Renal Colic Fact Sheet - Improving Care In ED
advertisement
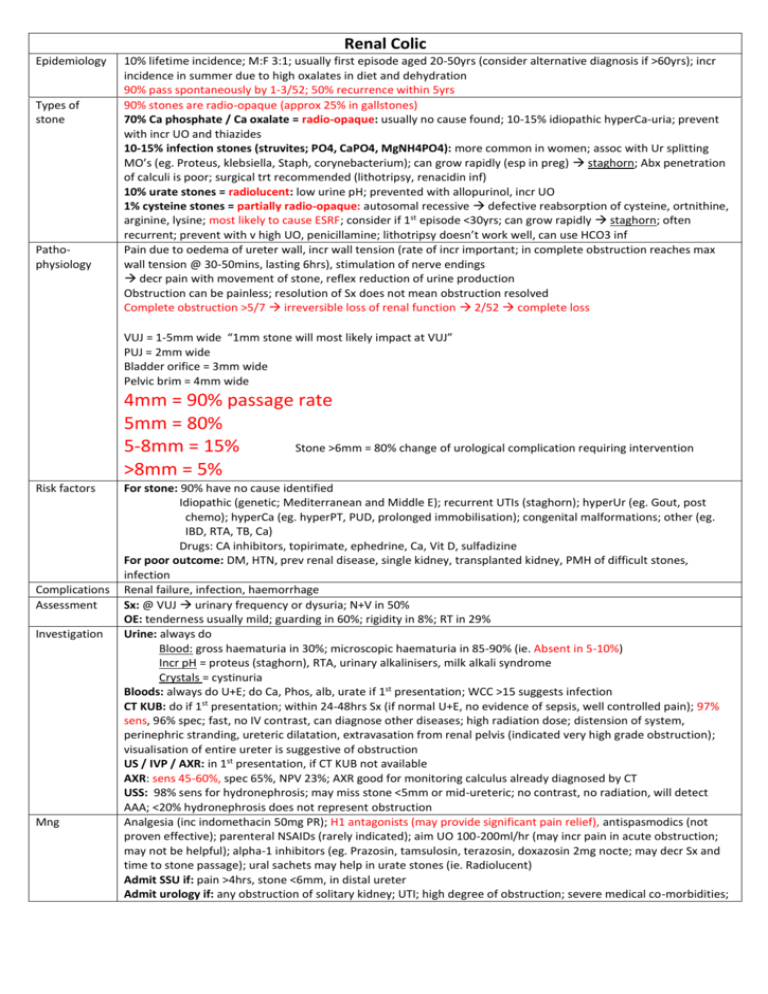
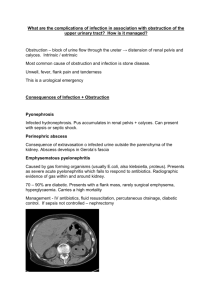
Renal Colic Epidemiology Types of stone Pathophysiology 10% lifetime incidence; M:F 3:1; usually first episode aged 20-50yrs (consider alternative diagnosis if >60yrs); incr incidence in summer due to high oxalates in diet and dehydration 90% pass spontaneously by 1-3/52; 50% recurrence within 5yrs 90% stones are radio-opaque (approx 25% in gallstones) 70% Ca phosphate / Ca oxalate = radio-opaque: usually no cause found; 10-15% idiopathic hyperCa-uria; prevent with incr UO and thiazides 10-15% infection stones (struvites; PO4, CaPO4, MgNH4PO4): more common in women; assoc with Ur splitting MO’s (eg. Proteus, klebsiella, Staph, corynebacterium); can grow rapidly (esp in preg) staghorn; Abx penetration of calculi is poor; surgical trt recommended (lithotripsy, renacidin inf) 10% urate stones = radiolucent: low urine pH; prevented with allopurinol, incr UO 1% cysteine stones = partially radio-opaque: autosomal recessive defective reabsorption of cysteine, ortnithine, arginine, lysine; most likely to cause ESRF; consider if 1st episode <30yrs; can grow rapidly staghorn; often recurrent; prevent with v high UO, penicillamine; lithotripsy doesn’t work well, can use HCO3 inf Pain due to oedema of ureter wall, incr wall tension (rate of incr important; in complete obstruction reaches max wall tension @ 30-50mins, lasting 6hrs), stimulation of nerve endings decr pain with movement of stone, reflex reduction of urine production Obstruction can be painless; resolution of Sx does not mean obstruction resolved Complete obstruction >5/7 irreversible loss of renal function 2/52 complete loss VUJ = 1-5mm wide “1mm stone will most likely impact at VUJ” PUJ = 2mm wide Bladder orifice = 3mm wide Pelvic brim = 4mm wide 4mm = 90% passage rate 5mm = 80% 5-8mm = 15% Stone >6mm = 80% change of urological complication requiring intervention >8mm = 5% Risk factors Complications Assessment Investigation Mng For stone: 90% have no cause identified Idiopathic (genetic; Mediterranean and Middle E); recurrent UTIs (staghorn); hyperUr (eg. Gout, post chemo); hyperCa (eg. hyperPT, PUD, prolonged immobilisation); congenital malformations; other (eg. IBD, RTA, TB, Ca) Drugs: CA inhibitors, topirimate, ephedrine, Ca, Vit D, sulfadizine For poor outcome: DM, HTN, prev renal disease, single kidney, transplanted kidney, PMH of difficult stones, infection Renal failure, infection, haemorrhage Sx: @ VUJ urinary frequency or dysuria; N+V in 50% OE: tenderness usually mild; guarding in 60%; rigidity in 8%; RT in 29% Urine: always do Blood: gross haematuria in 30%; microscopic haematuria in 85-90% (ie. Absent in 5-10%) Incr pH = proteus (staghorn), RTA, urinary alkalinisers, milk alkali syndrome Crystals = cystinuria Bloods: always do U+E; do Ca, Phos, alb, urate if 1st presentation; WCC >15 suggests infection CT KUB: do if 1st presentation; within 24-48hrs Sx (if normal U+E, no evidence of sepsis, well controlled pain); 97% sens, 96% spec; fast, no IV contrast, can diagnose other diseases; high radiation dose; distension of system, perinephric stranding, ureteric dilatation, extravasation from renal pelvis (indicated very high grade obstruction); visualisation of entire ureter is suggestive of obstruction US / IVP / AXR: in 1st presentation, if CT KUB not available AXR: sens 45-60%, spec 65%, NPV 23%; AXR good for monitoring calculus already diagnosed by CT USS: 98% sens for hydronephrosis; may miss stone <5mm or mid-ureteric; no contrast, no radiation, will detect AAA; <20% hydronephrosis does not represent obstruction Analgesia (inc indomethacin 50mg PR); H1 antagonists (may provide significant pain relief), antispasmodics (not proven effective); parenteral NSAIDs (rarely indicated); aim UO 100-200ml/hr (may incr pain in acute obstruction; may not be helpful); alpha-1 inhibitors (eg. Prazosin, tamsulosin, terazosin, doxazosin 2mg nocte; may decr Sx and time to stone passage); ural sachets may help in urate stones (ie. Radiolucent) Admit SSU if: pain >4hrs, stone <6mm, in distal ureter Admit urology if: any obstruction of solitary kidney; UTI; high degree of obstruction; severe medical co-morbidities; In paeds decr renal function (Cr>200); persistent pain (despite 24hrs in SSU); stone >6mm; transplanted kidney Definitive trt if: stone >7mm; infection; high degree obstruction not resolving; failure of conservative trt at 4-6/52 + symptoms Perc nephrolithotomy preferred (esp if staghorn, multiple, complex) Ureteroscopy preferred if pregnant, morbid obese, coagulopathy, lower ureteric stones Shockwave lithotripsy if prox ureteral calculi <10mm (best for Ca oxalate or struvite) - complicated by some renal inj in 50%, rarely other organs inj, serious complication <1%, haematuria for 3/7, passage of stone fragments (colic in 15%) 30% children will have urinary tract abnormality; 20-30% present with painless haematuria Notes from: Dunn, Cameron, TinTin