Practical classes
advertisement

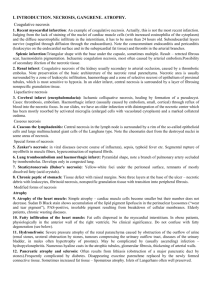
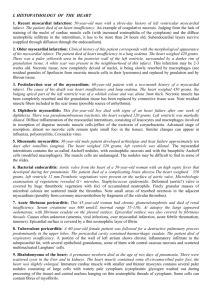
I. INTRODUCTION. NECROSIS, GANGRENE. 1. Recent myocardial infarction: An example of coagulative necrosis. Judging from the lack of staining of the nuclei of cardiac muscle cells (with increased eosinophilia of the cytoplasm) and the diffuse neutrophilic infiltrate in the interstitium, it has to be more than 24 hours old. Subendocardial layers survive (supplied through diffusion through the endocardium). 2. Older myocardial infarction: This infarction may be 2-3 weeks old. Necrotic tissue, now completely devoid of nuclei, is being slowly resorbed by macrophages (see residual granules of lipofuscin from necrotic muscle cells in their lysosomes) and replaced by graulation and by fibrous tissue. 3. Postinfarction scar of the myocardium: Necrotic muscle has been completely resorbed and the granulation tissue has been replaced by connective tissue scar. Note residual muscle fibers included in the scar tissue (possible source of arrhythmia). 4. Renal infarct: Coagulative necrosis of the kidney usually secondary to arterial occlusion, caused by a thrombotic embolus. Note preservation of the basic architercture of the necrotic renal parenchyma. Necrotic area is usually surrounded by a zone of leukocytic infiltration, haemorrhage and a zone of selective necrosi of epithelium of proximal tubules, which is most sensitive to hypoxia. In an older infarct, central necrosis is surrounded by a layer of fibrosing nonspecific granulation tissue. 5. Caseous tbc lymphadenitis: Central necrosis in the lymph node is surrounded by a rim of the so-called epithelioid cells and large multinucleated giant cells of the Langhans type. Note the cheomatin dust from the destroyed nuclei in some areas of necrosis. 6. Cerebral infarct (encephalomalacia): Ischemic colliquative necrosis, vital reaction – activated microglia (enlarged cells with vacuolated cytoplasm) so called “granular cells” (rich in lipids), healing by formation of a pseudocyst. Causes: thrombosis, embolism. Hemorrhagic infarct (usually caused by embolism, small, cortical) through reflux of blood into the necrotic focus – red encephalomalacia. Diagnostic features – leucostasis, diapedesis of leukocytes and erythrocytes, activated microglia disintegration of necrotic tissue. 7. Lung tromboembolism and haemorrhagic infarct: Pyramidal shape, note a branch of pulmonary artery occluded by trombembolus. Develops only in congested lung. 8. Chronic peptic ulcer of stomach: Chronic peptic ulcer, note three layers at the base – necrotic debris with leukocytes, layer of fibrinoid necrosis, layer of non-specific granulation tissue, then peripheral fibrosis. Thickened walls of adjacent arteries, hyperthrophy of nervous fibres and fibrosis in the basal part of wall are signs of chronicity. II. INTRODUCTION. ATROPHY, DYSTROPHY. 1. Atrophy of the heart muscle: Simple atrophy – cardiac muscle cells become smaller but their number does not decrease. Sudan B Black stain shows accumulation of the lipid pigment lipofuscin in the perinuclear lysosomes (“wear and tear pigment”), PAS-positive, insoluble pigment resulting from breakdown of cellular membranes. Elderly patients, chronic wasting diseases. 2. Atrophy of the hepatis: 3. Follicular amyloidosis of liver: AA amyloid, Congo-positive, apple green fluorescence in polarized light. Deposition mostly in the white pulp (in follicles). 4. Amyloid nephropathy: Deposition of amyloid in the walls of arteries and arterioles, less in the glomeruli and under the tubular epithelium. Both in the AA and AL amyloidosis, morphologically indistinguishable. 5. Fatty change of the liver: Intracellular accumulation of neutral triglycerides in large vacuoles in the liver cells. Various causes: hypoxia, toxic effects (mushroom poisoning, carbon tetrachloride), starvation etc. 6. Atherosclerosis: Principal morphological envents: fatty streaks, fibrous plaques, atheromas, ulceration, dystrophic calcification. Mostly intimal involvement. The section shows popliteal artery with a large atheromatous plaque. The lumen is partly filled with red thrombus (amputation spcimen, gangrene of the leg caused by arterial obstuction). 7. Fatty infiltration of the heart muscle: Fat cells dispersed in the myocardial interstitium. In obese patients, physiologically in the anterior wall of the right ventricle. No clinical significance. Do not confuse with fatty degeneration (see below). 8. Renal cell carcinoma (tumor of Grawitz): Assesment of malignancy is unreliable on morphological grounds, since malignant tumours may appear differentiated and encepsulated. Small tumours (under 2cm in diameter) considered benign (clear cell adenoma). Vascular, sometimes cystic, consisting mostly of celar cells containing glycogen. Sometimes with oxyphilic cells, sarcomatoid variant. III. INTRODUCTION. CRYSTALS, PIGMENTATION. 1. Haemosiderosis and haemochromatosis of the liver: The section of the liver tissue shows micronodular cirrhosis and severe deposition of the coarsely granular greensh-brown haemosiderin mostly in the lever cells. In some areas pigmentation can be located to lysosomes on the biliary pole of hepatocytes. There is no pigmentation of Kupffer cells and of the macrophages in the fibrous septa, which show proliferation of bile ducts and mononuclear infiltrate. Haemosiderosis – from excessive destruction of erythrocytes in the RES (e.g.after multiple blood transfudions). Haemochromatosis – from excessive absortion of iron in the intestine. 2. Biliary cirrhosis: This lesion is often called biliary fibrosis (there is no nodular transformation of the liver tissue), it appears with severe long-lasting intrahepatic bile stasis. Bile plugs in biliary capillaries between the hepatocytes in liver cell cords, bile stasis in interlobular bile ducts, formation of bile lakes. Staining of bilirubin with the Fouchet's reagent (oxidation to dark green biliverdin – sections bleache out, the staining is not permanent). 3. Haemochromatosis of pancreas: In haemochromatosis, pigment is deposited in varius organs (liver, skin, heart muscle, kidney etc.). Pigmentation of pancreas is accompanied by fibrosis with destruction of the Langerhans islets, leading to diabetes (bronze diabetes). Pearls stain (blue coloration of haemosiderin). 4. Chronic bronchitis (hypertrophic type) with emphysema (COPD), exacerbating: Lungs have emphysematous configuration with perivasal and peribronchial antrakosis. The bronchi are lined by hypertrophic mucosa with an increase in goblet cells. Bronchial walls are oedematous, thickened by hyperplastic and hypertrophic mucus-secreting glands, increase amounts of smooth muscle and capillaries. Basement membranes are also thickened. An increase in chronic inflammatory infiltration has been documented (lymphocytes, plasma cells, eosinophils). In airways there is excess mucus with small amount of polymorphonuclear leukocytes. 5. Antracosis of the lungs: Many macrophages filled with black pigment in the area of lymphatics (periarterial, peribronchial location), intraalveolar pigmented macrophages. 6. Silicosis of the lungs: Coniofibrosis with three stages: 1-stigmatization with SiO2 crystals in similar location as antracotic pigment. 2-formation of silicotic nodules, 3-massive fibrosis. Silica crystals can be observed as fine needles in polarized light. 7. Intradermal naevocellular naevus: Clinically small, variably pigmeted, slightly elevated lesion in the skin. Histological types: junctional (with nests of naevus cells in the dermo-epidermal junction. Compound naevus – with more pronouced dermal component. Dermal naevus – no junctional activity, naevus cells are only in the dermis. 8. Malignant melanoma: Increasing in frequency, relation to sunlight. Often developing on the basis of a naevocellular naevus. Variable histological composition, differences in amount of melanin. In nonpigmented variants, Fontana's silver stain for melanin and immunohistology (S100 protein, HMB45 antibody) help in establishing correct diagnosis. Superficial spreading, nodular type. Prognostic assessment according to the depth of infiltation on the dermis (Clark, Breslow grading). IV. INTRODUCTION. CIRCULATORY DISTURBANCES. PART I. 1. Hypertrophy of the myocardium: Increased size of cardiac muscle cells, enlarged rectangular nuclei or binucleated cells, ultrastructure generally preserved. In severe hypertrophy widening of the interstitium. 2. Chronic congestion of the liver: Most pronounced in the lobular centers, sometimes accompanied by centrilobular steatosis and zonal fibrosis. 3. Chronic pulmonary congestion: Mostly in the patients with chronic insufficiency of the left ventricle. Accumulation of the macrophages with haemosiderin in the cytoplasm (blue in the Pearls reaction) - brown induration. 4. Red (stagnation) thrombus: Most often in veins, clotted blood with all its constituents, red colour from the presence of numerous red blood cells. 5. Mixed (stratified) thrombus: Layers of fibrin with blood platelets alternating with layers of whole clotted blood. Note old, mostly resorbed myocardial infarction with formation of an aneurysm filled with the thrombus (effect of slow and turbulent flow of blood). 6. Organising thrombus: Cross section through popliteal vessels (Weigert's elastica stain). The artery shows signs of atherosclerosis, the vein is blocked by a red (stagnation) thrombus with signs of organization (ingrowth of fibroblasts, capillaries). 7. Organised thrombus: 8. Recanalised thrombus: The fusion of capillaries in the granulation tissue during the process of organisation. Anastomosis of the vascular lumina proximal and distal to the occluded segment. Functionally insufficient, often complicated by re-thrombosis. Popliteal vein affected, note the normal structure of popliteal artery. Weigert's elastica stain. V. INTRODUCTION. CIRCULATORY DISTURBANCES. PART II. 1. Lung thrombembolism and haemorrhagic infarct: Necrotic area is of pyramidal shape, note the branch of pulmonary artery occluded by thrombembolus. Infarct develops only in congested lung. 2. Renal infarct: Pyramidal shape, central coagulative necrosis with a layer of leukocytic infiltration and haemorrhage at the periphery. Heals by formation of scar. Causes: Arterial occlusion, most frequently by arterial thrombembolism. 3. Fat embolism: Many fat droplets (Sudan III on frozen sections) in lung capillaries and arterioles. Most frequently after trauma associated with fracture of long bones, when fat droplets are released from bone narrow. 4. Atherosclerosis: Principal morphological envents: fatty streaks, fibrous plaques, atheromas, ulceration, dystrophic calcification. Mostly intimal involvement. The section shows popliteal artery with a large atheromatous plaque. The lumen is partly filled with red thrombus (amputation specimen, gangrene of the leg caused by arterial obstuction). 5. Polyarteritis nodosa: Systemic necrotizing vasculitis of small or medium-sized muscular arteries, preferentially at vessel bifurcations, resulting in microaneurysm formation, aneurysmal rupture with hemorrhage, thrombosis, and, consequently, organ ischemia or infarction. Histologically, transmural inflammation of the arterial wall...mixed inflammatory infiltrate (neutrophils, eosinophils and mononuclear cells), deposits of fibrin, thrombus in the lumen. Spares pulmonary circulation. 6. Erdheim's cystic medial necrosis: Fragmentation and separation of the elastic fibers of the media by small cystic spaces filled with abundant basophilic ground substance (acid mucopolysaccharides). Multifocal laminar splitting of the media. May lead to dissection. Frequently accompanies Marfan syndrome. 7. Syphilitis aortitis: Vasa vasorum of adventitia surrounded by lymphoplasmocellular inflammatory infiltrate resulting in the narrowing of their lumina, and, consequently, ischemic injury of the aortic media (obliterative endarteritis). Patchy loss of the medial elastic fibers and muscle cells, followed by inflammation and scarring. Aortic aneurysm may develop. Tertiary stage of syphilis. VI. INTRODUCTION. NON-SPECIFIC INFLAMMATION. 1. Catarrhal enteritis: Note oedema of the interstitium with detachment of the superficial epithelium, also increased number of goblet cells. There is some inflammatory infiltrate with neutrophils and eosinophils in the mucosal stroma. 2. Suppurative leptomeningitis: Leptomeninges and subarachnoid space are filled with neutrophils. Cortical oedema. Healing by absorption of the infiltrate and fibrosis (scar...epileptic focus, hydrocephalus). 3. Bronchopneumonia: Acute inflammation of the walls of the bronchi and bronchioles which then spreads to the adjacent alveoli. Various etiologic agents. There is an inflammatory exudate in the alveoli, often with numerous neutrophils and sparse fibrin. 4. Absceding pneumonia: Acute suppurative inflammation associated with the destruction of the tissue. Acute abscess: irregular shape, no capsule. Chronic abscess: regular shape, capsule (pyogenic membrane). Can be either of bronchogenous, hematogenous or lymphogenous origin. 5. Septicopyaemia - myocardial abscesses: Focal accumulation of the neutrophils within the myocardium, necrosis of isolated myocytes adjacent to the abscess. 6. Acute ulcerophlegmonous appendicitis: Note segmental mucosal ulceration and diffuse neutrophilic infiltrate in all layers of the wall (best seen in the muscularis) - phlegmon. 7. Fibrinous pericarditis: Fibrinous exudate over the pericardial surface with ingrowth of nonspecific granulation tissue resulting in fibrosis. Possibile outcomes: constrictive pericarditis, dystrophic calcification of the newly formed connective tissue. 8. Lobar pneumonia: Alveoli are completely filled with fibrinous exudate, a meshwork of fibrin with admixture of leukocytes. If not absorbed, the exudate is organized by granulation tissue with subsequent fibrosis (carnification). 9. Rheumatismus nodosus: Central eosinophilic (fibrinoid) necrosis with a rim of palisading histiocytes. Disperse lymphocytic infitrate can also be seen. 10. Fibrocartilaginous perisplenitis: The splenic capsule is thickened by the newly formed, relatively acellular hyaline eosinophilic mass, grossly resembling cartilage. 11. Carnification of lung: Complication of healing of lobar pneumonia. Irreversible filling of alveoli with connective tissue. 12. Chronic cholecystitis: Gallbladder is contracted, adheres to liver, contains number of stones. The wall is thickened, whitish, firm. Scattered chronic inflammatory infiltrate in the thickened mucosa focally forms lymphatic follicles. Mucosa is atrophic with smoothened folds. VII. INTRODUCTION. SPECIFIC INFLAMMATION. 1. Tuberculosis of the lung: 2. Tuberculosis of the lung, cavity (cavitary tuberculosis): Cavitary TB involves the upper lobes of the lung. The bacteria cause progressive lung destruction by forming cavities, or enlarged air spaces. This type of TB occurs in reactivation disease, rarely, it can occur soon after primary infection. 3. Caseous pneumonia: Caused by a porogenous spread of TB bacteria. Diffuse extensive cellular infiltration that undergoes caseation (necrosis with chromatin dust and scattered Langhans cells. Affects large areas of lungs. If the regions gain access to the bronchi, the necrotic material is coughed up and cavities develop. 4. Miliary tuberculosis of the lung: If TB bacteria gain entry to the bloodstream from an area of damaged tissue they spread through the body and set up many foci of infection, all appearing as tiny white tubercles (with central necrosis and a peripheral rim of epitheloid and Langhans cells) in the tissues. Severe form. Its name comes from a distinctive pattern seen on a chest X-ray of many tiny spots distributed throughout the lung fields with the appearance similar to the millet seeds. 5. Congenital syphilis, liver: "Flint stone liver." Note the proliferation of the interstitial connective tissue surrounding individual liver cells. High number of spirochetes can be visualized by a special stain. 6. Syphilitic gumma in the liver: Gumma is a typical morphological lesion of the third stage of syphilis. Note the radiating retracting scar around the lobular centre with incomplete necrosis. Location of the gumma may be variable, most commonly in the liver. 7. Syphilitic aortitis: Vasa vasorum of adventitia surrounded by lymphoplasmocellular inflammatory infiltrate resulting in the narrowing of their lumina, and, consequently, ischemic injury of the aortic media (obliterative endarteritis). Patchy loss of the medial elastic fibers and muscle cells, followed by inflammation and scarring. 8. Congenital syphilis, liver: See no. 5. 9. Rhinoscleroma: Large histiocytes with pale vacuolated cytoplasm (Mikulicz cells) containing mucinous substance from the capsules of the bacteria, intermingled with plasma cells and newly formed capillaries at the periphery. IX. INTRODUCTION. GENERAL ONCOLOGY. 1. Branchiogenic cyst: Lateral cyst of the neck, the lining is formed by cuboidal or by columnar epithelium, the cyst is filled with transparent fluid. Aggregates of lymphoid tissue in the wall of the cyst. 2. Parasitic cyst: cystic cavities in the liver with chitin remnants of parasites, rare presence of scolexes and of hooks. Eosinophilia. 3. Fibrocystic disease: Several histological types: adenosis- enlargement of lobules with many acini, structurally normal, sclerosing adenosis- lobular proliferation, proliferate both the epithelium and myoepithelial cells, increased amount of collagen between the glandular structures, epithelial hyperplasiaproliferation of epithelium that may lead to obliteration of the lumen, relationship to cancer. papillomatosis papillary proliferation into the lumen of dilated ducts or cysts, cysts- dilation of acini and of terminal ducts, usual with cuboidal or with flat lining, apocrine metaplasia - the lining of the cysts resembles that of apocrine sweat glands - eosinophilic cytoplasm (so-called pink-cell metaplasia), fibrosis - association with hormonal dysbalance. 4. Myoadnomatous hyperplasia of prostate: hormonal effect, leading to hyperplasia of both glands (with bi-layered epithelium) and the interstitial connective tissue with smooth muscle cells. 5. Foreign body giant cell granuloma: Schloffer’s tumour giant cell reaction around stitches. 6. Mola hydatidosa: Oedema of the chorionic villi, trophoblastic hyperplasia, risk of development of choriocarcinoma. Increased level of HCG. Two types: complete mola(no fetus, karyotype 46XX). partial mola (triploid karyotype, fetus may develop). 7. Polyposis of the intestine: several types of polyps: adenoma tubular or villous, may undergo malignant transformation, inflammatory polyp, hamartomatous polyp (juvenile) (Peutz-Jeghers’ disease) metaplastic polyp- not malignant. Malignant epithelial polyp - the stalk should always be examined! 8. Paget’s carcinoma: Large pale cells in the epidermis of the nipple. Associated with intraductal or infiltrating carcinoma of the breast. 9. Comedocarcinoma: Debris of necrotic cells in the lumen of ducts, intraductal non-invasive carcinoma. 10. Bowen’s dermatosis: A variant of intraepithelial squamous cell carcinoma. Varied cellular composition with giant cells, base membrane is not broken. Note cellular atypias and increased mitotic activity and intact basal membrane. Sometimes present in sun exposed areas of solar keratosis. The presence of HPV (type 16, 18) was detected in lesions in anogenital region. 10% risk of development of invasive squamous cell carcinoma. X. INTRODUCTION. MESENCHYMAL TUMOURS. HEMATOPATHOLOGY. Fibroma: This a benign encapsulated tumour with ubiquitous localization. It consists of uniform slender spindle cells with minimal mitotic activity. 1. Leiomyoma: Originates from smooth muscle tissue, consists of spindle cells in fascicular arrangement. Most frequently in uterus, the most frequent uterine neoplasm. Uterus myomatosus - multiple uterine leiomyomas. Whitis, circumscribed tumour, often with secondary fibrotic changes. 2. Capillary haemangioma: One of the most frequent tumours of the skin - naevus flammeus. Consists of capillaries lined by swollen endothelial cells. May not be well circumscribed, but does not cause any destruction of the surrounding tissue. 3. Cavernous haemangioma: Most frequent in the liver, usually in subcapsular location. Note multiple fresh and organizing thrombi in the wide vascular spaces. May cause bleeding on liver biopsy. Chondroma: Originates from hyaline cartilage. Multiples chondromas – Ollier’s disease. Location inside a bone - enchondroma, outside - ekchondroma. Cartilaginous exostosis - hyperplastic process, resembles true neoplasm. 4. Gigant cell tumour of the bone: Also called giant cell tumour or brown tumour (haemosiderin deposits). In younger patients (3rd and 4th decade), distal femur and proximal tibia, highly vascular, predominant spindle pulpy cells with scattered multiple multinucleated giant cells. Osteolytic aggressive growth, but almost always benign. Healing after extirpation but recurrence is also possible. 5. Hodgkin's lymphoma: Normal architecture of this lymph node is replaced by confluent foci of pale vells and many eosinophils, among which there are scattered diagnostic binucleated Reed-Sternberg cells and more numerous but slightly less diagnostic mononuclear Hodgkin cells, both with conspicuous large amphophilic nucleoli (mixed cellularity). 6. Chronic lymphadenosis, liver: In chronic lymphadenosis, the infiltrating cells typically accumulate in portal fields, which appear enlarged. Liver sinusoids are relatively free of tumour cells. Chronic myelosis, liver: Infiltration of liver tissue with characteristic accumulation of the neoplastic cells in the sinusoids, less infiltration in the portal fields. Multiple myeloma: This femoral bone marrow (without bone trabeculae) is heavily infiltrated by neoplastic plasma cells which in one part of the section form a compact nodule. The cell resemble normal nonneoplastic plasma cells - plasmocytic type of multiple myeloma. XI. INTRODUCTION. BENIGN AND MALIGNANT EPITHELIAL TUMOURS. 1. Polyposis of the intestine: several types of polyps: adenoma tubular or villous, may undergo malignant transformation, inflammatory polyp, hamartomatous polyp (juvenile) (Peutz-Jeghers’ disease) metaplastic polyp- not malignant. Malignant epithelial polyp - the stalk should always be examined! 2. Serous cystadenoma of the ovary: Unilocular or multilocular cysts with papillary proliferation containing serous fluid. Borderline tumours - less regular, multiple shorter, branching papillae. 3. Pleomorphic adenoma: Previously called myxochondroepithelioma for its microscopical appearance (only the epithelial and the myxoid structures are visible on our slides). Epithelial structures, with locally variable differentiation, cells form stripes, glandular and solid structures. The tumour is benign but poorly outlined, without capsule, hence the tumour may recur when not completely removed). 4. Adenoid cystic carcinoma: Characteristic arrangement of cells surrounding small "lumina" (actually oedematous stroma). Typical perineural spread and frequent haematogenous metastases, surgical excision of the tumour difficult. 5. Adenocarcinoma, carcinoma of glandular epithelium: Mostly with tubular arrangement, production of mucin (PAS positivity). 6. Dissociating carcinoma: Another form of low differentiated glandular carcinoma with tumour cells scattered in abundant connective tissue stroma - grossly diffuse growth, hard tumour tissue (scirrhus, scirrhotic carcinoma). Paget’s carcinoma: Large pale cells in the epidermis of the nipple. Associated with intraductal or infiltrating carcinoma of the breast. Bowen’s dermatosis: A variant of intraepithelial squamous cell carcinoma (carcinoma in situ). Varied cellular composition with giant cells, basement membrane is not broken. Note cellular atypias, increased mitotic activity and intact basal membrane. Sometimes present in sun exposed areas of solar keratosis. The presence of HPV (type 16, 18) was detected in lesions in anogenital region. 10% risk of development of invasive squamous cell carcinoma. 7. Keratinizing squamous cell carcinoma: 8. Basal cell carcinoma: Malignant, with aggresive growth, but never develops metastases. Solid arrangement of cells resembling cells of the basal layer of epidermis. Margin of the lesion should always be examined. Copmplete excision with margins free of tumour = cure. 9. Small cell carcinoma: Highly malignant, the second most frequent form of lung cancer. Small cells with scanty cytoplasm and round to spindle nuclei ("oat cell cancer"). Immunohistology and electron microscopy must be used to differentiate the tumour from other small round cell tumours (neuroendocrine granules). 10. Papillocarcinoma of the urinary blader: Compare with slide l, less differentiated, thicker layers of epithelium, cellular atypia, higher number of mitoses, invasive growth. XII. INTRODUCTION. NEUROECTODERMAL TUMOURS. MIXED TUMOURS. TERATOMA. THE DISEASES OF THE TROPHOBLAST. 1. Neurinoma: Benign tumour, dangerous location in the pontocerebellar angle (8th cranial nerve). Originates from the Schwann cells, two main histological patterns: Antoni A- spindle cells with palisading nuclei, Antoni B- irregular arrangement with larger cells with clear cytoplasm. Usually attached to the surface of a nerve. Synonym: schwannoma. 2. Neurofibroma: Despite its benign behaviour, it is usually less circumscribed than schwannoma. Located inside the nerve. On histology, neurofibroma consists of a mixture of Schwan cells and fibroblasts. Irregular arrangement of fascicles with wavy nuclei, sometimes storiform pattern. 3. Pigmented nevus: several forms according to its maturity: junctional nevus- accumulations of proliferating melanocytes at the dermo-epidermal junction, compound nevus- still showing junctional activity, simultaneously nests of nevus cells in the dermis, (intra)dermal nevus- without junctional activity, sometimes signs of regression at the base with fibrosis. Benign, however, risk of malignant transformation into melanoma. 4. Malignant melanoma (melanoblastoma): Consists of more or less pigmented melanoblasts. In nonpigmented cells premelanosomes are found on electron microscopy. Several patterns of growth - superficial spread in the epidermis or vertical ingrowth into dermis. Classification of Clark, of Breslow - prognostic importance of histological assessment. One of the most malignant neoplasms with unpredicatable period of latency before the manifestation of metastases in all organs. Astrocytoma: Progression of malignancy from differentiated astrocytoma through anaplastic astrocytoma to glioblastoma. Signs of malignancy - cellular pleiomorphism, necroses, neovascularization. Sometimes formation of cysts. Gemistocytic astrocytoma - consists of plump enlarged astrocytes. Glioblastoma multiforme: Marked cellular pleiomorphism, scattered necroses with palisading nuclei, vascular proliferation (compare to astrocytoma). Malignant. 5. Pheochromocytoma: Benign tumour arising in medulla of adrenal glands, with paroxysmal, less frequently continuous hypertension. 90% of tumours sporadical, 10% associated with the MEN II a, b syndrome. Highly vascular, with large and scattered bizzare giant cells. IHC: chromogranin positivity. Ultrastructurally catecholamine granules in the cytoplasm, secreting epinephrine and norepinephrine. 6.Teratoma of the ovary: Various grades of differentiation: differentiated (mature teratoma) with more differentiated tissues of several germ layers, even with organoid structures (usually benign), and undifferentiated (immature teratoma, teratocarcinoma) with less differentiatedd structures - usually highly malignant. May contain embryonic structures (trophoblast, yolk -sac type of epithelium). The most frequent form of mature teratoma is ovarian dermoid cyst. 7. Choriocarcinoma: Malignant trophoblastic tumour with pronounced invasive growth into blood vessels, frequent necroses. Teratogenic or of placental origin (hydatidiform mole). Hematogenous metastases into lungs, sometimes brain. Produces chorionic gonadotrophin (HCG)- biochemical diagnosis and control. Tumours of placental origin are sensitive to chemotherapy. By contrast, relatively poor response to chemotherapy in tumours that arise in the gonads. XIII. INTRODUCTION. ETHIOLOGIC PATHOLOGY. 1. Cytomegaloviral sialoadenitis: An example of predominantly alterative infiltration, mostly in small infants (cytomegaloviral infection in HIV patients usually involves other organs than the salivary glands). Typical basophilic intranuclear inclusions in the markedly enlarged ductal lining cells. 2. Candidiasis: 3. Aspergillosis of the lung: Secondary involvement, suppurative and non-suppurative forms. Aspergilloma- accumulation of hyphae in a preformed cavity. Branching, septated hyphae, diagnostic conidial heads with conidia. 4. Non-suppurative interstitial pneumocystis pneumonia: Alveolar septa thickened by infiltration with predominantly plasmocytic inflammatory infiltrate. Foamy masses filling the alveoli - pneumocystis organisms with their capsules. Sensitive to UV light, frequent in HIV patients. 5. Actinomycosis: An opportune infection, suppurative inflammation with formation of diagnostic actinomycotic grains sometimes with an eosinophilic rim (Splendor-Hoeppli phenomenon). Grossly sometimes resembles tumour - actinomycoma. Cervicofacial, abdominal forms. 6. Toxoplasmosis of the brain: Accumulation of trophozoits in the cells with formation of pseudocysts, in slower course of the disease parasitic cysts (muscle, brain), with innumerable parasites. 7. Ulcerophlegmonous appendicitis: Shallow mucosal ulceration, diffuse infiltration of the wall by polymorphonuclear leukocytes. Serosal surface covered by fibrin. Compulications: gangraene, circumscribed or diffuse peritonitis. Appendicitis oxyurica: parasitic eggs in the lumen, numerous eosinophils in the inflammatory infiltrate.