- National League for Nursing
advertisement

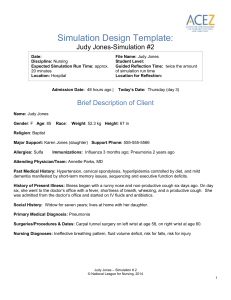
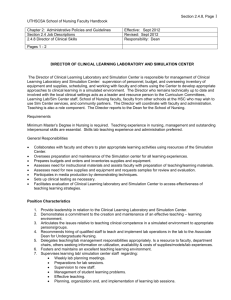
Simulation Design Template: Judy Jones-Simulation #1 Date: Discipline: Nursing Expected Simulation Run Time: approx. 20 minutes Location: Hospital Admission Date: Yesterday | File Name: Judy Jones Student Level: Guided Reflection Time: twice the amount of simulation run time Location for Reflection: Today’s Date: Wednesday (day 2) Brief Description of Client Name: Judy Jones Gender: F Age: 85 Race: Weight: 52.3 kg Height: 67 in Religion: Baptist Major Support: Karen Jones (daughter) Support Phone: 555-555-5566 Allergies: Sulfa Immunizations: Influenza 3 months ago; Pneumonia 2 years ago Attending Physician/Team: Annette Parks, MD Past Medical History: Hypertension, cervical spondylosis, hyperlipidemia controlled by diet, and mild dementia manifested by short-term memory issues, sequencing and executive function deficits. History of Present Illness: Illness began with a runny nose and non-productive cough six days ago. On day six, she went to the doctor’s office with a fever, shortness of breath, wheezing, and a productive cough. She was admitted from the doctor’s office and started on IV fluids and antibiotics. Social History: Widow for seven years; lives at home with her daughter. Primary Medical Diagnosis: Pneumonia Surgeries/Procedures & Dates: Carpal tunnel surgery on left wrist at age 58, on right wrist at age 60. Nursing Diagnoses: Ineffective breathing pattern, fluid volume deficit, risk for falls, risk for injury Judy Jones – Simulation # 1 © National League for Nursing, 2014 1 Psychomotor Skills Required Prior to Simulation General head-to-toe assessment Applying nasal cannula Incentive spirometry Patient transfer/ambulation skills Cognitive Activities Required Prior to Simulation [i.e. independent reading (R), video review (V), computer simulations (CS), lecture (L)] Read information in textbook and lecture notes on community acquired pneumonia, dementia and delirium, and care of confused older adult. (R) (L) Tools in the Try This: ® and How to Try This Series, available on ConsultGeriRN.org (http://consultgerirn.org/resources). Specific tools recommended for this scenario are the Confusion Assessment Method (CAM), Mini-Cog TM, Updated Beers Criteria and Family Questionnaire. (R) Simulation Learning Objectives General Objectives 1. Practice standard precautions throughout the exam. 2. Employ effective strategies to reduce risk of harm to the client. 3. Assume the role of team leader or member. 4. Perform a focused physical assessment noting abnormal findings. 5. Recognize changes in patient symptoms and/or signs of patient compromise. 6. Perform priority nursing actions based on clinical data. 7. Reassess/monitor patient status following nursing interventions. 8. Perform within scope of practice. 9. Demonstrate knowledge of legal and ethical obligations. 10. Communicate with client in a manner that illustrates caring for his/her overall well-being. 11. Communicate appropriately with physician and/or other healthcare team members in a timely, organized, patient-specific manner. 12. Apply the nursing process to initiate care of the Alzheimer’s patient. Simulation Scenario Objectives 1. 2. 3. 4. Conduct a focused assessment. Use updated Beers criteria to assess medications ordered for the patient. Demonstrate use of non-pharmacological methods to manage an agitated patient. Respond to patient-specific physical and emotional needs related to ineffective breathing patterns. Judy Jones – Simulation # 1 © National League for Nursing, 2014 2 5. Perform the Mini-Cog TM assessment, 6. Use the Confusion Assessment Method to evaluate the client for delirium versus dementia after the scenario is completed. References, Evidence-Based Practice Guidelines, Protocols, or Algorithms Used for This Scenario: These and other tools in the Try This: ® and How to Try This Series are available on the ConsultGeriRN.org (http://consultgerirn.org/resources), the website of the Hartford Institute for Geriatric Nursing, at New York University’s College of Nursing. The tool, an article about using the tool, and a video illustrating the use of the tool, are all available for your use. Beers Criteria for Potentially Inappropriate Medication Use in Older Adults: Tool: http://consultgerirn.org/uploads/File/trythis/try_this_16.pdf Video: http://consultgerirn.org/resources/media/?vid_id=4852321#player_container Article: Fick, D.M., & Semla, T.P. (2012). 2012 American Geriatrics Society Beers Criteria: New Year, New Criteria, New Perspective. Available online at: http://www.americangeriatrics.org/files/documents/beers/Perspective_JAGS.pdf Confusion Assessment Method (CAM): Tool: http://consultgerirn.org/uploads/File/trythis/try_this_13.pdf Video: http://consultgerirn.org/resources/media/?vid_id=4361983#player_container Article:http://journals.lww.com/ajnonline/Fulltext/2007/12000/How_to_Try_This__Detecting_Delirium.27.as px Dementia: Nursing Standard of Practice Protocol: Recognition and Management of Dementia: http://consultgerirn.org/topics/dementia/want_to_know_more Assessing and Managing Delirium in Older Adults with Dementia: Tool: http://consultgerirn.org/uploads/File/trythis/try_this_d8.pdf Video: http://consultgerirn.org/resources/media/?vid_id=4361983#player_container Mental Status Assessment of Older Adults: The Mini-Cog TM Tool: http://consultgerirn.org/uploads/File/trythis/try_this_3.pdf Video: http://consultgerirn.org/resources/media/?vid_id=4361918#player_container Recognition of Dementia in Hospitalized Older Adults: Tool: http://consultgerirn.org/uploads/File/trythis/try_this_d5.pdf Video: http://consultgerirn.org/resources/media/?vid_id=4361882#player_container Judy Jones – Simulation # 1 © National League for Nursing, 2014 3 Decreasing Patient Agitation: Waszynski, C., Veronneau, P., Therrien, K., Brousseau, M., Massa, A. & Levick, S. (2013). Decreasing patient agitation using individualized therapeutic activities. AJN, American Journal of Nursing, 113 (10), 32-39. Available at: http://www.nursingcenter.com/lnc/CEArticle?an=00000446-20131000000024&Journal_ID=54030&Issue_ID=1606223 Therapeutic Activity Kits: http://consultgerirn.org/uploads/File/trythis/try_this_d4.pdf Review the Essential Nursing Actions in the ACES Framework at: http://www.nln.org/professionaldevelopment-programs/teaching-resources/aging/ace-s/nln-aces-framework Fidelity (choose all that apply to this simulation) Setting/Environment: ER Med-Surg Peds ICU OR / PACU Women’s Center Behavioral Health Home Health Pre-Hospital Other: Medications and Fluids: IV Fluids: see chart Oral Meds: IVPB: IV Push: IM or SC: Diagnostics Available: Labs X-rays (Images) 12-Lead EKG Other: Simulator Manikin/s Needed: Human patient simulator (e.g. SimMan, Vital Sim) or standardized patient. Props: Patient is sitting on the floor looking under bed. On the bedside table is an incentive spirometer, box of tissues and a small bag for used tissues with green sputum. Equipment Attached to Manikin: IV tubing with primary line D5. 45 NSS running at 42 mL/hr Secondary IV line IV pump Foley catheter mL output PCA pump running Documentation Forms: Physician Orders Admit Orders Flow sheet Medication Administration Record Kardex Graphic Record Shift Assessment Triage Forms Code Record Anesthesia / PACU Record Standing (Protocol) Orders Transfer Orders Other: Students will need copies of the Mini-Cog Judy Jones – Simulation # 1 © National League for Nursing, 2014 4 IVPB with running at mL/hr 02 set at 2L; nasal cannula in an empty bed Monitor attached ID band Other: and CAM tools. You may provide them or assign learners to retrieve them from www.consultgerirn.org. Recommended Mode for Simulation: (i.e. manual, programmed, etc.) either Equipment Available in Room: Bedpan/Urinal Student Information Needed Prior to Scenario: Foley kit Straight Catheter Kit Has been oriented to simulator Incentive Spirometer Understands guidelines /expectations for Fluids scenario IV start kit Has accomplished all pre-simulation IV tubing requirements IVPB Tubing All participants understand their assigned IV Pump roles Feeding Pump Has been given time frame expectations Other: Students will need copy of Mini-Cog Pressure Bag 02 delivery device (type) Crash cart with airway devices and emergency medications Defibrillator/Pacer Suction Other: Tissues and a small container/bag for the used tissues Roles/Guidelines for Roles: Primary Nurse Secondary Nurse Clinical Instructor Family Member #1 Family Member #2 Observer/s Recorder Physician/Advanced Practice Nurse Respiratory Therapy Anesthesia Pharmacy Lab Imaging Social Services Important Information Related to Roles: The primary nurse will enter the scenario alone and will call for the second nurse when help is needed. Judy Jones – Simulation # 1 © National League for Nursing, 2014 5 Clergy Unlicensed Assistive Personnel Code Team Other: Report Students Will Receive Before Simulation Time: 1900, 24 hours after admission Situation: Judy Jones is an 85-year-old female patient of Dr. Annette Parks who was admitted yesterday afternoon with a diagnosis of community-acquired pneumonia. She is being treated with IV Azithromycin and IV fluids. Background: Judy Jones has a medical history of hypertension, which is controlled by spironolactone, cervical spondylosis with pain controlled with ibuprofen when needed, hyperlipidemia that is controlled by diet. She also has mild dementia. She hasn’t been confused but is forgetful and easily redirected. She has a history of carpal tunnel surgery on both wrists. Assessment: She is alert and oriented to self, but needs frequent reorientation to place and time. She is forgetful. At 1600 her vital signs were temp 99.9, heart rate 103, respirations 24, BP 130/68, pulse ox 95% on 2 liters of O2 via nasal cannula. Her heart rhythm is regular. She has D5 .45 NSS running at 42 mL/hr into her left forearm. She frequently removes her nasal cannula, and when she does, her pulse ox goes down as low as 90%. Upon auscultation she has rhonchi bilaterally and occasional wheezing. There are PRN respiratory treatments ordered to relieve her wheezing. We are encouraging her to use the incentive spirometer every hour. Ms. Jones is on a regular diet; her appetite is poor. Her abdomen is soft with positive bowel sounds. Her last bowel movement was two days ago and she denies any feelings of constipation at this time. She has been urinating without difficulty in the bathroom, but needs someone’s help to get into the bathroom, basically to manage the IV pole. Her skin looks great. I didn’t see any areas of breakdown, but she is at risk for skin breakdown because she is sitting a lot in the bed. Recommendation: I recommend checking on her frequently due to the forgetfulness and to be sure she keeps her nasal cannula on. It is important that we continually assess her respiratory status. Her last albuterol treatment was at 1200, and she can have her next one whenever she needs it. Be sure to remind and reteach her each time how to use the incentive spirometer; she forgets. Don’t forget we are starting our new Quality Improvement project today. We are doing Mini-Cog assessments three times a week on each patient that scored a 3 or more on the Family Questionnaire for Dementia. You will need to do the Mini-Cog assessment on Ms. Jones before the end of your shift. Judy Jones – Simulation # 1 © National League for Nursing, 2014 6 Significant Lab Values: refer to chart Physician Orders: refer to chart Home Medications: refer to chart Scenario Progression Outline Timing (approx.) 0-5 min Manikin Actions Expected Interventions May Use the Following Cues Manikin or standardized patient is sitting on the floor looking under the bed and saying, “Come on out baby girl . . .it’s OK . . .I’ll help you. It’s time for a snack.” Nasal cannula on bed, oxygen set at 2L. Wash hands and introduce self. Identify patient. Reapply nasal cannula, check oxygen settings. Reorient patient. Call for help to get patient into bed. Role member providing cue: Patient Cue: If the students do not introduce themselves the patient will say, “Who are you? Do you see the children? I haven’t seen you before.” Take vital signs. Assess patient. Role member providing cue: Pulse ox – 88% on room air; increases to 93% after nasal cannula is reapplied. When the nurse reorients Judy, she only remains oriented briefly, then reverts to thinking she is at the day care center. “Come on, Susan, let’s go outside.” Judy cooperates with whatever the nurse instructs her to do but is easily distracted, switching from realizing she is in the hospital to being at the day care. “Does anyone want to go down the slide?” 5-10 min Patient has a productive cough. Judy Jones – Simulation # 1 © National League for Nursing, 2014 7 Temperature: 99.9 F HR: 115 RR: 28 BP: 126/66 Patient Cue: If oxygen is not reapplied patient says, “The person who was here before you kept trying to shove things in my nose.” Pulse ox – 88% on room air; increases to 93% after nasal cannula is reapplied. Lung sounds: Rhonchi with crackles in bases of both lungs. 10-15 min 15-20 min Judy remains focused during the incentive spirometry teaching and uses spirometer correctly. Judy forgets what she is doing several times: “What am I drawing?” Completed clock drawing attached When asked to recall the three words, Judy responds, “Duck, duck, goose.” Teach how to use incentive spirometer. Encourage Judy to use spirometer. Role member providing cue: Patient Cue: If patient is not asked to perform incentive spirometry patient asks, “What is that thing for?” pointing to incentive spirometer. Adminster Mini-Cog TM Give Judy three words to remember. Ask Judy to draw a clock at 11:10. Ask Judy to repeat the three words. After the scenario is completed ask all participants to evaluate the patient using CAM Diagnostic Algorithm available at: http://consultgerirn.org/uploads/File/trythis/try_this_13.pdf Judy Jones – Simulation # 1 © National League for Nursing, 2014 8 Judy’s clock drawing: Debriefing/Guided Reflection Questions for This Simulation (Remember to identify important concepts or curricular threads that are specific to your program) 1. How did you feel throughout the simulation experience? 2. Describe the objectives you were able to achieve. 3. Which ones were you unable to achieve (if any)? 4. Did you have the knowledge and skills to meet objectives? 5. Were you satisfied with your ability to work through the simulation? 6. To Observer: Could the nurses have handled any aspects of the simulation differently? 7. If you were able to do this again, how could you have handled the situation differently? 8. What did the group do well? 9. What did the team feel was the primary nursing diagnosis? 10. How were physical and mental health aspects interrelated in this case? Judy Jones – Simulation # 1 © National League for Nursing, 2014 9 11. What were the key assessments and interventions? 12. Is there anything else you would like to discuss? Specific Debriefing Questions for this Scenario: Assess Function and Expectations: After your initial assessment of Judy, what were your priority interventions? Coordinate and Manage Care: The medications aldactone and ibuprofen are both listed on the Beers Criteria list. How does this affect the coordination and management of care? What was it like to figure out behavioral interventions to address the psychotic behavior? Use Evolving Knowledge: What kind of psychotic behaviors were present? Would these behaviors be part of the client’s dementia or the onset of delirium? To clarify, review/discuss student ratings of Judy on the Confusion Assessment Method (CAM) Diagnostic Algorithm. Make Situational Decisions: What was it like to work with Judy while she was having hallucinations and needing immediate respiratory interventions? Judy Jones – Simulation # 1 © National League for Nursing, 2014 10