizophr Res 147, 262-8 (2013). So, H.C. et al. An association study of RGS4 polymorphisms with clinical phenotypes of schizophrenia in a Chinese population. Am J Med Genet B Neuropsychiatr Genet 147B, 77-85 (2008). Winantea, J. et al. A summary statistic approach to sequence variation in noncoding regions of six schizophrenia-associated gene loci. Eur J Hum Genet 14, 1037-43 (2006). Talkowski, M.E. et al. Evaluation of a susceptibility gene for schizophrenia: genotype based meta-analysis of RGS4 polymorphisms from thirteen independent samples. Biol Psychiatry 60, 152-62 (2006). Fallin, M.D. et al. Bipolar I disorder and schizophrenia: a 440-single-nucleotide polymorphism screen of 64 candidate genes among Ashkenazi Jewish case-parent trios. Am J Hum Genet 77, 918-36 (2005). Zhang, F. et al. Association analysis of the RGS4 gene in Han Chinese and Scottish populations with schizophrenia. Genes Brain Behav 4, 444-8 (2005). 37 125. 126. 127. 128. 129. 130. 131. 132. 133. 134. 135. 136. 137. 138. 139. 140. 141. Prasad, K.M. et al. Genetic polymorphisms of the RGS4 and dorsolateral prefrontal cortex morphometry among first episode schizophrenia patients. Mol Psychiatry 10, 213-9 (2005). Chen, X. et al. Regulator of G-protein signaling 4 (RGS4) gene is associated with schizophrenia in Irish high density families. Am J Med Genet B Neuropsychiatr Genet 129B, 23-6 (2004). Morris, D.W. et al. Confirming RGS4 as a susceptibility gene for schizophrenia. Am J Med Genet B Neuropsychiatr Genet 125B, 50-3 (2004). Williams, N.M. et al. Support for RGS4 as a susceptibility gene for schizophrenia. Biol Psychiatry 55, 192-5 (2004). Chowdari, K.V. et al. Association and linkage analyses of RGS4 polymorphisms in schizophrenia. Hum Mol Genet 11, 1373-80 (2002). Jonsson, E.G. et al. Lack of association between the regulator of G-protein signaling 4 (RGS4) rs951436 polymorphism and schizophrenia. Psychiatr Genet 22, 263-4 (2012). Rethelyi, J.M. et al. Association study of NRG1, DTNBP1, RGS4, G72/G30, and PIP5K2A with schizophrenia and symptom severity in a Hungarian sample. Am J Med Genet B Neuropsychiatr Genet 153B, 792-801 (2010). Sanders, A.R. et al. No significant association of 14 candidate genes with schizophrenia in a large European ancestry sample: implications for psychiatric genetics. Am J Psychiatry 165, 497-506 (2008). Ishiguro, H. et al. RGS4 is not a susceptibility gene for schizophrenia in Japanese: association study in a large case-control population. Schizophr Res 89, 161-4 (2007). Guo, S. et al. RGS4 polymorphisms and risk of schizophrenia: an association study in Han Chinese plus meta-analysis. Neurosci Lett 406, 122-7 (2006). Li, D. & He, L. Association study of the G-protein signaling 4 (RGS4) and proline dehydrogenase (PRODH) genes with schizophrenia: a meta-analysis. Eur J Hum Genet 14, 1130-5 (2006). Liu, Y.L. et al. Evaluation of RGS4 as a candidate gene for schizophrenia. Am J Med Genet B Neuropsychiatr Genet 141B, 418-20 (2006). Rizig, M.A. et al. Failure to confirm genetic association between schizophrenia and markers on chromosome 1q23.3 in the region of the gene encoding the regulator of G-protein signaling 4 protein (RGS4). Am J Med Genet B Neuropsychiatr Genet 141B, 296-300 (2006). Sobell, J.L., Richard, C., Wirshing, D.A. & Heston, L.L. Failure to confirm association between RGS4 haplotypes and schizophrenia in Caucasians. Am J Med Genet B Neuropsychiatr Genet 139B, 23-7 (2005). Cordeiro, Q. et al. Association and linkage analysis of RGS4 polymorphisms with schizophrenia and bipolar disorder in Brazil. Genes Brain Behav 4, 45-50 (2005). Volk, D.W., Eggan, S.M. & Lewis, D.A. Alterations in metabotropic glutamate receptor 1alpha and regulator of G protein signaling 4 in the prefrontal cortex in schizophrenia. Am J Psychiatry 167, 1489-98 (2010). Mirnics, K., Middleton, F.A., Stanwood, G.D., Lewis, D.A. & Levitt, P. Disease-specific changes in regulator of G-protein signaling 4 (RGS4) expression in schizophrenia. Mol Psychiatry 6, 293-301 (2001). 38 142. 143. 144. 145. 146. 147. 148. 149. 150. 151. 152. 153. 154. 155. 156. 157. 158. Ding, L. & Hegde, A.N. Expression of RGS4 splice variants in dorsolateral prefrontal cortex of schizophrenic and bipolar disorder patients. Biol Psychiatry 65, 541-5 (2009). Bowden, N.A., Scott, R.J. & Tooney, P.A. Altered expression of regulator of G-protein signalling 4 (RGS4) mRNA in the superior temporal gyrus in schizophrenia. Schizophr Res 89, 165-8 (2007). Erdely, H.A., Tamminga, C.A., Roberts, R.C. & Vogel, M.W. Regional alterations in RGS4 protein in schizophrenia. Synapse 59, 472-9 (2006). Schwendt, M., Sigmon, S.A. & McGinty, J.F. RGS4 overexpression in the rat dorsal striatum modulates mGluR5- and amphetamine-mediated behavior and signaling. Psychopharmacology (Berl) 221, 621-35 (2012). Vrajova, M., Pekova, S., Horacek, J. & Hoschl, C. The effects of siRNA-mediated RGS4 gene silencing on the whole genome transcription profile: implications for schizophrenia. Neuro Endocrinol Lett 32, 246-52 (2011). Chowdari, K.V. et al. Linkage disequilibrium patterns and functional analysis of RGS4 polymorphisms in relation to schizophrenia. Schizophr Bull 34, 118-26 (2008). Gu, Z., Jiang, Q. & Yan, Z. RGS4 modulates serotonin signaling in prefrontal cortex and links to serotonin dysfunction in a rat model of schizophrenia. Mol Pharmacol 71, 1030-9 (2007). Ebert, P.J., Campbell, D.B. & Levitt, P. Bacterial artificial chromosome transgenic analysis of dynamic expression patterns of regulator of G-protein signaling 4 during development. II. Subcortical regions. Neuroscience 142, 1163-81 (2006). Jaen, C. & Doupnik, C.A. RGS3 and RGS4 differentially associate with G proteincoupled receptor-Kir3 channel signaling complexes revealing two modes of RGS modulation. Precoupling and collision coupling. J Biol Chem 281, 34549-60 (2006). Gong, Y. et al. Polymorphisms in microRNA target sites influence susceptibility to schizophrenia by altering the binding of miRNAs to their targets. Eur Neuropsychopharmacol 23, 1182-9 (2013). Cheng, Y.C. et al. Zebrafish rgs4 is essential for motility and axonogenesis mediated by Akt signaling. Cell Mol Life Sci 70, 935-50 (2013). Paspalas, C.D., Selemon, L.D. & Arnsten, A.F. Mapping the regulator of G protein signaling 4 (RGS4): presynaptic and postsynaptic substrates for neuroregulation in prefrontal cortex. Cereb Cortex 19, 2145-55 (2009). Kang, G. et al. Two-stage designs to identify the effects of SNP combinations on complex diseases. J Hum Genet 53, 739-46 (2008). Nicodemus, K.K. et al. Evidence for statistical epistasis between catechol-Omethyltransferase (COMT) and polymorphisms in RGS4, G72 (DAOA), GRM3, and DISC1: influence on risk of schizophrenia. Hum Genet 120, 889-906 (2007). Lipska, B.K. et al. RGS4 mRNA expression in postmortem human cortex is associated with COMT Val158Met genotype and COMT enzyme activity. Hum Mol Genet 15, 2804-12 (2006). Buckholtz, J.W. et al. Allelic variation in RGS4 impacts functional and structural connectivity in the human brain. J Neurosci 27, 1584-93 (2007). Kattoulas, E. et al. Schizophrenia-related RGS4 gene variations specifically disrupt prefrontal control of saccadic eye movements. Psychol Med 42, 757-67 (2012). 39 159. 160. 161. 162. 163. 164. 165. Prasad, K.M. et al. RGS4 polymorphisms associated with variability of cognitive performance in a family-based schizophrenia sample. Schizophr Bull 36, 983-90 (2010). Stefanis, N.C. et al. Association of RGS4 variants with schizotypy and cognitive endophenotypes at the population level. Behav Brain Funct 4, 46 (2008). Lane, H.Y. et al. RGS4 polymorphisms predict clinical manifestations and responses to risperidone treatment in patients with schizophrenia. J Clin Psychopharmacol 28, 64-8 (2008). Campbell, D.B. et al. Ethnic stratification of the association of RGS4 variants with antipsychotic treatment response in schizophrenia. Biol Psychiatry 63, 32-41 (2008). Rivero, G. et al. Brain RGS4 and RGS10 protein expression in schizophrenia and depression. Effect of drug treatment. Psychopharmacology (Berl) 226, 177-88 (2013). Allen, N. et al. Systematic meta-analyses and field synopsis of genetic association studies in schizophrenia: The SzGene Database. Nature Genetics 40, 827-34 (2008). Schizophrenia Working Group of the Psychiatric Genomics Consortium. Genomewide association analysis identifies more than 100 loci for schizophrenia. (Submitted). 40