Patient History Form
advertisement

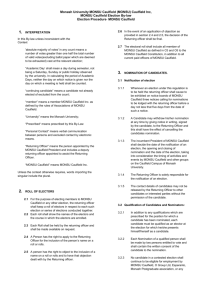
Patient History Date_________________ Name______________________________________________Age______Date of Birth______________ Phone ______________ Recent Primary Care Physician___________________Are you Changing Primary Care to This facility: Y/N Current Medication: If you are a returning patient with no change to medication check here---------------------------Name Strength (i.e. 25mg) Amount (i.e. 1 tab…) Frequency (Once in AM, twice a day…) 30/90 day supply Past Medical History: If you are a returning patient with no change to History check here-------------------------------Check all that apply to you, list additional in remaining boxes Asthma Blood Transfusion Heart Murmur Glaucoma Sleep Apnea Heart Disease Angina Cancer________ Heart Attack GERD Blood Clot Thyroid Arthritis Chronic Pain High Blood Press Kidney Stone Colitis Diabetes Aneurysm Cirrhosis High Cholesterol Pancreatitis HIV/AIDS Anemia Emphysema/COPD Hepatitis _____ Stroke Ulcers A. Fib Diverticulosis/itis Hearing Loss Tuberculosis Allergies Immunizations: If you are a returning patient with no change to Immunizations check here------------------------------Year Year Year Year Other Flu Pneumovax (Pneumonia) ZostaVax (shingles) Tetanus / TdaP Hepatitis A Hepatitis B Medication Allergies: If you are a returning patient with no change to allergies check here------------------------------Medication Reaction Medication Reaction Medication Reaction Surgical History: If you are a returning patient with no change to surgical history check here----------------------------Surgery Year Surgery Year Surgery Year Colonoscopy Hospitalization: If you are a returning patient with no hospitalizations since last visit check here----------------------Date Reason Date Reason Family History: If you are a returning patient with no change to family history check here-------------------------------Arthritis Blood Press Colon Cancer Stroke Blood Clots Cholesterol Breast Cancer Melanoma Diabetes Heart disease Prostate cancer Thyroid Social History: If you are a returning patient with no change to social history check here------------------------------------Marital Status Tobacco Use None/Current/Former Employment Status Alcohol Use None/Current/Former Number of Children Recreational Drug Use None/Current/Former Gynecological History: If you are a returning patient with no change to gyn history check here------------------------Date Date Date Last PAP Last Mammogram Last Bone Density Scan Patient/Guardian Signature ____________________________________By signing I acknowledge that above information is correct to the best of my knowledge. Patient History Date_________________ Name____________________________________________ Date of Birth_____________ To help your appointment flow in a timely fashion and avoid overlooking issues, please list the 4 issues you wish to address in your time with the doctor today: (i.e. follow up on blood pressure, sore throat…) 1.___________________________________________________2.________________________________________________ 3.___________________________________________________4.________________________________________________ Please Circle all that apply to the above listed complaints and to today’s visit: Constitutional Chills Fatigue Eyes Blurring of vision Ear pain Runny Nose Ears, Nose, Mouth & Throat Fever Weight loss/Gain Change in vision Hearing loss Eye Drainage Nasal congestion Sore throat Nose bleeds Sputum Production Wheezing Respiratory Cough Shortness of breath Cardiovascular Leg swelling Chest pain Cold extremities Gastrointestinal Black stools Diarrhea Blood in stool Heartburn Change in bowel habits Nausea Female Reproductive Vaginal discharge Hot flashes Vaginal itching Irregular menses Male Reproductive Difficulty with erection Genitourinary Painful urination Urinary retention Muscle pain Musculoskeletal Rash Integumentary (Skin) Palpitations Breast lumps Constipation Vomiting Nipple discharge Testicular pain or swelling Frequent Urination Blood in urine Urinary urgency Joint pain Itching Joint Swelling Back pain Suspicious Mole Neurological Numbness Dizziness Slurred speech Headache Burning pain in feet Memory loss Tremor Psychiatric Anxiety Depression Insomnia Endocrine Cold intolerance Heat intolerance Excessive thirst Excessive urination Confusion Weakness Suicidal Thoughts Hair changes