Medical Form - Salt Lake Community College
advertisement

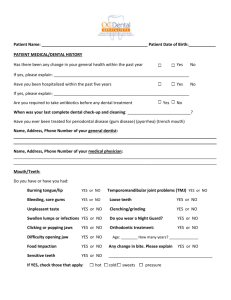
Pt ID # _________________ Medical/Dental History Form Office Use Only SLCC has written policies on this clipboard to protect your privacy. Please read them and if you have any questions, please ask. The Medical/Dental History form should be answered completely and as accurately as possible. The information will allow us to provide appropriate care for you. Thank you for being a patient in our student dental hygiene clinic. Please Fill Out This Form Completely Last Name ______________________________ First Name ________________________________ Middle Initial __________ Gender: M F Address_______________________________________________________________________ Date of Birth: ______________ Street City State Zip Phone (h) ________________ Phone (w) _________________Phone (c) _____________________ email __________________ How do you prefer that we contact you? ___________________________Occupation: __________________________________ Emergency Contact __________________________________Relationship ___________________ Phone _________________ Dental History Dentist’s Name ______________________________ City/State __________________________ Phone ___________________ A. Do your gums bleed when you brush or floss? B. Are your teeth sensitive to hot, cold, sweets, pressure? C. Does food or floss catch between your teeth? D. Is your mouth often dry? E. Have you had periodontal (gum) treatment? F. Have you had orthodontic treatment (braces)? G. Have you had a serious injury to your head or mouth? H. Do you have clicking, popping, or other discomfort in your jaw? I. Have you had any problems related to dental treatment? J. Are you currently experiencing dental pain or discomfort? U. What is the reason for your visit today? Yes No K. Do you have any sores or ulcers in your mouth? S. Date of your last dental radiographs (x-rays): T. How do you feel about your smile? L. Do you participate in energetic sports or activities? M. Do you experience frequent ulcers in your mouth? N. Do you brux (grind) your teeth? O. Do you wear dentures or partial dentures? P. Is your home water fluoridated? Q. Do you frequently drink bottled or filtered water? Yes No Yes No R. Date of your last dental exam? Medical History Yes No 1. Do you consider yourself in good health? 2. Are you currently under the care of a physician? If yes, what condition is being treated? 7. Has there been any change in your general health in the past year? 8. Have you had a serious illness, operation, or been hospitalized in the past five years? If yes, what was the illness or problem? 3. Date of your last physical exam? 9. 4. Have you taken any diet drugs such as Pondimin, Redux, or Phen-Fen? 5. Were you treated or are you presently scheduled to begin treatment with intravenous bisphosphonates? For what purpose? Do you use controlled substances/recreational drugs? If yes, what and how often? 10. Do you use tobacco? Please circle which form(s): smoke snuff chew How frequently do you use tobacco? Are you interested in learning how to quit? Date treatment began or will begin: 6. Are you taking cortisone medication? 11. Do you use alcohol? If yes, how much do you typically drink in a week? If yes, how much in the past 24 hours? If yes, when did you last use? WOMEN ONLY: 12. Are you taking birth control pills or hormone therapy? 13. Are you lactating (nursing)? 14. Are you pregnant? If pregnant, number of weeks? No Have you ever had a positive TB skin test? Yes No If yes, when? 16. Have you ever had a joint replacement Yes No What joint? If yes, did you have any complications or infections? 17. Please circle any of the following that you are allergic to or had a reaction to, and specify the type of reaction: Local anesthetics Penicillin or other antibiotics Aspirin or NSAID Barbiturates, sedatives, sleeping pills Sulfa drugs Codeine or other narcotics Metals Latex Iodine Hay fever/seasonal allergies Other 18. Drugs: Please list any prescription or over the counter medicines that you are currently taking (include vitamins, natural medicines, homeopathic or herbal supplements or remedies). Prescription Over-the-Counter (OTC) 15. Do you have or have you had tuberculosis? Yes Circle if you have or have had any of the following: 19. Damaged/artificial heart 31. Anemia valves 20. Congenital heart defects 32. AIDS or HIV 21. Cardiovascular disease 33. Arthritis 22. Angina or chest pain 34. Autoimmune disease 23. Infective endocarditis 35. Lupus erythematosus 24. Congestive heart failure 36. Asthma 25. MI (Heart attack) 37. COPD 26. High blood pressure 38. Emphysema 27. CVA (Stroke) 39. Sinus problems 28. Abnormal bleeding 40. Persistent cough 29. Hemophilia 41. Chronic pain 30. Pacemaker or Implantable 42. Diabetes Type I Cardioverter Defibrillator (ICD) 43. Diabetes Type II 44. Eating disorder 12. Mental disorder 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. If yes, specify_______________ 13. Recurrent infections If yes, specify_______________ 14. Kidney problems/hemodialysis 15. Osteoporosis 16. Persistent swollen neck glands 17. Wheezing/shortness of breath 18. Significant/rapid weight change 19. Sexually transmitted infection 20. Cold sores or fever blisters 21. Excessive urination, thirst, hunger Special diet Gastrointestinal disease GERD/Reflux Ulcers Thyroid problems Glaucoma Hepatitis, liver disease Epilepsy Physical limitation(s) Sleep disorder Cancer, chemotherapy, radiation 66. Has a physician recommended that you take antibiotics prior to professional oral health care (dental work)? Yes 67. Do you have any disease, condition, or problem not listed on this form that you think we should know about? Please explain? Yes No No Physician’s Name _____________________________ City/State _______________________________Phone _______________ I understand the importance of complete and truthful medical and dental information and that incorrect information could pose a serious threat to my health. To the best of my knowledge, the answers to the preceding questions are true and correct. I will not hold the Salt Lake Community College (SLCC) or any person who provides dental hygiene or dental services responsible for any actions that they take or do not take because of any errors or omissions that I may have made in the completion of this form. I consent to the release of medical/dental information to my dentist, physician, or other healthcare professional if requested. Further, if I ever have any change in my health, or if my medications change, I will inform my student dental hygienist or a SLCC faculty member at my next appointment without fail. I hereby grant permission to be treated by students and faculty of SLCC. __________________________ _____________ __________________________ Signature of Patient/Legal Guardian Date Date ________________________________________________________ Signature of Clinical Instructor Signature/Number Signature of Student/Number ________________________ Date Note: Your signature below verifies that any necessary changes to the history for subsequent appointments have been noted and dated on the form. A new medical/dental history form must be completed every three years. a. Date: _______ Yes No Patient Signature ______________________________ Student ____________________ CI Init b. Date: Yes No Patient Signature ______________________________ Student ____________________ CI Init c. Date: Yes No Patient Signature ______________________________ Student ____________________ CI Init d. Date: Yes No Patient Signature ______________________________ Student _____________ ____ __ CI Init e. Date: Yes No Patient Signature ______________________________ Student ____________________ CI Init f. Date: Yes No Patient Signature ______________________________ Student ________________ ___ CI Init