Gastroenterology (Medical Abdo) Notes
advertisement
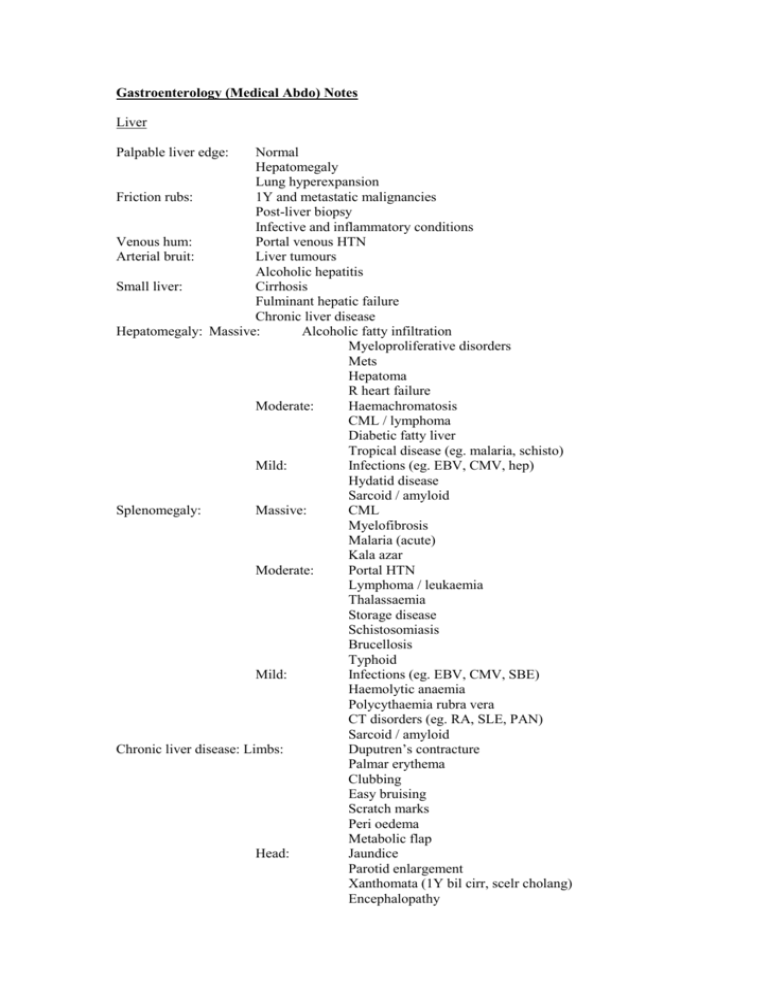
Gastroenterology (Medical Abdo) Notes Liver Palpable liver edge: Normal Hepatomegaly Lung hyperexpansion Friction rubs: 1Y and metastatic malignancies Post-liver biopsy Infective and inflammatory conditions Venous hum: Portal venous HTN Arterial bruit: Liver tumours Alcoholic hepatitis Small liver: Cirrhosis Fulminant hepatic failure Chronic liver disease Hepatomegaly: Massive: Alcoholic fatty infiltration Myeloproliferative disorders Mets Hepatoma R heart failure Moderate: Haemachromatosis CML / lymphoma Diabetic fatty liver Tropical disease (eg. malaria, schisto) Mild: Infections (eg. EBV, CMV, hep) Hydatid disease Sarcoid / amyloid Splenomegaly: Massive: CML Myelofibrosis Malaria (acute) Kala azar Moderate: Portal HTN Lymphoma / leukaemia Thalassaemia Storage disease Schistosomiasis Brucellosis Typhoid Mild: Infections (eg. EBV, CMV, SBE) Haemolytic anaemia Polycythaemia rubra vera CT disorders (eg. RA, SLE, PAN) Sarcoid / amyloid Chronic liver disease: Limbs: Duputren’s contracture Palmar erythema Clubbing Easy bruising Scratch marks Peri oedema Metabolic flap Head: Jaundice Parotid enlargement Xanthomata (1Y bil cirr, scelr cholang) Encephalopathy Chest: Abdo: Portal HTN: Gynaecomastia Spider naevi (>5 abnormal) Dilated superficial veins Ascites Splenomegaly Hepatomegaly Splenomegaly Venous collaterals Ascites Murphy’s sign: Inability to deep inspire due to RUQ pain = acute cholecystitis: sensitivity 97%, specificity 50% Kehr’s sign: Severe L shoulder tip pain esp when lying supine = haemoperitoneum Cullen’s sign: Periumbilical ecchymoses = retroperitoneal haemorrhage Grey-Turner’s sign: Flank ecchymoses = retroperitoneal haemorrhage McBurney’s sign: Tenderness 2/3 distance from umbilicus to R ASIS = appendicitis Iliopsoas sign: AP on extension of R hip = appendicitis: 16% sensitivity, 95% specificity Obturator’s sign: AP on internal rotation of flexed R hip = appendicitis Rovsing’s sign: RLQ pain and palpation LLQ = appendicitis Heel-drop sign: RLQ pain on dropping heels to ground when on tiptoe = appendicitis: 93% sensitivity Cough test: AP after cough = appendicitis: 95% sensitivity Gastroenteritis 3+ abnormally loose BM’s over 24hrs Sx: vomiting ++ if pre-formed toxin; prominent AP if invasive Doses: Norfloxacin 400mg (10mg/kg) PO BD 5/7 Alternative: ciprofloxacin, cotrimoxazole, ampicillin - E coli, Campylobacter, Yersinia, salmonella, shigella - Cholera Doxycycline Alternative: tetracycline Metronidazole 400mg (10mg/kg) PO TID 7-10/7 Vancomycin 125-250mg PO QID 10/7 Erythromycin 500mg (10mg/kg) PO QID 5/7 MO Incbn DOA Source - C diff, giardia - Severe C diff - Campylobacter Specific symptoms Antibiotics? Pre-formed toxin Bacillus cereus 1-6hrs <24hrs Staph aureus 1-6hrs <24hrs Rice, cereal, soup, veggies, meats, pasta Cold foods, sweetened dairy products Vomiting ++ May be delayed onset form At 8-18hrs, AP + D but little V Vomiting ++ diarrhoea, AP dehydration No Many raw foods 0157:H7 Shiga bloody watery stools without WBC Debatable TTP, HUS Norfloxacin if severe (but may CAUSE HUS) No Post-formed toxin E Coli (20-75%) (Most common cause of traveller’s diarrhoea) Clostridium perfringens (25% all bacterial) Vibrio cholera (0-30% travellers) C difficile Toxins A and B; secretory Varies (usually 1-5/7) Dayswks 6-12hrs <24hrs Hrs-days 2-7/7 7-10/7 after ABx Meat and poultry, soil, manure, sewage Shellfish Antibiotics Clindamycin Ampicillin Amoxicillin Cephalosporin 1-25% colonisation in hospitalized patients Diarrhoea, AP Severe rice water diarrhoea, headache, N+V Severe: Pseudomembranous enterocolitis (RF inc recent ABx, recent GI surgery, co-morbidities, chemo, old age) or any 2 of: >60yrs; T >38.4, alb <2.5mg/dL; WBC >15 YES NEEDS ABX: Metronidazole Vancomycin if severe Fulminant (3-8%): Toxic megacolon, systemic manifestations (eg. incr WBC, hypotension, MOF, anascara) Listeria Doxycycline if in 1st 48hrs Stop offending ABx Days wks Meat, cheese 1-3% get toxic megacolon or perf Relapse in 10-25% Flu like meningitis, septicaemia, miscarriage, prem birth Emergency colectomy if fulminant Bad if pregnant / neonate / immunosupp / elderly Enteroinvasive Salmonella (0-33% travellers) 12-24hrs Up to 3/52 Dairy, eggs, raw meat, raw veggies Can cause bloody diarrhoea, systemic illness In children can cause osteomyelitis, meningitis If septicaemia / immunocompromised / infant / elderly / multiple co-morbidities Norfloxacin if severe IV ceftriaxone if <3/12 Shigella 2-30% travellers (also release cyto, neuro and enterotoxins) 12-96hrs 4-7/7 Infected foodhandler or water; poor sanitation; traveller; child care centres Poultry, milk, pets with diarrhoea Campylobacter Jejuni (3-17% travellers) 2-5/7 2-5/7 E coli (0-6% in travellers) Varies (usually 1-5/7) Dayswks Many raw foods Vibrio parahaemolyticus Yersinia enterocolitica 12-24hrs 1-7/7 Shellfish Mod severity gastro 3-7/7 1-21/7 Pork and chicken Bloods and pus in stool, severe AP (may mimic appendicitis) May cause reactive arthritis, erythema nodosum, scarlatiform rash, GN, conjunctivitis, hepatic/splenic abscess, meningitis, osteomyelitis Risk of bacteriaemia and metastatic infection if immunosupp Rapid deterioration with fever, hypoT, V+D, haemorrhagic bullous rash necrotic ulcers If immunocomp / systemically unwell Cotrimoxazole / ciprofloxacin Vomiting in children, diarrhoea in adults No Gastro No Can cause bloody / mucusy diarrhoea, systemic illness Bloody stools without WBC Profuse watery diarrhoea Metronidazole + iodoquinol Vibrio vulnificus Dysentry: Bloody mucusy stools and tenesmus, systemic illness Seizures, perf, HUS, Reiter’s syndrome, fulminant toxic encephalopathy YES NEEDS ABX: As public health measure Can cause bloody diarrhoea, systemic illness; can cause severe AP with little diarrhea Can cause reactive arthritis, GBS, seizures, Reiter’s syndrome, neonatal sepsis Bloody diarrhoea and severe AP, systemic illness If severe / prolonged / food-handler Erythromycin / norfloxacin Norfloxacin if severe IV ceftriaxone if <3/12 Debatable Norfloxacin / cotrimoxazole / amox if severe Broad spectrum ABx Viral 12-48hrs 12-60hrs 24-72hrs Up to 1/52 Shellfish; maybe infected food handler Food-handler / water Entamoeba histiolytica 2-4/52 Wks – mths Food handler / water Cryptosporidium 1-12/7 2-21/7 Giardia lamblia 1-3/52 >1/52 diarrhoea Food handler / water Food-handler / water History of rural hiking; contaminated drinking water Norovirus (most common viral cause) Rotavirus (most common cause in children) (0-36% in travellers) Parasitic Mild; flatulence, sulphurous belching, bloating, abdo cramps; trophozoites and cysts in stool Pale, foul, greasy poo for >1/52 If severe / immunocompromised YES NEEDS ABX: Metronidazole 2g (child: 30mg/kg) OD 3/7 Pathology Invasive cell damage and incr secretion 1) Decreased intestinal absorption – healthy SI absorbs 75% of fluid, LI absorbs 90%; usually <100ml/day lost in stool; fluids absorbed passively with Na and actively with Glu; Large vol suggests SI pathology, small vol suggests LI a. Enterotoxins: block Na absorption, stimulate Na secretion net loss of fluid. Don’t affect Glu absorption, therefore add Glu to rehydration fluid b. Inflammation / ischaemia – affect villi responsible for absorption 2) Increased osmotic load a. Draws fluid into lumen b. Will be associated with certain foods 3) Increased intestinal secretion a. Unopposed crypt secretion – unaffected by inflammation b. Persists with fasting 4) Abnormal intestinal motility a. Occurs in IBS, short gut syndrome RF’s: achlorhydria, bowel stasis, immunodef, recent ABx Traveller’s Diarrhoea – usually don’t need ABx as usually self-limiting; treat with norfloxacin 800mg (20mg/kg in child) PO single dose, or azithromycin 1g (child 20mg/kg) PO single dose Usually due to consumption of contaminated food and drink; educate about boiling water etc… Bacteria (80%) Protozoa Viral E coli (Mexico, S America) Salmonella (S Asia) Campylobacter (S Asia) Shigella (S Asia) Giardia Cryptosporidium Entamoeba histolytica Rotavirus, norovirus Immunocompromised causes: cryptosporidium, microsporidium, isospora, CMV Reiter syndrome: arthritis + conjunctivitis + urethritis/cervicitis = Salmonella, Shigella, Campylobacter, Yersinia Investigations Stool Microscopy and culture – look for bacteria; low yield; indicated if child, toxic, dehydrated, illness >3/7, blood/pus in stool, immunocomp Cysts, ova, parasites – if traveler, >7/7 illness; may need multiple samples, as again low yeild Wright stain for fecal leucocytes – if +ive, more chance of invasive pathogen Analysis for C. diff toxin – if recent ABx or hospitalisation Electron microscopy, PCR, ELISA or latex agglutination to look for virus or C diff toxins; may need multiple samples Colonscopy: yellow plaques in C diff pseudomembranous colitis, usually in R colon; not routinely required to make diagnosis AXR If recent surgery Drug levels, TFT’s Non-infectious causes of diarrhoea: IBS, mesenteric ischaemia, thyroid storm, toxins (esp. cholinergic), adrenal insufficiency, drugs (eg. erythromycin, laxatives, antacids, oral contrast, lactulose, sorbitol, NSAIDs), GI bleed, acute radiation syndrome If fecal evidence on inflammation and rule out Shigella, Salmonella, Campylobacter, C diff and Entamoeba histolytica – then need to consider IBD Trt Mild Mod Drink 30-50ml/kg over 4 hrs Drink 100ml/kg over 4 hrs Avoid chewing gum, raw fruit; avoid sugary drinks (hyper-osmolar and no electrolytes incr fluid losses); avoid caffeine (incr cAMP worsened diarrhea); avoid milk (transiently lactose intolerant) Attempt early solid food intake Educate about food hygiene. Give sick note if work in health care / with food. Cipro 500mg BD for 1/52 has been shown to shorten duration of infectious diarrhea 2Y to bacteria Hepatitis Acute = self limited liver inj <6/12 Chronic = diagnosed on pathological criteria, >6/12 Incubation pre-icteric icteric convalescent ALT > AST (AST > ALT in cirrhosis); ALP normal or mild incr A Incubation / Transmission 2-6/52 Fecal-oral (contaminated food and water, overseas travel) Rarely parenteral Reportable disease B 2/12 Parenteral 15% risk of transmission with sex 2-30% risk seroconversio n in needlestick Acute infection Fulminant / Carrier / Chronic Prodrome for 1/52 mild-mod jaundice, N+V+AP, tender hepatoM, dark urine, clay coloured stools recovery over 1/12 Extrahepatic: vasculitis, ARF, pancreatitis, transverse myelitis, seizures, aplastic anaemia Infectious: from 2/52 before jaundice 1/52 after onset jaundice 20% get relapse; >80% children asymptomatic Serum Markers Treatment IgM-anti HAV = acute infection; detectable 1st at onset of Sx, 3/52 postexposure; remains for 36/12 Supportive IgG-anti HAV = past infection and immunity; peaks 3/52 after IgM Hep B than Hep A HAV RNA = in stool/plasma for most of asymptomatic period; disappears soon after onset of Sx Current acute infection: HBsAg HBeAg IgM-anti HBcAg Hep B DNA HBsAg = acute, detectable 1st in preicteric phase; may have normalized if late presentation; carrier if present on 2 occasions >6/12 apart IgM-anti HBcAg = acute; high infectivity HBeAg = acute and phase 2 chronic (usually decreases in 3-4/52); high infectivity; marker of viral replication Co-infection: HBsAg HBeAg IgM-anti HBcAg Hep B DNA Anti-D virus Fulminant: <1% Chronic: No Carrier: No Acute = HBsAg and HBeAg, IgM-anti HBcAg Symptomatic acute infection in 30%; Arthritis, fever, skin eruption in preicteric phase; most common hepatitis cause of ALF; mortality higher in ALF caused by Give inactivated vaccine if contact with case, within 2/52 exposure (nearly 100% effective) Give NPIG if <1yr, immunocomp, CLF, CI to vaccine (80-90% effective) Supportive Trt if infected and abnormal LFT’s or high HBV DNA levels (likely in acute, phase 2 + 4 chronic) – entecavir, lamivudine, tenofovir etc… Vaccine available (HBsAg) Fulminant: 0.1-0.5% (mortality rate 80%) Chronic: 5-10% (1-3% healthy adults, 5-10% immunocomp, 90% neonates) = HBsAg >6/12, IgG-anti HBcAg, maybe HBeAg, anti-HBeAg cirrhosis and hepatocellular Ca; shortens life span in 45% men, 15% women Phase 1: immune tolerance; 20-40yrs; normal ALT; high levels viral replication; no trt Phase 2: immune clearance with immune response; symptomatic in 30%; hepatitis, incr ALT fibrosis with repeated episodes; cirrhosis in 30-40% Phase 3: immune control immune response suppresses replication decr inflamm, ALT normalises; 5-10%/yr phase 2 become phase 3; assoc with HBeAg seroconversion (anti-HBeAg develops, decr HBeAg); hepatitis stops; may reactivate at any time Phase 4: immune escape; recurrence of hepatitis, fibrosis; virus mutates and stops making HBeAg; incr ALT; 8-10%/yr develop cirrhosis Chronic active Hep B: HBsAg HBeAg IgG-anti ABcAg Hep B DNA If non-immune exposed, give anti-HBsAg within 1/52 (75% effective) Previous resolved Hep B: Anti HBsAg Anti-HBeAg IgG-anti ABcAg Carrier: IgM-anti HBcAg Vaccinated: Anti-HBsAg IgG-anti ABcAg = chronic, previous infection Anti-HBeAg = phase 3 chronic; low infectivity; indicates viral replication as ceased HBV DNA: high infectivity, used for monitoring response to trt Carrier: 1-10% = HBsAg Accounts for 90% chronic infections C 2/12 D Parenteral 80% prevalence in IVDU 15% rate of transmission with sex (rare) 10% unknown source <2% seroconvert with needlestick 4-7/52 Parenteral Sexual rare Usually IVDU Only occurs in patients with acute/chronic HBV 5% HBV IgG-anti HBsAg = immunity and recovery Acute = HCV RNA: Pre-icteric non-specific; usually asymptomatic (Sx in 15-20%) icteric phase for 12/52; Extrahepatic Sx in 75%: arthralgia, paraesthesia, myalgia, pruritis, sicca spontaneous resolution in 30-50% Fulminant: Rare HCV RNA = acute, detectable 1st within 1-2/52 exposure IgG-anti HCV = chronic; +ive by 3/12 usually Chronic = IgG-anti HCV: 75-85% adults; 55% children 25% develop cirrhosis over 20-30yrs; 20% cirrhotics develop hepatocellular Ca Supportive Interferon if persistently high LFT’s (effective in 1/3); peginterferon + ribavarin (effective in 50%) No vaccine / postexposure prophylaxis available Carrier: 0.2-1% Acute = HDV RNA, Ig-anti HDV: in 2-20% Co-infection – hepatitis with resolution in 80-95% Fulminant: 2-20% if super-infection Chronic = Ig-anti HDV: 5-10% if co-infection; 80% if super-infection Carrier: Low 1-10% IVDU and haemophiliacs are carriers HDV RNA = acute Co-infection = IgM-anti HDAg + IgM antiHBcAg Super-infection = IgM-anti HDV + HBsAg IgM/G-anti HDV = acute / chronic Supportive; interferon may help Otherwise as per HBV E carriers have HDV 2-8/52 Fecal-oral, water-bourne Acute = HEV Ag, IgM-anti HEV: Self-limited; 1-3% overall fatality; 5-25% mortality in pregnancy Fulminant: 20% if pregnant Chronic: No Carrier: No Virus Acute infection Chronic infection A HAV RNA IgM-anti HAV HBsAg IgM-anti HBcAg, HBeAg B C HCV RNA D HDV RNA IgM-anti HDV HEVAg = acute IgM-anti HEV = acute Supportive IgG-anti HEV = immunity Carrier No Immunity and recovery IgG-anti HAV 5-10% IgG-anti HBsAg 1-10% IgG-anti ABcAg, HBeAg (phase 2) Anti-HBeAg (phase 3) 75-85% No HBsAg 0.2-1% IgG-anti HCV 5-10% Low IgG-anti HDV Co-infection = IgM-anti HDAg + IgM antiHBcAg E Super-infection = IgM-anti HDV + HBsAg HEVAg IgM-anti HEV No IgG-anti HEV No Other causes: ETOH; non-alcoholic steatohepatitis (10-50% develop cirrhosis); drug induced (necroinflammatory eg. Paracetamol; cholestatic eg. Chlorpromazine); autoimmune Hepatorenal Syndrome Development of ARF in patient with normal kidneys in presence of preexisting A or CLF; cause unknown Type I More serious; progressive oliguria; Cr x2 in 2/52; survival without medical trt <1/12 Type II Gradual impairment of renal function Toxic Megacolon Defintion: non-obstructive colonic dilation with fever + abdo distension + severe AP + shock; distension can be segmental / total Pathophysiology: NM tone decr 2Y to transmural inflammation; abnormal if >6cm; transverse colon most commonly affected; occurs in IBD, but also in Crohn’s (also in ischaemic bowel, pseudomembranous colitis, radiation colitis, infectious colitis, Hirschsprung disease RF’s: precipitated by hypomotility agents (eg. Loperamide), Ba enema, hypoK, opiates, anticholinergics, pregnancy, enema, recent colonscopy Sx: severely ill, fever, profuse diarrhea, hypoV, incr HR, abdo distension, severe pain, tenderness and peritonitis, N+V, rectal bleeding may occur; Sx may be masked by steroids Complications: perforation, circulatory collapse, septicaemia Investigation: Bloods (FBC, U+E, glu, lipase, LFTs, cultures, ABG, ESR, CRP); XR (loss of haustra, thumb printing, air filled dilated segments of colon >6cm); CXR (for perf); ECG; scope (carries risk of perf); CT (for complications like abscess and perf); effectiveness of scope screening controversial Mng: admit if severe disease, suspected complications; response assessed by serial XR 1. IVF: as indicated 2. Analgesia 3. NG, NBM 4. Sulfasalazine: 1-4g/day; for mild-mod Mesalazine: better tolerated, equally effective, can be given PR Antibiotics: for severe disease; ampicillin / gent + clindamycin / metronidazole 5. Steroids: pred 25-50mg; hydrocort 100mg Q6h; enemas / IV / PO 6. ImmunoS: if refractory; azathioprine, ciclosporin (may avert need for OT), tacrolimus, infliximab 7. Total colectomy: if drug resistant (ie. No response in 24-48hrs) Prognosis: >30% mortality; 15yrs disease 12% risk of Ca, 20yrs 23%, 25yrs 42%, risk greatest with pancolitis