Peripheral Vasopressors
advertisement

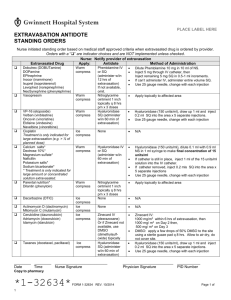
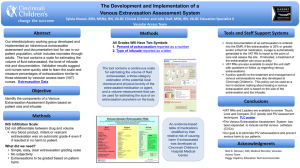
Last Updated: 07/2015 VCU Emergency Department: Peripheral Vasopressor Guidance Criteria: 1. Limited to norepinephrine at doses of <20 mcg/min 2. A central line should be placed as soon as possible to minimize the risk of extravasation 3. Peripheral IV (PIV) must be placed at or above the antecubital fossae (AC) or external jugular (EJ) with a minimum of a 20 gauge catheter or larger 4. Selected PIV must first be rapidly flushed with 10 mL NaCl 0.9% and then return blood 5. The PIV site will be continuously monitored by nursing and documented in iView at a minimum of every 4 hours 6. The maximum duration of PIV vasopressor use is 4 hours. This maximum duration should not preclude the placement of a central line as soon as possible 7. The utilization of a peripheral vasopressor should not delay transport to a higher level of care 8. This guidance does not apply in the emergent cardiac arrest/return of spontaneous circulation Background: Patients in the emergency department (ED) often require emergent vasopressor management for hemodynamic stabilization. The maintenance of a patient's perfusion to vital organs such as the brain, heart, and kidneys should not be delayed by the placement of a central line that is often time and resource intensive. Published literature has shown that patients have been safely managed on peripheral vasopressors if appropriate precautions are taken. Three studies have looked at the peripheral administration of vasopressors. Publications by Loubani et al and Turner et al identify characteristics associated with extravasation injury including poor PIV placement, prolonged infusion time, and high doses. i,ii Ricard et al is the only prospective, randomized controlled trial that compared peripheral vs. central catheter use in the ICU patient population and found no difference in the number of mechanical complications, of which included subcutaneous diffusion. iii A summary of the aforementioned studies is below: A systematic review completed by Loubani et al. included publications that looked at adult patients who received IV vasopressors as part of their intended medical care that experienced adverse events that were attributed to vasopressor administration. i Overall, 85 publications and 270 patients with 325 separate events were included. In the peripheral vasopressor group, events were separated into local tissue or extravasation injuries. Of the 204 local tissue injury events, 85.3% of them had peripheral catheters located at a site distal to the AC or popliteal fossae. The average duration of infusion before local tissue injury was 55.9 hrs (+/- 68.1), with a median of 24 hrs and a range of 0.08-528 hrs. Major disability was reported in 4.4% of events and in 2% of these events, the complications arising from the use of peripheral vasopressors were felt to be a significant contributor to mortality. Of 114 extravasation events, 75% of the events were located distal to the AC or popliteal fossa. The average duration was 35.2 hrs (+/- 51), with a median of 22 hrs, and a range of 0.26-240 hrs. Long-term sequelae were reported in 112 events, of these only 3 events (2.7%) resulting in major disability and only one event (0.9%) was felt to be a significant contributor of mortality. Overall, a majority of local tissue injuries occurred at sites distal to the AC and after more than 6 hrs of vasopressor infusion. In a retrospective, pediatric transport study, the use of peripheral IVs in 73 patients resulted in 11 infiltrations.ii Median age was 1 year old (range from birth to 19 years old) and dopamine monotherapy was used in 90% of cases. Patients with IV infiltrates had a longer median vasopressor infusion time (13.5 hrs vs. 4.2 hrs, P<0.05) and had a higher median maximum dopamine dose (15 mcg/kg/min vs. 10 mcg/kg/min, P<0.05). All infiltrations occurred after arrival to the accepting institution, not during transport. Ricard et al randomized 266 intensive care unit (ICU) patients to central or peripheral venous access.iii The primary endpoint was the rate of major catheter related complications within 28 Last Updated: 07/2015 days. Regarding vasopressor administration, the peripheral group was required to switch to the central group if epinephrine/norepinephrine requirements were greater than 2 mg/h (~ 33 mcg/min) or dopamine/dobutamine requirements were greater than 10 mcg/kg/min. The study found that the number of major catheter-related complications was greater in the peripheral than the central catheter group (133 vs. 86, P=0.02), however, this was mostly driven by complications with peripheral IV insertion. Nineteen patients in the peripheral and two in the central catheter groups experienced subcutaneous diffusions. In correspondence, the authors noted that all patients in the peripheral catheter group only required observation and conservative management. Management of Extravasation Possible signs and symptoms of extravasation include blanching along the course of the infused vein, acrocyanosis, swelling, and dermal sloughing. If there is suspicion for vasopressor extravasation or any of these symptoms occur the supervising physician should be notified immediately. If a peripheral or central vasopressor extravasation occurs, the following steps should be taken to minimize adverse sequelae: 1. Stop vasopressor infusion (relocate if necessary) and disconnect IV tubing, leaving catheter in place 2. Attempt to aspirate the residual drug volume from the catheter using a 1 mL or 3 mL syringe 3. Apply a hot compress to area to improve local blood flow and enhance drug removal 4. Perform a 1:10 dilution of phentolamine (5 mg/mL) by placing 1 mL of phentolamine in 9 mL of NaCl 0.9%. Administer phentoalmine through the catheter and subcutaneously around the site of infiltration using a 25-gauge needle. Repeat dose if necessary 5. Monitor HR, BP Phentoalmine is an α-adrenergic agonist that promotes vasodilation and capillary blood flow. It is considered effective within the first 12 hrs of extravasation injury. If phentolamine is not available, prescribers may consider topical nitroglycerin 2% and/or subcutaneous tertbutaline, though evidence supporting efficacy is limited.iv,v,vi This guidance was approved by the VCU Emergency Department Quality Committee on 07/13/15. This document is for internal use only. i Loubani OM, Green RS. A systematic review of extravasation and local tissue injury from administration of vasopressors through peripheral intravenous catheters and central venous catheters. J Crit Care 2015. ii Turner DA, Kleinman ME. The use of vasoactive agents via peripheral intravenous access during transport of critically ill infants and children. Pediatr Emerg Care 2010;26(8):563-6. iii Ricard JD, Salomon L, Boyer A, Thiergy G, Meybeck A, Roy C et al. Central or peripheral catheters for initial venous access for ICU patients: a randomized controlled trial. Crit Care Med 2013;41:2108-15. iv Denkler KA, Cohen BE. Reversal of dopamine extravasation injury with topical nitroglycerin ointment. Plast Reconstr Surg 1989;84(5):811-3. v Wong AF, McCulloch LM, Sola A. Treatment of peripheral tissue ischemia with topical nitroglycerin ointment in neonates. J Pediatr 1992;121(6):980-3. vi Stier PA, Bogner MP, Webster K, Leikin JB, Burda A. Use of subcutaneous terbutaline to reverse peripheral ischemia. Am J Emerg Med 1999;17:91-4. T. Nguyen, PharmD