transition from health visitor to school nurse
advertisement
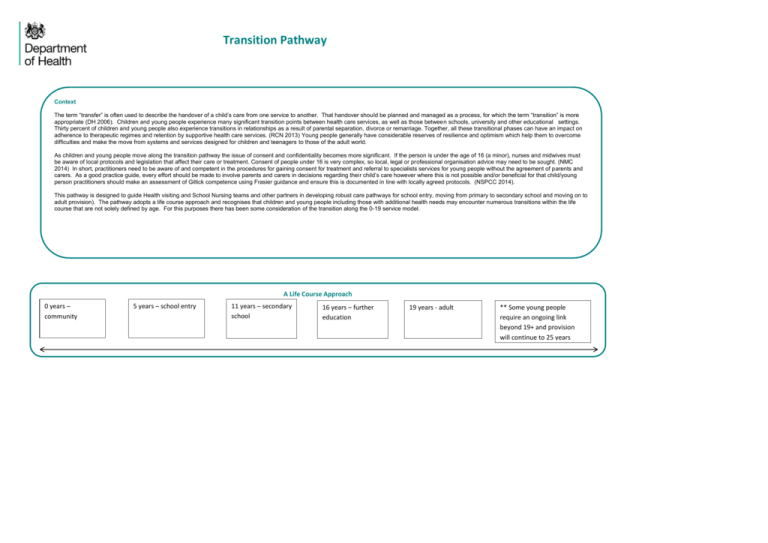
Transition Pathway Context The term “transfer” is often used to describe the handover of a child’s care from one service to another. That handover should be planned and managed as a process, for which the term “transition” is more appropriate (DH 2006). Children and young people experience many significant transition points between health care services, as well as those between schools, university and other educational settings. Thirty percent of children and young people also experience transitions in relationships as a result of parental separation, divorce or remarriage. Together, all these transitional phases can have an impact on adherence to therapeutic regimes and retention by supportive health care services. (RCN 2013) Young people generally have considerable reserves of resilience and optimism which help them to overcome difficulties and make the move from systems and services designed for children and teenagers to those of the adult world. As children and young people move along the transition pathway the issue of consent and confidentiality becomes more significant. If the person is under the age of 16 (a minor), nurses and midwives must be aware of local protocols and legislation that affect their care or treatment. Consent of people under 16 is very complex, so local, legal or professional organisation advice may need to be sought. (NMC 2014) In short, practitioners need to be aware of and competent in the procedures for gaining consent for treatment and referral to specialists services for young people without the agreement of parents and carers. As a good practice guide, every effort should be made to involve parents and carers in decisions regarding their child’s care however where this is not possible and/or beneficial for that child/young person practitioners should make an assessment of Gillick competence using Frasier guidance and ensure this is documented in line with locally agreed protocols. (NSPCC 2014). This pathway is designed to guide Health visiting and School Nursing teams and other partners in developing robust care pathways for school entry, moving from primary to secondary school and moving on to adult provision). The pathway adopts a life course approach and recognises that children and young people including those with additional health needs may encounter numerous transitions within the life course that are not solely defined by age. For this purposes there has been some consideration of the transition along the 0-19 service model. A Life Course Approach 0 years – community 5 years – school entry 11 years – secondary school 16 years – further education 19 years - adult ** Some young people require an ongoing link beyond 19+ and provision will continue to 25 years Framework . Transition of Children and Young People with Long Term Conditions (LTC) to Adult Services Transition of Children and Young People through the life Course who are at Risk of Significant Harm Getting transition right for children with LTC should be seen as a whole system approach; early help (including the support of Specialist community Public Health nursing) will improve health outcomes, keeping children/young people out of hospital for longer and/or reduce the need for hospital admissions into adult life. The government reforms detailed in Children and Families Bill (2013) intend to transform the system for children and young people with special educational needs (SEN), including those who are disabled, so that services consistently support the best outcomes for them. It intends to do this by replacing statements and learning difficulty assessments with a new birth- to-25 Education, Health and Care Plan, extending rights and protections to young people in further education and training and offering families personal budgets so that they have more control over the support they need. This may mean the planning of transition into adult services for these young people is delayed. When participating in the planning transition of services practitioners should:- Safeguarding and promoting the welfare of children can be defined as; protecting children from maltreatment, preventing impairment of children's health or development, ensuring that children are growing up in circumstances consistent with the provision of safe and effective care and taking action to enable all children to have the best chances. Child protection is part of safeguarding and promoting the welfare of children and refers to the activity that is undertaken to protect specific children who are suffering, or are likely to suffer, significant harm. (DFE 2013). The specialist community public health function involves a capacity not only to participate actively in public health provision but also ensure it is practised within a safe environment. (NMC 2004) Throughout the life course this means services designed to promote health outcomes for children and young people should consider a seamless approach to the transition and should:- Embrace children and young people’s enthusiasm for ‘growing up’ and not just concentrate on the young person’s health problem Understand that as they grow older children and young people need to be increasingly involved with and leading on the management of their LTC taking responsibility for their own health. Consider that an increasing number of children with complex disorders that only a few years ago were fatal in infancy or childhood now survive into adolescence and adult life, presenting new challenges. Understand that although coping with the adult world may be seen as a normal part of development, many young people cannot cope with the frustration and anxiety and disengage with the process leading to deterioration in their condition which can have serious consequences on their health and wellbeing. Ensure the concept of transition is introduced to children, young people and their families long before it becomes an issue. Ensure transition process begins early – ensure all professional perspectives are considered it is helpful to embed medical transition within the broader context of growing up and/or moving on i.e. HV views should be considered when a child is entering school including producing a health care plan if appropriate, the views of education staff should be considered when a young person is being considered for transfer to adult health services. Identify the skill set required for child/young person to function in an adult clinic – a transition check list may be useful. Liaise with the child and family and specialist services to identify the child/families understanding of the disease process, treatment and possible side effects. This knowledge and understanding should be re-assessed at key points during the transition process. Consider ‘welcoming’ teams or process within receiving services to ensure that families, children/young people understand specific service provisions ie what services are available. Ensure a child’s records are available for review wherever possible – this ensures that vital information is not missed and so that families do not feel they have to keep ‘telling their story’ at each transition point. Ie 0-19 records, CAF, discharge summaries or other locally agreed processes. Add complex needs pathway link her Consider that families do not necessarily see transition as significant in a child’s journey; the family stay the same during this period it’s the systems and professionals that change. Ensure that transition is seamless; this builds the confidence of children, young people and their families that ‘things will stay the same’. Ensure early communication with families prior to transition creating the opportunity for ‘‘thinking time resource’ – so that families can anticipate what their needs might be. Consider that positive transition experiences will have an impact on attainment as it will; increase school readiness, improve school attendance, which will often improve academic attainment and increase independence and ability to access adult health services which will contribute to prevention of ill health and disease in adult life. Ie dentist service, GP services, sexual health services, smoking cessation etc. Develop ongoing links with universal health services beyond 19+. For some children/YP this may be required (including those with Child Protection plans) to ensure the ongoing reduction of significant harm. (ie discharge to GP services). Consider which professionals actually need to have direct contact with families and minimise the amount of ‘visits’ – i.e. consider multi-agency joint visits where possible Include children, young people and their families in decisions and communications to ensure they are informed about who is the lead health professional. Ensure assumptions regarding non-engagement are not made- it is important for professionals to build trusting relationships at each transition point. Develop Joint HV/SN health records to ensure all significant information is recorded and communicated. Develop Robust locally agreed transfer processes to ensure pertinent information is shared between other services as required (ie identified support services) Health Visiting and School Nursing Programme: Supporting the implementation of the new service offer: No 5: Safeguarding children and young people: enhancing professional practice: working with children and families Compassion in practice: Nursing, Midwifery and Care Staff: Our Vision and Strategy support the core values of public health nursing. School nurses have the potential to transform the care, advice and support that people receive. Compassionate care values and behaviours should be at the centre of all interventions and particularly at times when service deliver may mean changes in relationships and when clinical expertise is required. The 6c’s will promote professionals in building trusting relationships with children, young people and their families in order to ensure improved health outcomes Care Commit to providing care in a range of settings in order to provide services that are accessible and visible Ensure the completion of health screens and understand criteria for appropriate referral to specialist services in a timely manner. Deliver the healthy child programme 0-19. Compassion Ensure an open, honest and non-judgemental approach when delivering care Develop trusting relationships and give early information to families particularly when referrals to other services are required. Recognise that children live in homes not in organisations – services should be child focussed NOT service focussed. Competence Develop skill mix teams Ensure all staff are appropriately trained to deliver services Ensure all care givers (including families and education staff) are competent and confident to deliver care. Develop evidence based packages of care that are regularly updated Ensure equipment and resources are regularly serviced and calibrated to ensure accurate results data Communication Ensure information sharing protocols are in place and understood – providing a flow of information. Develop electronic 0-19 health records Embrace modern technology to deliver improved health outcomes and access to information for staff, children, young people and their families. Courage Seek opportunities to provide innovative care that is child/family focussed Support children, young people and their families to make decisions that will lead to improves outcomes Develop strong working relationships with commissioners and other stakeholders to speak on behalf of children and young people when service provision is inadequate including seeking solutions. Commitment Demonstrate a commitment to improve the emotional, mental, physical and social health and wellbeing of children young people and their families. Seek opportunities to provide high quality services to the local population. Commit to working collaboratively with children, young people and their families, specialist services and the wider multiagency team. Primary Actions Optimising 0-19 services at local service level will ensure the best possible outcomes for children, young people and their families, reduce duplication of provision therefore increase service capacity and ensure a universally delivered service that is seamless. This involves influencing commissioning, working in partnership with service users and key stakeholders and adapting national guidance (including this pathway) when planning local arrangements for transition. This pathway can contribute to improving the seamless delivery of services by considering the following actions:Commissioning Identify health visitors and school nurses at all levels but particularly those leading services work closely with commissioners to improve the service offer and provision to children and young people across the pathway in order to ensue services are effective, efficient and relevant to the local population. Ensure professional Public Health representatives are involved in shaping the direction of universal 0-19 services in order to maintain a strong professional identity and high standards of care. Ensure a clear professional representation at strategic level in order to influence future commissioning. Support Commissioners in gaining a clearer insight of the role of school nursing to ensure the effective delivery of the Healthy Child Programme Ensure commissioners gain clear access to professionals with joint accountability and responsibility to develop working positive relationships with provider organisations. Conflicting Agendas Identify a clear understanding of roles for practitioners working within universal services in order to ensure a reduction in duplication for children/young people and their families. Develop robust key performance indicators and quality data to ensure the core universal offer is delivered and to identify and measure an enhanced offer. Ensure commissioners have sight of Department of Health service specification and academic calendar when planning services and re-procuring services. Identify the unique selling point (USP) of service delivery in order to identify areas of delivery that may be duplicated across the pathway thus potentially building capacity. Identify the core service particularly where there are reductions in workforce, ensuring that this is prioritized in terms of service delivery in order to reduce health inequalities. Introduce skill mix teams in order to share expertise and skills and maintain and support specialist community public health (SCPHN) role Identify additional funding streams including but not restricted to income generation, applying for professional grants and identifying additional work stream contracts bid for outside of current service specification. See Nursing Technology Fund Mary Seacole Awards and Burdett Trust for Nursing. Communication Promote innovative practice through local professional forums, regional and national events i.e. SAPHNA and CPHVA conferences and forums, and using social media ie participating on twitter, webinars etc. Embed transition pathway in and out of local authority, education etc. Embed the call to action for HV and SN providing national recognition of professional roles and the importance of those roles in the delivery of the Healthy Child Programme – 0-19. Develop a better understanding and recognition of the roles and responsibilities of all professionals working with children and young people resulting in a more cohesive approach to multi agency working and improve the outcome for children young people and their families. Engagement Consider engaging young people in the School Nurse ambassador programme Identify areas of the service that can be assessed for You’re welcome status and strive towards achieving this. Also encourage other services to achieve this ie GP, local pharmacies etc in order to ensure local services are accessible to young people. Ensure that young people are consulted on service provision including considering having young people of recruitment panels. Ensure services are robustly evaluated and shaped and to measure when an intervention has provided accessible and user friendly services and assess positive outcomes. Case studies Shropshire 0-19 Services – Health visitors and school nurses attend continence training sessions/workshops with other health professionals such as a Clinical Psychologist. This aids toileting and tackles any constipation issues before they become a real problem however, consistent advice and support can be transferred from the health visitor to the school nurse in an effective way. For example a 5 year old was soiling at school and the work that the HV had commenced was passed to SN to continue and this appeared expedited resolution of his issue in conjunction with the Telford Constipation Service. School nurses use power-point and interactive assemblies for Years 6 and 7 to address school transitional anxiety. We have “Crucial Crew” - a group session for all Year 6s in Telford which has many different professionals aiding transitional phase including Electric Companies, Fire Service, Police and School Nurses, the latter providing constructive advice in a game format addressing any anxieties with Primary to Secondary school transition. The Bridge Foundation - The Stepping Up project is delivered by a partnership of five Bristol voluntary organisations and provides specialist support to vulnerable children/young people before, during and after the period of their transition from primary to secondary school. The Project meets the emotional, physical and social needs of young people through 1:1counselling, sports / creative groups: 1:1 year long mentoring for children living in families with substance misuse issues; and an intensive environmental group programme and 3 day summer residential. The young people entering the Stepping Up programme frequently have complex or troubled family situations, involving loss, frequent change, relationship breakdown and/or disrupted attachments. Once in secondary school, without support, this can lead to poor attendance, disruptive behaviour and lower attainment. Support begins in year 6 and continues into the first term in secondary school. Further places are available for children whose difficulties come to the schools attention in year 7. A high importance is placed on partnership working – within the Stepping up partnership, between the project and the schools and importantly with parents. The project has involvement with most parents at the Primary school stage and continuing into the secondary school. Many of those parents feel more confident in their contact with school and consequently have a greater involvement in their child’s educational progress. We have completed the first full year of activities and are encouraged by reported outcomes. For example; attendance of children participating in Stepping Up increased from 66% in year 6 to 88% in year 7. The ongoing needs of each child/ family are considered at the end of Stepping Up involvement. The secondary school continues to offer appropriate support; young people can have the opportunity to attend other sports or creative activities and children attending last year’s residential continue to meet as a peer group. Coram Project Coram Life Education (CLE) Supporting Schools – working in Lancashire primary schools following a review of the school’s PSHE policy. The intention of the programmes was to build resilience of children as they moved to adolescence so they could make positive assertive choices in their lives and because they are based in a holistic framework address all aspects of health and wellbeing including relationships with others personal confidence etc. CLE delivered lessons for children at Years 1 and 2 (Key Stage 1) and Years 3, 4, 5 and 6 (Key Stage 2) about how the body works and how to keep physically and emotionally healthy and safe. The specially-trained educators provided lessons which were fun, using active learning strategies and innovative teaching techniques including songs, brain games and role play, which are evidenced to be memorable year on year. Evaluation (pupil questionnaire) found a 100% positive response to ‘not smoking’ and the dangers of alcohol putting them in the 1st percentile in Lancashire. The School was one of the first schools in Lancashire to gain National Healthy School Status and the school’s strength in drug and alcohol awareness was recognised in its Ofsted report. Acknowledgements Betsy Allen Professional Lead for School Nursing, Devon Integrated Children’s Services Virgin Care Limited Catherine Ashton Julie Bulmer Locala Community Partnerships David Burton Coram Life Education Mary Dillon-Hanley Central London Community Healthcare Trust Beverley Evans Health Transition Lead for Young People with Complex Physical Health Needs Ealing ICD Diane Evans Clinical Lead – School Nursing Walsall Healthcare NHS Trust Heidi Ferrier-Hixon Lead Nurse – Universal Plus School Nursing Team Sandwell and West Birmingham NHS Trust Glenda Bestford Public Health School Nurse Team Lead Newcastle Upon Tyne Hospitals NHS Foundation Trust Frances Fox Director The Bridge Foundation Sue Garland Service Lead – School Nursing Staffordshire and Stoke-on-Trent Partnership Trust Jo Gregg Jenny Hallsworth Lancashire Care NHS Trust Julie Hughes Royal Berkshire NHS Trust Carrie James Health Transition Case Manager Walsall Healthcare NHS Trust Ceri Anwen James-Ellis Senior Lecturer (Faculty of Education, Health and Community) Liverpool John Moores University Ros Jagoe Specialist Community Public Health Nurse (School Nurse) Shropshire Community Health NHS Trust Annemarie Kennedy Coventry and Warwickshire Partnership NHS Trust Kath Lancaster Orla McAlinden Lecturer in Children and Young People’s Nursing Queens University Belfast Helen Molloy Blackpool, Fylde and Wyre Hospitals NHS Foundation Trust E Owen Farhaj Parthan Quality Improvement Lead – Young People and Transition into Adulthood NHS England Rachel Osborne Shropshire Community Health NHS Trust Getting it right for children, young people and families: Maximising the contribution of school nursing team: Vision and call to action Department of Health, 2012 Healthy Child Programme: From 5-19 years old, Department of Health and Department for Children, Families and Schools, 2009 Getting the right start: National Service Framework for Children: Standard for Hospital Services Department of Health, 2003 Transition: Moving on well: A good practice guide for professionals and their partners on transition planning for young people with complex needs or a disability, Department of Health, 2008 Think transition: Developing the essential link between paediatric and adult care, Royal College of Physicians of Edinburgh, 2008 Nursing and Midwifery Council, Consent Claire Robson Public Health England Kerry Rose South Warwickshire NHS Foundation Trust Jackie Ruddy Coventry and Warwickshire Partnership NHS Trust Lynne Schuller Clinical Lead, Healthy Child Programme 5-19 Rotherham, Doncaster and South Humber NHS Foundation Trust Carla Williams SCPHN Student Sandwell and Birmingham NHS Trust Sheila Thomas Acting Matron/Team Leader – School Health Sandwell and Birmingham Hospitals NHS Trust Secretariat Ruth Cohen, Clinical Lead for School Health, Barts Health NHS Trust Wendy Nicholson, Professional Officer – School and Community Nursing, Department of Health Fiona Hill, PA to Professional Officer – School and Community Nursing, Department of Health Lost in Transition: moving young people between child and adult health services, Royal College of Nursing, 2013 Transition: Getting it right for young people: Improving the transition of young people with long term conditions, Department of Health, 2007 Sharon Poole Registered Nurse – Student Public Health Nurse Worcestershire Health and Care Trust Frances Walsh SCPHN Student South Warwickshire NHS Foundation Trust References and Resources Lisa Worth Gillick Competency and Fraser Guidelines, NSPCC, 2014 Working Together to Safeguard Children: A guide to inter-agency working to safeguard and promote the welfare of children, HM Government , 2013 Children and Families Bill 2013, Department for Education, 2013 Compassion in practice: Nursing, Midwifery and Care Staff: Our Vision and Strategy Resilience in the face of adversity: Protective factors and resistance to psychiatric disorder. Rutter, M. 1985