Primary Care Workforce Development 2/21/12 Advanced Health
advertisement

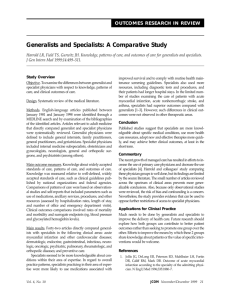
Primary Care Workforce Development Advanced Health Policy 2/21/12 Laura Williams The American primary care workforce is in need of some development to be able to take on the newly insured patients that will be covered by the PPACA’s individual mandate. There is concern that the expanded coverage will cause problems similar to Massachusetts’s experiences with universal coverage that started in 2008; universal coverage doesn’t necessarily equate with universal access if there are not adequate providers. Much of the focus around the primary care workforce has been on primary care physicians. In the US, we have a disproportionate number of specialists compared to other countries of similar economic status: 70% are specialists and 30% are generalists compared to 50-60% generalists in other similar countries (Goodson, 2010). There are many different reasons for this situation, including the following: Less prestige (Lakhan & Laird, 2009) Concerns regarding lifestyle quality (Vaughn et al, 2010) Rising medical school costs and subsequent debt (Vaughn et al, 2010) Reimbursement structure: Fee-for-service model provides better reimbursement for specialists who are procedurally oriented (Goodson, 2010). Primary care physicians spend more time doing un-reimbursable activities and their compensation is 30-60% less than specialists (Goodson, 2010). More familiarity and experience with specialists than generalists through medical school education (Rieselbach et al., 2009). There are different perspectives—some complementary and some disparate—on how to bolster the primary care workforce. Start by reading this article written by the Center for American Progress that provides a nice summary of the situation: http://www.americanprogress.org/issues/2009/11/primary_care_shortage.html Based on this article and other sources I read, there seem to be three main schools of thought regarding how to address primary care shortages. Please pick 2-3 of the following four articles to read (you’re welcome to read all the articles if you’d like, but I didn’t want to overload you!): 1. Alter the way we pay physicians and the generalist-specialist ratio will correct itself This is a definite possibility with arguments for different reimbursement models and pay reform (Berenson & Rich, 2010); however, this discussion is for another day. Since we are talking about the healthcare workforce this week, we will focus our attention on the next two perspectives. 2. Alter the way we recruit and train doctors/incentivize them into primary care Lakhan SE & Laird C. (2009). Addressing the primary care physician shortage in an evolving medical workforce. International Archives of Medicine 2(14). Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2686687/ Rieselbach RE, Crouse BJ, & Frohna JG. (2009). Teaching primary care in community health centers: Addressing the workforce crisis for the underserved. Annals of Internal Medicine 152:118-122. Retrieved from http://www.annals.org/content/152/2/118.full Primary Care Workforce Development Advanced Health Policy 2/21/12 3. Look beyond the doctors and find other providers that can do the same job Naylor MD & Kurtzman ET. (2010). The role of nurse practitioners in reinventing primary care. Health Affairs 29(5):893-899. **article is attached** Jacobson PD & Jazowski SA. (2011). Physicians, the Affordable Care Act, and primary care: Disruptive change or business as usual. Journal of General Internal Medicine 26(8):934-937. **article is attached** Discussion questions: 1. What are some of your favorite solutions presented? What seems more feasible? Less feasible? 2. Perspective #2 provides a more incremental problem-solving type solution to the primary care shortage while perspective #3 takes a more “enlightenment information” route. How should each of these perspectives be prioritized as we allocate money and efforts toward developing the primary care workforce? Consider solutions for both the short and long term. 3. The success of perspective #3 will take significant ideological changes to the current thinking in medicine. Lakhan & Laird (2009) point out that “minds are often harder to change than policies” (p.2). How can we overcome physician reluctance to expanding nurse practitioners’ and physician assistants’ scope of practice and create buy in among the professional medical associations? Additional references cited: Berenson RA & Rich EC. (2010). US approaches to physician payment: The deconstruction of primary care. Journal of General Internal Medicine 25(6):613-618. Goodson JD. (2010). Patient Protection and Affordable Care Act: Promise and peril for primary care. Annals of Internal Medicine 152:742-744. Vaughn BT, DeVrieze SR, Reed SD, & Schulman KA. (2010). Can we close the income and wealth gap between specialists and primary care physicians? Health Affairs 29(5):933-940.