Schrag et al.: Risk factors for neonatal sepsis and death in Soweto
advertisement
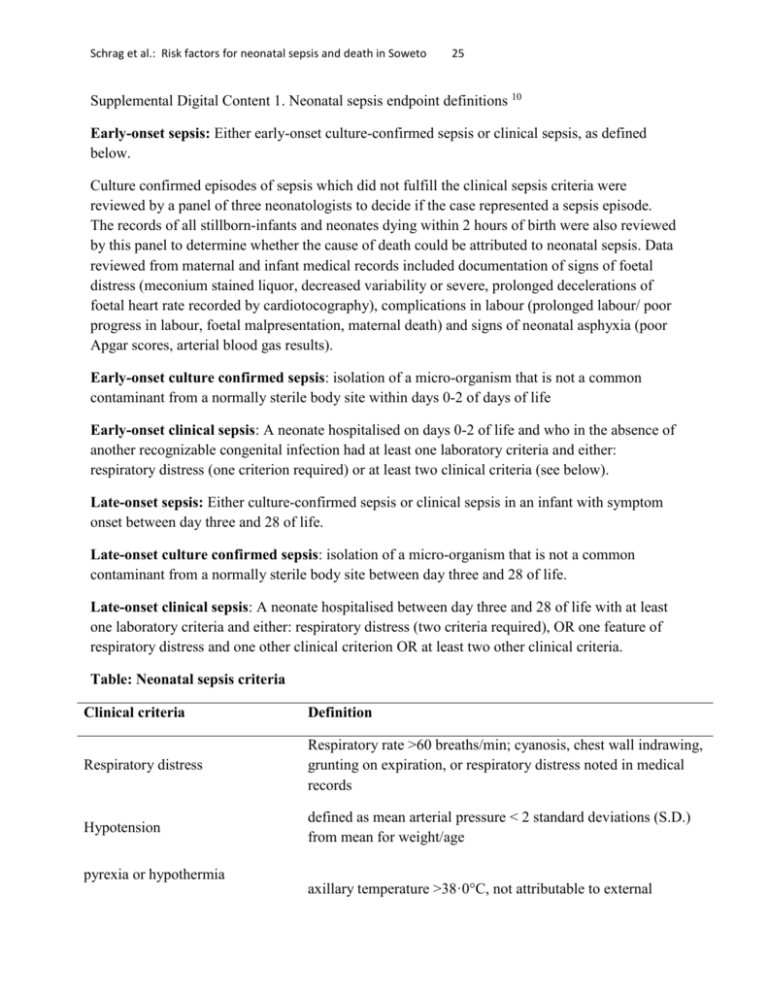
Schrag et al.: Risk factors for neonatal sepsis and death in Soweto 25 Supplemental Digital Content 1. Neonatal sepsis endpoint definitions 10 Early-onset sepsis: Either early-onset culture-confirmed sepsis or clinical sepsis, as defined below. Culture confirmed episodes of sepsis which did not fulfill the clinical sepsis criteria were reviewed by a panel of three neonatologists to decide if the case represented a sepsis episode. The records of all stillborn-infants and neonates dying within 2 hours of birth were also reviewed by this panel to determine whether the cause of death could be attributed to neonatal sepsis. Data reviewed from maternal and infant medical records included documentation of signs of foetal distress (meconium stained liquor, decreased variability or severe, prolonged decelerations of foetal heart rate recorded by cardiotocography), complications in labour (prolonged labour/ poor progress in labour, foetal malpresentation, maternal death) and signs of neonatal asphyxia (poor Apgar scores, arterial blood gas results). Early-onset culture confirmed sepsis: isolation of a micro-organism that is not a common contaminant from a normally sterile body site within days 0-2 of days of life Early-onset clinical sepsis: A neonate hospitalised on days 0-2 of life and who in the absence of another recognizable congenital infection had at least one laboratory criteria and either: respiratory distress (one criterion required) or at least two clinical criteria (see below). Late-onset sepsis: Either culture-confirmed sepsis or clinical sepsis in an infant with symptom onset between day three and 28 of life. Late-onset culture confirmed sepsis: isolation of a micro-organism that is not a common contaminant from a normally sterile body site between day three and 28 of life. Late-onset clinical sepsis: A neonate hospitalised between day three and 28 of life with at least one laboratory criteria and either: respiratory distress (two criteria required), OR one feature of respiratory distress and one other clinical criterion OR at least two other clinical criteria. Table: Neonatal sepsis criteria Clinical criteria Definition Respiratory distress Respiratory rate >60 breaths/min; cyanosis, chest wall indrawing, grunting on expiration, or respiratory distress noted in medical records Hypotension defined as mean arterial pressure < 2 standard deviations (S.D.) from mean for weight/age pyrexia or hypothermia axillary temperature >38·0C, not attributable to external Schrag et al.: Risk factors for neonatal sepsis and death in Soweto 26 warming, or axillary temperature <36·0C Abdominal/ feeding problems Bleeding diathesis abdominal distension OR feeding intolerance (>20% residual over 24 hours), or poor feeding after feeding well, or > 2 episodes of emesis defined as petechiae, ecchymosis, mucous membrane bleeding, pulmonary hemorrhage, or excessive oozing from venipuncture sites Lethargy or irritability noted by medical staff in absence of other central nervous system symptoms Central nervous system seizures, or bulging fontanelle, or single witnessed episode of apnea Laboratory criteria White blood cell count (WCC) WCC <5 x109/l OR >25 x109/l in the absence of receiving corticosteroids; Absolute neutrophil count (ANC) ANC <1·75 x109/l or >15 x109/l Platelet count <150 x109/l C-reactive protein > 10·0 mg/l (early onset sepsis) OR >40mg/l (late-onset sepsis) Elevated CSF white blood cell (WBC) count >30 x106/l WBC in absence of significant red blood cells