National C diff Infection Workshop
advertisement
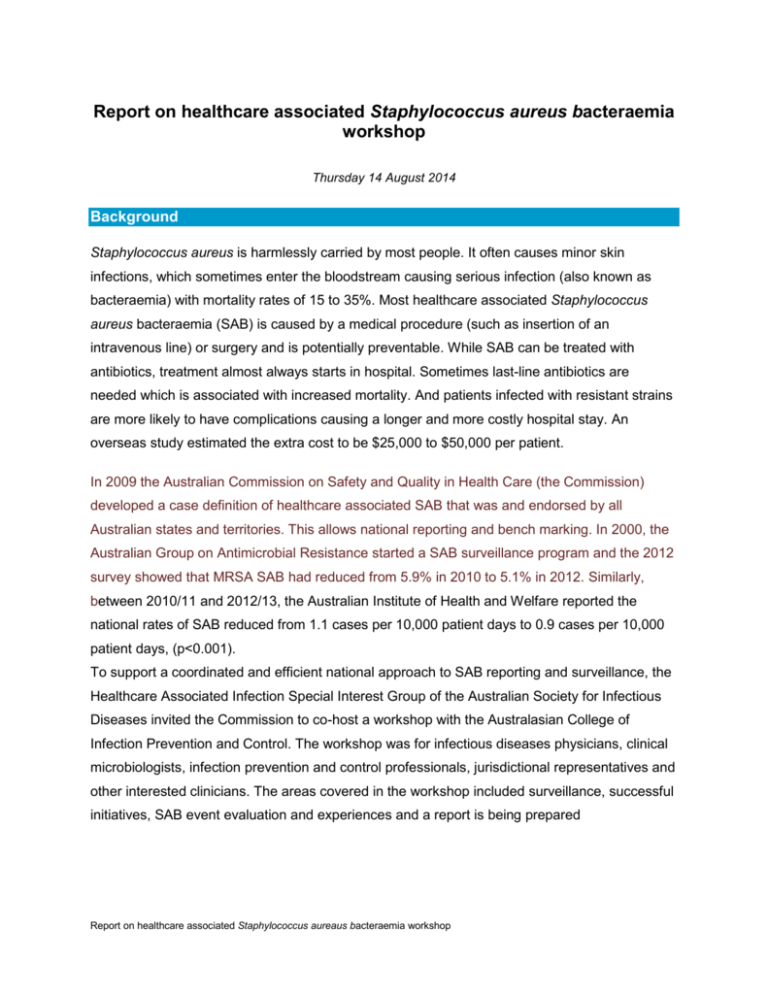
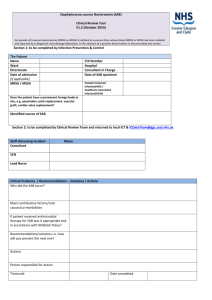
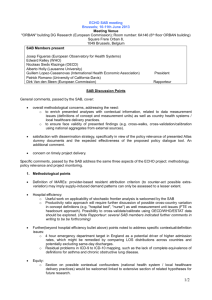
Report on healthcare associated Staphylococcus aureus bacteraemia workshop Thursday 14 August 2014 Background Staphylococcus aureus is harmlessly carried by most people. It often causes minor skin infections, which sometimes enter the bloodstream causing serious infection (also known as bacteraemia) with mortality rates of 15 to 35%. Most healthcare associated Staphylococcus aureus bacteraemia (SAB) is caused by a medical procedure (such as insertion of an intravenous line) or surgery and is potentially preventable. While SAB can be treated with antibiotics, treatment almost always starts in hospital. Sometimes last-line antibiotics are needed which is associated with increased mortality. And patients infected with resistant strains are more likely to have complications causing a longer and more costly hospital stay. An overseas study estimated the extra cost to be $25,000 to $50,000 per patient. In 2009 the Australian Commission on Safety and Quality in Health Care (the Commission) developed a case definition of healthcare associated SAB that was and endorsed by all Australian states and territories. This allows national reporting and bench marking. In 2000, the Australian Group on Antimicrobial Resistance started a SAB surveillance program and the 2012 survey showed that MRSA SAB had reduced from 5.9% in 2010 to 5.1% in 2012. Similarly, between 2010/11 and 2012/13, the Australian Institute of Health and Welfare reported the national rates of SAB reduced from 1.1 cases per 10,000 patient days to 0.9 cases per 10,000 patient days, (p<0.001). To support a coordinated and efficient national approach to SAB reporting and surveillance, the Healthcare Associated Infection Special Interest Group of the Australian Society for Infectious Diseases invited the Commission to co-host a workshop with the Australasian College of Infection Prevention and Control. The workshop was for infectious diseases physicians, clinical microbiologists, infection prevention and control professionals, jurisdictional representatives and other interested clinicians. The areas covered in the workshop included surveillance, successful initiatives, SAB event evaluation and experiences and a report is being prepared Report on healthcare associated Staphylococcus aureaus bacteraemia workshop Healthcare associated Staphlycoccus aureus bloodstream infection workshop agenda 14 August 2014 Co-hosted HICSIG of ASID / ACIPC Chairs Associate Professor Eugene Athan Convenor HICSIG of ASID Dr Marilyn Cruickshank ACSQHC 9:30am Registration tea, coffee and muffins 10:00am Introduction and Purpose 10:20am Surveillance History of SAB surveillance in Australia Dr Marilyn Cruickshank, ACSQHC 10:40am Strengths and weaknesses Professor Mary-Louise McLaws, UNSW Associate Professor Eugene Athan Associate Professor Leon Worth, Peter MacCallum Cancer centre/VICNISS 11:40am Successful Initiatives Zero CLABSIs in Adult ICU Barwon Health Geelong, Associate Professor Neil Orford 12:00pm Peripheral IV cannulation Austin Health, Professor Lindsay Grayson 12:20pm Preventing CLABSIs in NICU Adelaide Women & Children’s Hospital, Ms Jan Whitelaw Questions 12:30pm Lunch Break 1:30pm SAB event validation and experiences Canberra Professor Peter Collignon 1:50pm Newcastle Associate Professor John Ferguson 2:10pm Brisbane Dr Naomi Runnegar 2:10pm Panel discussion/debate and the way forward 3:10pm Summation 3:30 pm Close 60 min Report on healthcare associated Staphylococcus aureaus bacteraemia workshop Page 2 of 2