Event Reporting - Tenet Healthcare Corporation
advertisement
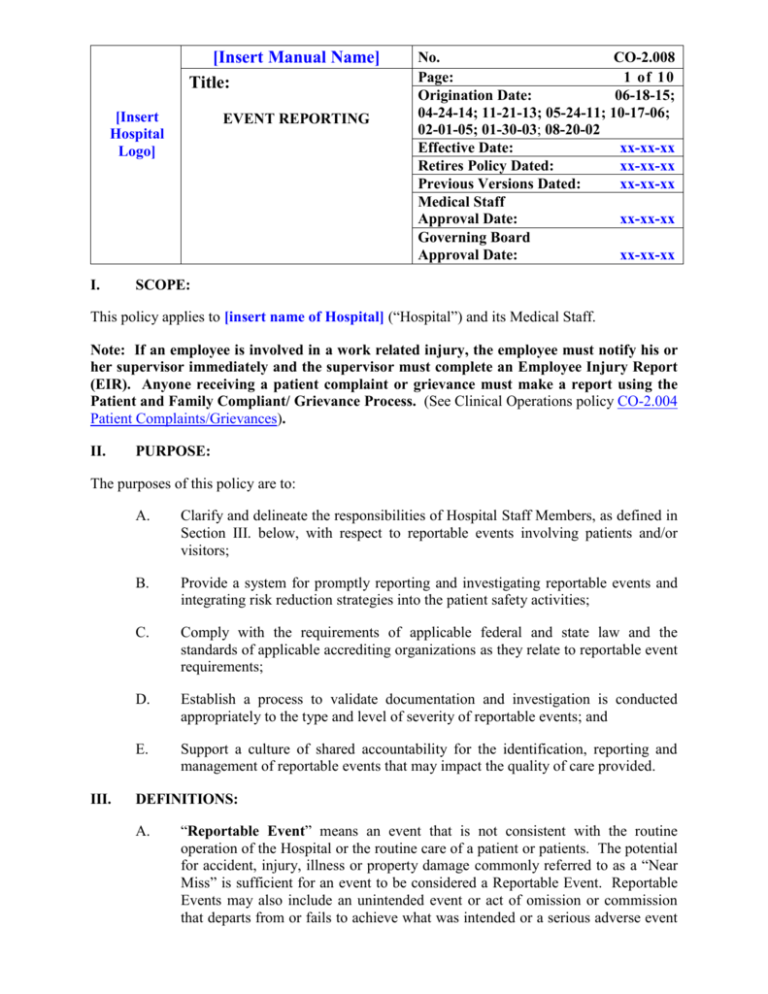
[Insert Manual Name] Title: [Insert Hospital Logo] I. EVENT REPORTING No. CO-2.008 Page: 1 of 10 Origination Date: 06-18-15; 04-24-14; 11-21-13; 05-24-11; 10-17-06; 02-01-05; 01-30-03; 08-20-02 Effective Date: xx-xx-xx Retires Policy Dated: xx-xx-xx Previous Versions Dated: xx-xx-xx Medical Staff Approval Date: xx-xx-xx Governing Board Approval Date: xx-xx-xx SCOPE: This policy applies to [insert name of Hospital] (“Hospital”) and its Medical Staff. Note: If an employee is involved in a work related injury, the employee must notify his or her supervisor immediately and the supervisor must complete an Employee Injury Report (EIR). Anyone receiving a patient complaint or grievance must make a report using the Patient and Family Compliant/ Grievance Process. (See Clinical Operations policy CO-2.004 Patient Complaints/Grievances). II. PURPOSE: The purposes of this policy are to: III. A. Clarify and delineate the responsibilities of Hospital Staff Members, as defined in Section III. below, with respect to reportable events involving patients and/or visitors; B. Provide a system for promptly reporting and investigating reportable events and integrating risk reduction strategies into the patient safety activities; C. Comply with the requirements of applicable federal and state law and the standards of applicable accrediting organizations as they relate to reportable event requirements; D. Establish a process to validate documentation and investigation is conducted appropriately to the type and level of severity of reportable events; and E. Support a culture of shared accountability for the identification, reporting and management of reportable events that may impact the quality of care provided. DEFINITIONS: A. “Reportable Event” means an event that is not consistent with the routine operation of the Hospital or the routine care of a patient or patients. The potential for accident, injury, illness or property damage commonly referred to as a “Near Miss” is sufficient for an event to be considered a Reportable Event. Reportable Events may also include an unintended event or act of omission or commission that departs from or fails to achieve what was intended or a serious adverse event [Insert Manual Name] Title: [Insert Hospital Logo] EVENT REPORTING No. CO-2.008 Page: 2 of 10 Origination Date: 06-18-15; 04-24-14; 11-21-13; 05-24-11; 10-17-06; 02-01-05; 01-30-03; 08-20-02 Effective Date: xx-xx-xx Retires Policy Dated: xx-xx-xx Previous Versions Dated: xx-xx-xx Medical Staff Approval Date: xx-xx-xx Governing Board Approval Date: xx-xx-xx involving research study patients (see Clinical Operations policy CO-2.030 Serious Adverse Events Involving Research Study Patients). Reportable Events may or may not result in negative consequences to the patient. Reportable Events may include a system error, or an individual error of judgment of action or inaction. B. “Patient Safety Reporting System” or “PSRS” is the mechanism for the Hospital Staff Member to complete an Event Report for patient safety events or near misses required under this policy. Methods of reporting include paper reports, such as completion of hospital-specific tools (e.g., incident reports), telephone hotlines, or on-line event reporting through software applications such as “Electronic Safety and Risk Management” or “eSRM” or “Midas.” C. “Hospital Staff Member” means the Hospital’s physicians, employees, agency staff, contractors and volunteers. D. “Near Miss” means an event or situation that could have resulted in harm to a patient but did not, either by chance or through timely intervention. The event was identified and resolved before reaching the patient. E. “Sentinel Event” means an unexpected occurrence involving death or serious physical or psychological injury not related to the natural course of the patient’s illness or underlying condition, or the risk thereof. F. “Event Report” means a confidential, internal electronic, telephonic, or paper submission used for reporting of events for identification of patient safety issues and performance improvement initiatives. This submission is not a part of the medical record. G. “Event Manager” means the role typically assigned to a subject matter expert who is the Hospital’s identified authority on the event type(s) assigned. This individual sees all events of their assigned event type(s) — regardless of where the events occur. Examples include: Directors of Pharmacy as medication event managers; falls champion as falls event manager. [Insert Manual Name] Title: [Insert Hospital Logo] IV. EVENT REPORTING No. CO-2.008 Page: 3 of 10 Origination Date: 06-18-15; 04-24-14; 11-21-13; 05-24-11; 10-17-06; 02-01-05; 01-30-03; 08-20-02 Effective Date: xx-xx-xx Retires Policy Dated: xx-xx-xx Previous Versions Dated: xx-xx-xx Medical Staff Approval Date: xx-xx-xx Governing Board Approval Date: xx-xx-xx POLICY: No Hospital Staff Member may intimidate, threaten, coerce, discriminate against, or take other retaliatory action against any employee or other individual for reporting, in good faith, any Reportable Event as defined in Section III.A. of this policy (see Standards of Conduct). Any Hospital Staff Member who witnesses, discovers or has direct involvement in and/or knowledge of a Reportable Event must complete an Event Report. More than one individual may complete a report concerning the same issue. Members of the Medical Staff may complete an Event Report or request that another Hospital Staff Member with direct knowledge of the event complete the form. All Event Reports must be completed using [insert “eSRM” or “Midas” or information on facility’s designated Patient Safety Reporting System, including hotlines, title of paper tool, or other reporting mechanisms]. [If the facility uses eSRM or Midas, also add this sentence: If the reporter does not have on-line access, please use the [eSRM][Midas] down time form (see Attachment B — [eSRM][Midas] Down Time Form).] All Event Reports are confidential and must not be copied, placed or referenced in the medical record. V. PROCEDURE: A. Time Frame for Completing an Event Report 1. B. After providing for the needs of the individuals involved, Hospital Staff Members must complete and submit an Event Report as soon as possible. Preferably, the report should be submitted before leaving the Hospital at the end of the work shift, but no later than twenty-four (24) hours from the time the event occurred. On occasion, events will be identified through retrospective quality or chart reviews or upon patient presentation (e.g., unintentionally retained foreign object). Report submission of this nature is to occur upon discovery, but no later than twenty-four (24) hours after discovery. Information to Provide in the Event Report 1. When entering an Event Report, Hospital Staff Members should have key information available for completing the report. [Insert Manual Name] Title: [Insert Hospital Logo] EVENT REPORTING 2. No. CO-2.008 Page: 4 of 10 Origination Date: 06-18-15; 04-24-14; 11-21-13; 05-24-11; 10-17-06; 02-01-05; 01-30-03; 08-20-02 Effective Date: xx-xx-xx Retires Policy Dated: xx-xx-xx Previous Versions Dated: xx-xx-xx Medical Staff Approval Date: xx-xx-xx Governing Board Approval Date: xx-xx-xx The Event Report must be limited to factual statements (who, what, where and when) related to the Reportable Event and any interventions taken. The Event Report must not include speculation, admit to or attempt to assign blame, liability or causation or include opinions of any kind. If the individual completing the report desires to discuss additional aspects of the event, that individual can contact the Risk Manager. a. Complete mandatory fields and all relevant fields specific to the event. (Mandatory fields are marked). b. Provide a brief, objective, factual narrative description of the event. Minimize use of abbreviations. c. Review information and submit. d. If the incident is an actual or a potential Sentinel Event, and/or has caused serious injury, immediately institute the Hospital’s chain of command and notify Risk Management and the patient’s attending physician. (See Clinical Operations policy CO-2.010 Sentinel Event Response and Reporting). e. Entries made in the medical record related to the event contain only objective and factual information necessary for continuity of care. If in question of what to document, contact the Risk Manager for guidance. f. Do not reference the Event Report or investigative process in the medical record. (1) The patient’s chart must: (a) Reflect all pertinent medical facts relating to the Reportable Event; (b) Be accurate, legible, and completed timely; and (c) Properly dated and timed. [Insert Manual Name] Title: [Insert Hospital Logo] C. EVENT REPORTING No. CO-2.008 Page: 5 of 10 Origination Date: 06-18-15; 04-24-14; 11-21-13; 05-24-11; 10-17-06; 02-01-05; 01-30-03; 08-20-02 Effective Date: xx-xx-xx Retires Policy Dated: xx-xx-xx Previous Versions Dated: xx-xx-xx Medical Staff Approval Date: xx-xx-xx Governing Board Approval Date: xx-xx-xx Department Director/Manager/Supervisor Responsibilities Each Department Director/Manager/Supervisor is responsible for: D. 1. Reviewing events that occur in their area, assigning severity, documenting the results of the review, and assigning or completing follow-up through the Hospital’s Patient Safety Reporting System; 2. Initiating investigation and follow-up as soon as possible after an Event Report is submitted. In most cases, investigation and follow-up must be completed within seven business days of the time the event is submitted; Hospital Risk Manager or Designee Responsibilities The Hospital’s Risk Manager is responsible for: 1. Providing leadership in all risk event functions/processes and ensuring that all staff is trained on this policy; 2. Full oversight of the PSRS, which includes but is not limited to: a. System administrator duties; b. Daily review of events in the PSRS inbox; c. Data integrity and analysis; (1) The Risk Manager or designee must conduct periodic analysis of all events based on appropriate categorizations (for example: severity, event type, locations and other factors). Focus should be directed to high-risk, problemprone areas/events; (2) Trending and analysis of Reportable Events and Near Misses with communication via proper committee structures; (3) Documenting closure of all reported events from the prior month no later than the eighth calendar day of the [Insert Manual Name] Title: [Insert Hospital Logo] EVENT REPORTING No. CO-2.008 Page: 6 of 10 Origination Date: 06-18-15; 04-24-14; 11-21-13; 05-24-11; 10-17-06; 02-01-05; 01-30-03; 08-20-02 Effective Date: xx-xx-xx Retires Policy Dated: xx-xx-xx Previous Versions Dated: xx-xx-xx Medical Staff Approval Date: xx-xx-xx Governing Board Approval Date: xx-xx-xx following month, with the exception of those events that are under investigation. d. Conducting training at orientation and annual refresher courses as appropriate regarding responsibilities for reporting events; as well as continuing education and training for all current employees; e. Collaborating with Event Managers; f. Reporting serious safety events to the appropriate individuals/ committees. These include, but are not limited to: (1) Hospital Senior Leadership (2) Corporate Patient Safety and Risk Management Department (see Clinical Operations procedure CO2.008.01 for criteria and timeline) (3) Litigation Manager, through the sentinel event reporting (SRE) function (4) Compliance Officer (5) Appropriate Hospital committees g. Notifying Home Office Senior Director of Patient Safety and Clinical Risk Management of any event meeting the serious reportable event criteria within 96 hours of the event being identified with submission of appropriate intense analysis documentation within 14 days of the event date. For cases identified through other mechanisms rather than end user reporting (chart review, etc.), the date of event detection will be used to determine the 14-day time frame for submission of appropriate intense analysis (see Clinical Operations procedure CO-2.008.01 for criteria). h. Review, categorization, final investigation as appropriate for all Event Reports; [Insert Manual Name] Title: [Insert Hospital Logo] EVENT REPORTING No. CO-2.008 Page: 7 of 10 Origination Date: 06-18-15; 04-24-14; 11-21-13; 05-24-11; 10-17-06; 02-01-05; 01-30-03; 08-20-02 Effective Date: xx-xx-xx Retires Policy Dated: xx-xx-xx Previous Versions Dated: xx-xx-xx Medical Staff Approval Date: xx-xx-xx Governing Board Approval Date: xx-xx-xx i. Completion of the Root Cause Analysis/Intense Analysis within 14 days of the Reportable Event for those that meet the definition for Intense Analysis. (See attached Clinical Operations procedure CO-2.010.03 Conducting a Root Cause Analysis). j. Monitoring the status and relationship with the patient and family The Risk Manager is responsible for coordinating the communication and maintaining the relationship with the patient and family during treatment at the Hospital and post-discharge, including but not limited to: E. (1) Review of potential billing adjustments according to the requirements of Regulatory Compliance policy COMPRCC 4.02 Waivers of Co-Payments and Deductibles or other pertinent hospital policies and guidelines. (Refer to Clinical Operations policy CO-2.010 Sentinel Event Response and Reporting, its procedure CO-2.010.04 Bill Hold Process for Possible Preventable Events and Clinical Operations policy CO-2.030 Serious Adverse Events Involving Research Patients). (2) Ensuring the notification to the patient and family per the Hospital patient and family notification policy. (Refer to Clinical Operations procedure CO-2.010.05 Disclosure of Outcomes to Patients). Storage and Retention of Records and Materials The Risk Manager must maintain all Event Records and any addenda and related material in a secured location. The Hospital must retain all Event Reports in accordance with Administrative policy AD 1.11 Records Management and its Record Retention Schedule. F. Confidentiality of Event Reports and Related Data All Event Reports and related material are confidential and may be legally privileged. The Risk Manager must not release or permit the review of Event Reports by any third party (including Hospital committees, the Hospital [Insert Manual Name] Title: [Insert Hospital Logo] EVENT REPORTING No. CO-2.008 Page: 8 of 10 Origination Date: 06-18-15; 04-24-14; 11-21-13; 05-24-11; 10-17-06; 02-01-05; 01-30-03; 08-20-02 Effective Date: xx-xx-xx Retires Policy Dated: xx-xx-xx Previous Versions Dated: xx-xx-xx Medical Staff Approval Date: xx-xx-xx Governing Board Approval Date: xx-xx-xx Governing Board, internal or external agencies), unless authorized by Regional Counsel. Aggregate or summary data may be reported to the Hospital Governing Board, appropriate committees and Hospital management for purposes of performance and patient safety improvement. G. Auditing and Monitoring Performance Standards will audit the Hospital’s compliance with this policy as part of its Comprehensive Clinical Audits. Audit Services will audit the Hospital’s compliance with this policy as part of its routine audits. H. Responsible Person The Risk Manager is responsible for ensuring that all individuals adhere to the requirements of this policy. If the Risk Manager is unable to create adherence to this policy, the Risk Manager must immediately report the non-adherence to the Chief Executive Officer. I. Enforcement All Hospital Staff Members whose responsibilities are affected by this policy are expected to be familiar with the basic procedures and responsibilities created by this policy. Failure to comply with this policy will be subject to appropriate performance management pursuant to all applicable policies and procedures, including the Medical Staff Bylaws, Rules and Regulations. IV. REFERENCES: - CO-2.008.01 Corporate Notification Criteria for Serious Reportable Events - Standards of Conduct - Administrative policy AD 1.11 Records Management and its Record Retention Schedule - Clinical Operations policy CO-2.004 Patient Complaints/Grievances - Clinical Operations policy CO-2.010 Sentinel Event Response and Reporting - Clinical Operations procedure CO-2.010.03 Conducting a Root Cause Analysis (RCA) [Insert Manual Name] Title: [Insert Hospital Logo] EVENT REPORTING No. CO-2.008 Page: 9 of 10 Origination Date: 06-18-15; 04-24-14; 11-21-13; 05-24-11; 10-17-06; 02-01-05; 01-30-03; 08-20-02 Effective Date: xx-xx-xx Retires Policy Dated: xx-xx-xx Previous Versions Dated: xx-xx-xx Medical Staff Approval Date: xx-xx-xx Governing Board Approval Date: xx-xx-xx - Clinical Operations procedure CO-2.010.04 Bill Hold Process for Possible Preventable Events - Clinical Operations procedure CO-2.010.05 Disclosure of Outcomes to Patients - Clinical Operations policy CO-2.030 Serious Adverse Events Involving Research Study Patients - Regulatory Compliance policy COMP-RCC 4.02 Waivers of Co-Payments and Deductibles VI. ATTACHMENTS: - Attachment A – eSRM Severity Codes [Delete if your facility does not use eSRM] - Attachment B – eSRM/Midas Down Time Form [Delete if your facility does not use eSRM or Midas] - CO-2.008.01 Serious Reportable Event Criteria – eSRM/Midas severity/classification crosswalk Attachment A CO-2.008 Event Reporting Page 1 of 1 eSRM Severity Codes Severity Code eSRM Inbox Symbol eSRM definition – adopted from NCCMERP A Near Miss Circumstances or events that have capacity to cause error. B Near Miss An event/error occurred, but the error did not reach the patient. There was no known impact/effect to the patient. C (green) D (blue) E (yellow) F (yellow) G (orange) H (orange) I (red) Δ No Harm Δ Minor Harm Δ Temporary Harm Δ Moderate Harm Δ Major Harm Δ Major Harm Δ Catastrophic Harm An event/error occurred that reached the patient, but DID NOT cause patient harm. An event/error occurred increasing the need for treatment/monitoring, but caused NO harm. An event/error occurred resulting in temporary harm. Intervention to prevent harm or extra monitoring was required, but initial or prolonged hospitalization was not required. An event/error occurred resulting in temporary harm. Intervention to preclude harm or extra monitoring was required AND initial or prolonged hospitalization was required. An event/error occurred that DID NOT require intervention necessary to sustain life BUT contributed to or resulted in permanent patient harm. “Permanent harm” is defined by TJC as an injury in which the patient does not regain their original level of functioning (upon admission to the hospital) within two (2) weeks from the date of the event. An event/error occurred that required intervention necessary to sustain life and caused permanent patient harm. “Permanent harm” is defined by TJC as an injury in which the patient does not regain their original level of functioning (upon admission to the hospital) within two (2) weeks from the date of the event. An event/error occurred that may have contributed to or resulted in the patient’s death. 04-24-14 Attachment B CO-2.008 Event Reporting Page 1 of 3 eSRM Downtime Form [eSRM Users: Forms are Available from Standardized Form Vendor; Insert Form and Delete Midas Form. Non-eSRM Users: Delete this Form] 06-18-15 Attachment A CO-2.008 Event Reporting Page 2 of 3 06-18-15 Attachment A CO-2.008 Event Reporting Page 3 of 3 Midas Downtime Form [Note: Midas Users, Insert Your Facility-Approved Downtime Form and Delete the eSRM Form; Non-Midas Users: Delete this Form] 06-18-15 [Insert Hospital Logo] [Insert Manual Name] Title: SERIOUS REPORTABLE EVENT CRITERIA No. CO-2.008.01 Page: Origination Date: 04-24-14; 11-21-13 Effective Date: Retires Procedure Dated: Previous Versions Dated: 1 of 1 06-18-15; xx-xx-xx xx-xx-xx xx-xx-xx Events for notification include: A. Sentinel Events B. Events resulting in major permanent harm based on severity scoring (eSRM G-I, Midas SSE 1-5, PSE 1 and NME 2). C. For unexpected deaths report those that are-Death: (related to potential medical error) Death: (unknown reason) D. Events referred on RM discretion E. Near miss events that may result in patient(s) significant harm if recurrence (NME2), eSRM A & B F. Actual events that meet NQF Serious Reportable Event Criteria G. Events involving potential allegation of patient abuse H. Serious events involving potential for media inquiry I. Death/Disability to mothers/infants during hospitalization for delivery J. Fires in direct patient care areas K. Death in restraints meeting CMS reporting Criteria L. Drug Diversion (patient safety events that impact patient care) Timeline for event notification: Report an event that meets one of the above criteria to Home Office Senior Director of Patient Safety and Clinical Risk Management using corporate notification functionality within 96 hours of the event being identified and reported at the organizational level (focus in on reporting when events meet criteria, root causes of these events may not be known at the time of reporting). Report Hospital-acquired fall and skin events that meet the above criteria to the Home Office within 7 calendar days of the identification date unless meeting sentinel event criteria.