Pace 4 - Surrey Care Association
advertisement
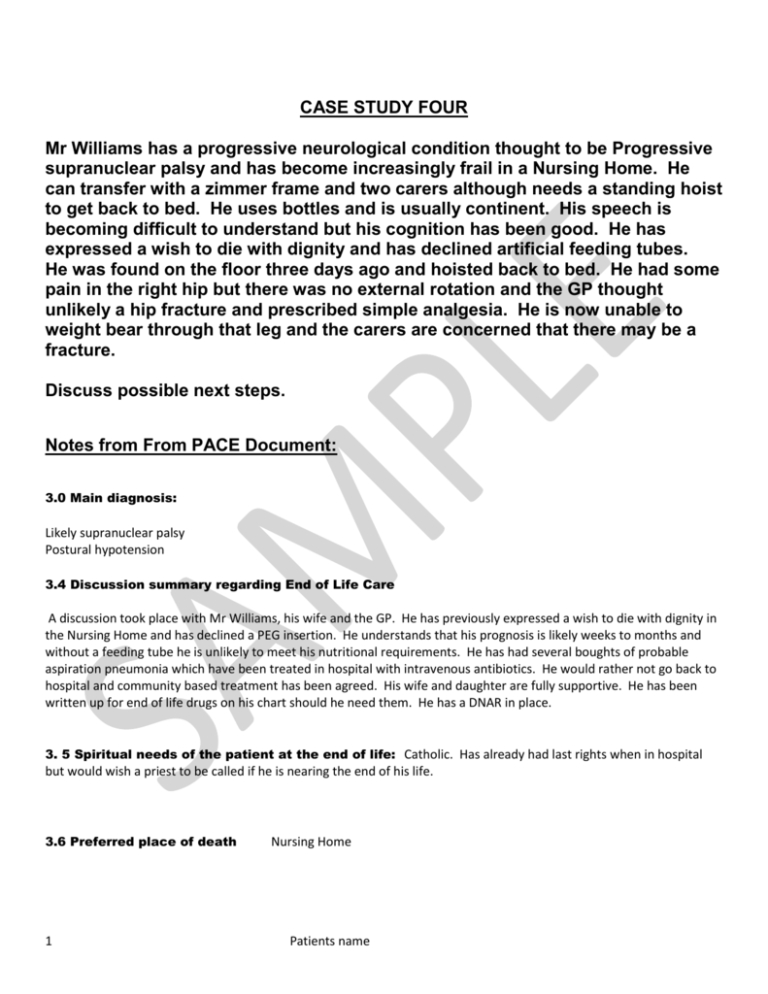
CASE STUDY FOUR Mr Williams has a progressive neurological condition thought to be Progressive supranuclear palsy and has become increasingly frail in a Nursing Home. He can transfer with a zimmer frame and two carers although needs a standing hoist to get back to bed. He uses bottles and is usually continent. His speech is becoming difficult to understand but his cognition has been good. He has expressed a wish to die with dignity and has declined artificial feeding tubes. He was found on the floor three days ago and hoisted back to bed. He had some pain in the right hip but there was no external rotation and the GP thought unlikely a hip fracture and prescribed simple analgesia. He is now unable to weight bear through that leg and the carers are concerned that there may be a fracture. Discuss possible next steps. Notes from From PACE Document: 3.0 Main diagnosis: Likely supranuclear palsy Postural hypotension 3.4 Discussion summary regarding End of Life Care A discussion took place with Mr Williams, his wife and the GP. He has previously expressed a wish to die with dignity in the Nursing Home and has declined a PEG insertion. He understands that his prognosis is likely weeks to months and without a feeding tube he is unlikely to meet his nutritional requirements. He has had several boughts of probable aspiration pneumonia which have been treated in hospital with intravenous antibiotics. He would rather not go back to hospital and community based treatment has been agreed. His wife and daughter are fully supportive. He has been written up for end of life drugs on his chart should he need them. He has a DNAR in place. 3. 5 Spiritual needs of the patient at the end of life: Catholic. Has already had last rights when in hospital but would wish a priest to be called if he is nearing the end of his life. 3.6 Preferred place of death 1 Nursing Home Patients name 4.0 Assessment Possible Developments specific to the person Action Category (see 4.1 below) e.g.“chest infection” (e.g.” Hospital” or “Home”) Comments Please also see supplementary notes for care home staff (appendix 2) 1 Has had recurrent aspiration pneumonia Home If sounding chesty consider glycopyronium to dry up secretions. If feverish may benefit from oral antibiotics. 2 Weight loss, increasing weakness and lethargy Home All part of progressive disease. 3 Coughing when eating / drinking Home Encourage small amounts of pureed diet and snacks regularly. Ideally while sitting up out of bed. review by SALT regarding appropriate thickening of fluids. 4 At risk of pressure sores Home Monitor and ensure appropriate mattress / cushion. 5 Prone to dizziness on standing and has fainted several times. Is on medication to try and prevent further episodes Home Encourage fluid intake. If feels dizzy or looks pale hoist back to bed immediately. If faints in chair, slide to floor and lift up legs. 6 Serious unexpected event eg Fall and broken bone Hospital Hospital assessment and management of pain 7 Patient has no signs of life. Home Has DNAR form in place e.g. “oral antibiotics appropriate” 4.1Action categories Intensive:Transfer to hospital for treatment if appropriate. Intubation, ventilation etc. should be considered. Hospital:Transfer to hospital for treatment if appropriate. Home:Treatment, medication and comfort measures with support from GP. Comfort:Palliative Medication by subcutaneous, oral or per rectal route, positioning, wound care and other measures to relieve suffering. Admission to hospital would be avoided unless comfort measures fail (e.g.: fractured neck of femur). 2 Patients name